JVP
Notes
Introduction
Examination of the jugular venous pressure provides an estimate of the central venous pressure.
Assessment of the jugular venous pressure (JVP) is a normal component of the cardiovascular examination. It is commonly used to help determine a patients’ fluid balance (i.e. do they have too much or too little fluid in the body). This is because the JVP can be used as an indirect marker of central venous pressure (CVP), which is a measure of pressure within the vena cava.
The term jugular venous pulse is often used synonymously with jugular venous pressure.
To determine the JVP, we have to visualise the jugular veins in the neck. The jugular veins connect to the right atrium of the heart via the superior vena cava. There are two main assessments to make when visualising the jugular veins:
- JVP height: the height of the column of blood within the jugular veins. Reflects right atrial pressure (RAP) that gives an indication for central venous pressure (CVP). CVP is commonly elevated in patients with heart failure.
- JVP waveform: refers to a tracing of the pressure within the internal jugular vein due to alteration in pressure in the right side of the heart during the cardiac cycle. Seen clinically as a ‘venous pulse’ with double movement.
Central venous pressure
Venous pressure refers to the average blood pressure within the venous system.
CVP refers to pressure within the thoracic vena cava near the right atrium. Due to the close proximity, right atrial pressure is a good approximation for CVP. The normal CVP is ~1-8 mmHg (mean 4 mmHg).
CVP can be used as a surrogate marker of preload of the right ventricle, which is the end-diastole volume (i.e. the amount of blood left in the heart at the end of diastole). Thus, increases in preload like seen in congestive heart failure will lead to an elevation in the CVP.
Clinically, alterations to the CVP may be reflected by changes to the JVP, which is why it forms part of the clinical examination. The jugular veins can act as a reservoir of venous blood in continuity with the right atrium. Therefore, changes in pressure in the CVP alter the distension and height of the JVP.
Jugular veins
The jugular veins return blood from the brain, face and neck to the right side of the heart.
The jugular veins are a series of vessels that are important for returning blood from the brain, face, and neck to the right atrium of the heart via the superior vena cava (SVC). The two principal veins are:
- Internal jugular vein (IJV): exits the skull at the jugular foramen and runs within the carotid sheath deep to the strap muscle of the neck (i.e. sternocleidomastoid). Joins the subclavian vein to form the brachiocephalic vein at the base of the neck that enters the SVC.
- External jugular vein (EJV): formed by two joining veins at the posterior angle of the mandible. The vein then runs obliquely across the sternocleidomastoid and drains into the subclavian vein.
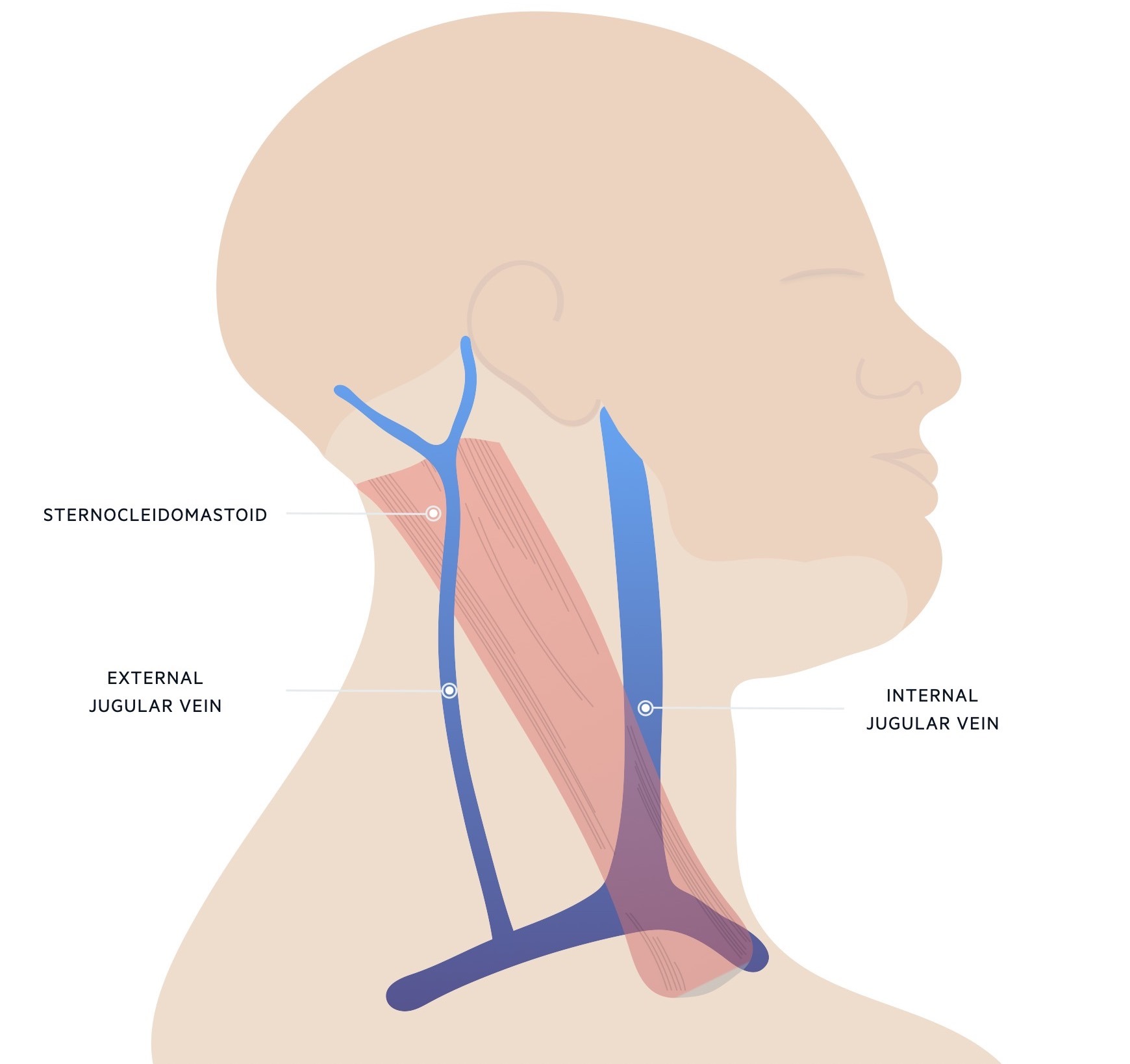
There are some functional valves that exist between the SVC and both the internal and external jugular veins. However, both veins can be used as an estimation of CVP because pressure can be exerted through these valves.
The IJV is a better marker of CVP because of its relatively straight path towards the right atrium. The EJV has to take two sharp angles during its course which makes it less reliable.
Examination of the JVP
Examination of the JVP should be conducted with the patient supine at a 45º angle.
Assessment of the JVP can be very challenging in clinical practice. It takes time and practice, so don’t be disheartened if you’re unable to do it straight away.
Set-up
Traditionally, the right IJV should be assessed from the right-hand side of the bed. Therefore, the patient needs to be placed in the correct position.
- The patient should be lying supine at a 45º angle
- The neck should be extended with the sternocleidomastoid muscles relaxed
- Ask the patient to turn their head slightly to the left
Identify the IJV
Try to visualise the right IJV that will be located between the ear lobe and the medial end of the clavicle. It may be visible just above the clavicle between the two heads of the sternocleidomastoid. In a very elevated JVP, the venous pulsation may cause the lower part of the ear lobe to pulsate or wiggle.
A light source (e.g. pen torch, bedside lamp) may be used to shine light across the neck to improve visualisation. This should be tangential (i.e. light shone on an object at a very low angle).
Measurement of JVP
Assessment of the height of the column of blood within the IJV gives us the JVP height. This measurement is combined with the distance from the mid-right atrium to the sternal angle:
- JVP height: length (cm) of the jugular venous column above the sternal angle
- Right atrium to sternal angle (5 cm)
The combination of these two measurements gives an estimation of right atrial pressure (JVP height + 5 cm). In healthy individuals, the JVP height should be < 3cm when lying in a 45º supine position.
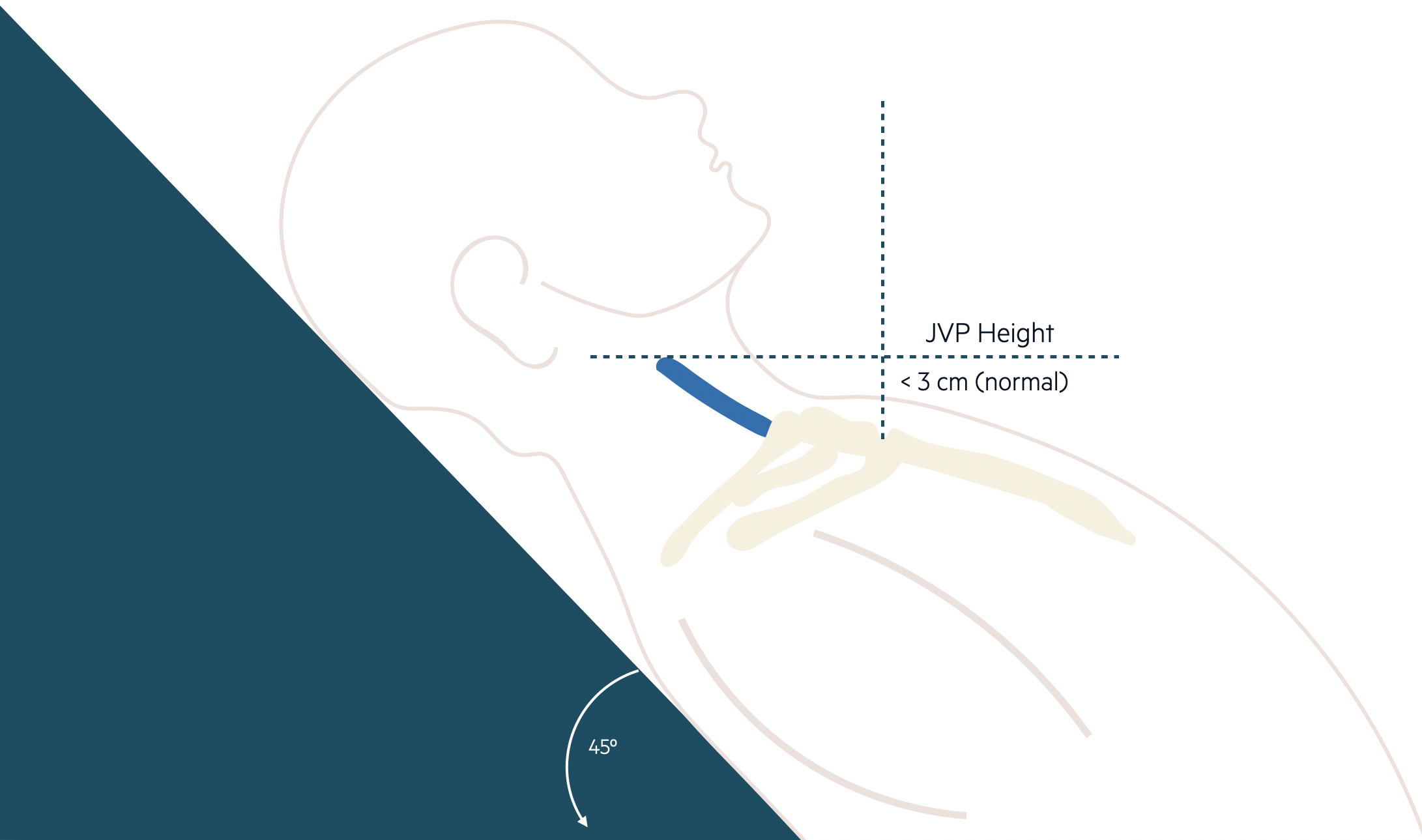
Measurement of the JVP
Differentiating venous and arterial pulsation
The jugular venous pulse has a characteristic double pulsation within the neck. However, it can be difficult to differentiate this from the arterial pulsation of the carotid artery. The following features help differentiate the two pulses:
- Number of pulsations: the JVP has two pulsations, whereas the carotid has one
- Effect with inspiration: the JVP will fall on inspiration. The carotid is unaffected
- Compression: the JVP pulsation will cease if the base of the neck is compressed. The carotid is unaffected
- Hepatojugular reflux (see below): the JVP pulsation may increase on abdominal palpation. The carotid is unaffected
- Palpation: JVP pulsation is not easily palpable, whereas the carotid pulse is easily felt
Using the EJV
When it is difficult to visualise the IJVs (right or left), the EJV may be used to estimate the JVP but it is less reliable. This is because it is not in direct line with the right atrium and two tight angulations.
Assessment of the EJV
- Compress lower EJV: place a finger just above the clavicle to compress the lower EJV
- Time to distend: allow a short time for the vein to distend from above (due to draining blood)
- Compress upper EJV: place a second finger to compress the EJV superiorly
- Release: release the first finger that is situated just above the clavicle
- Assess column height: the venous pressure can now be measured as the best reflection of right atrial pressure
Raised JVP
An elevation in the JVP height is an indication of heart failure.
The main abnormality that can be elicited from the JVP is an increase in height known as a ‘raised’ or ‘elevated’ JVP. A raised JVP usually indicates a rise in right atrial pressure (e.g. heart failure) but may also be seen when there is an obstruction to flow (e.g. superior vena cava obstruction).
Causes of a raised JVP include:
- Right ventricular failure: most commonly due to left-sided heart failure or chronic lung disease
- Abnormal right atrial/ventricular filling: pulmonary hypertension, constrictive pericarditis
- Right-sided valve disease: tricuspid regurgitation or stenosis
- Fluid overload state: secondary to renal disease or liver disease
- Obstruction: tumour or thrombosis within or adjacent to the superior vena cava
Kussmaul’s sign
Normally, the JVP will fall (move downwards towards the neck) with inspiration due to a reduction in intrathoracic pressure. The absence in this normal fall, or a paradoxical rise in the JVP, is known as Kussmaul’s sign. This may be seen in a variety of conditions but is commonly observed in constrictive pericarditis or a large pericardial effusion.
Hepatojugular reflux
Firm pressure over the right upper quadrant transiently increases the JVP in healthy individuals.
The hepatojugular reflux is a clinical test that can be used to help elucidate the JVP.
The test involves applying firm pressure over the right upper quadrant of the abdomen for 10 seconds. During the manoeuvre the IJV should be observed. Compression increases venous return that causes a temporary rise in the JVP for 2-3 beats.
The test is considered abnormal if the JVP remains elevated during at least 10 seconds of compression. This may be seen with conditions causing elevated pulmonary pressure (e.g. heart failure).
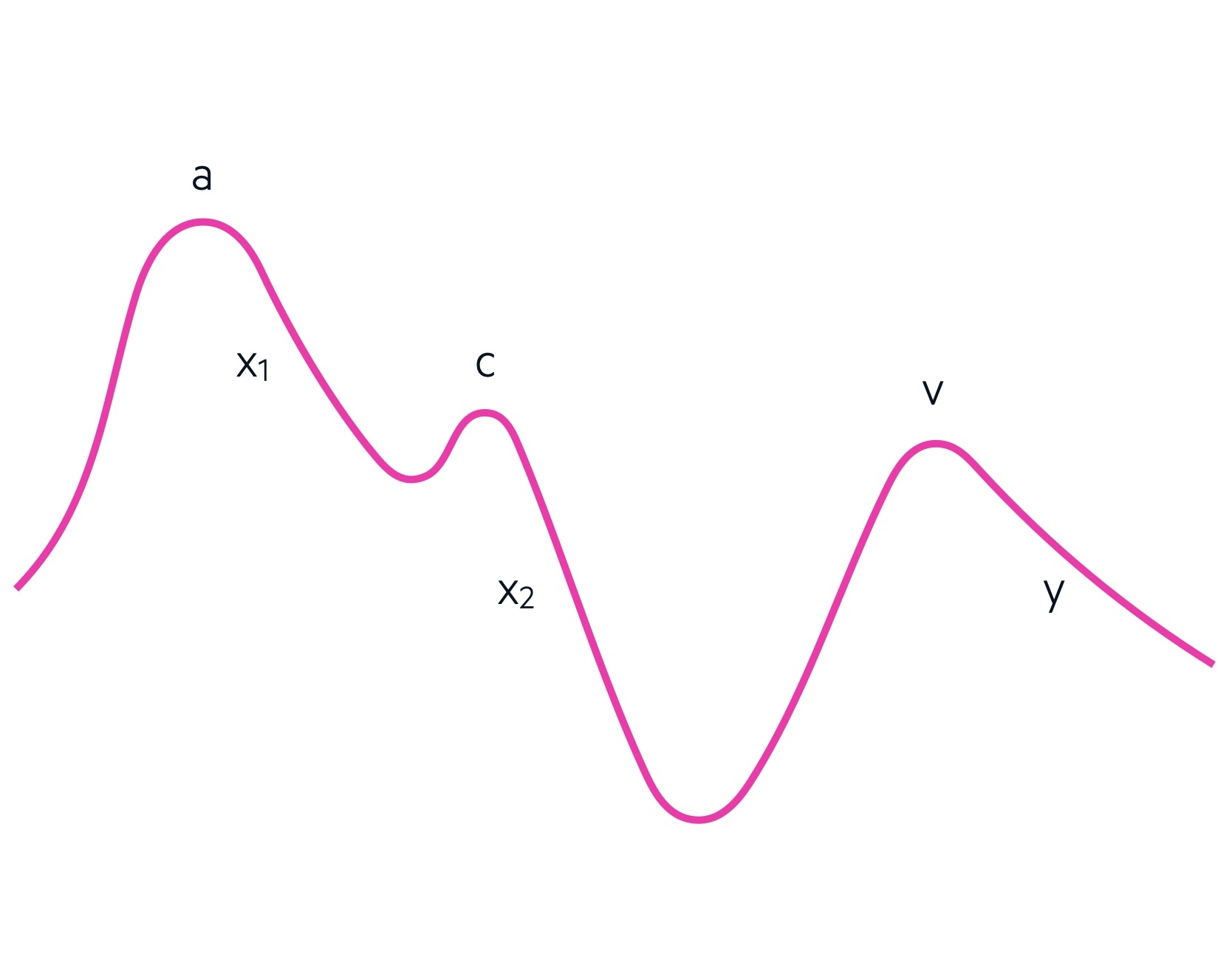
JVP waveforms
The JVP has a characteristic waveform that reflects pressures in the right heart during the cardiac cycle.
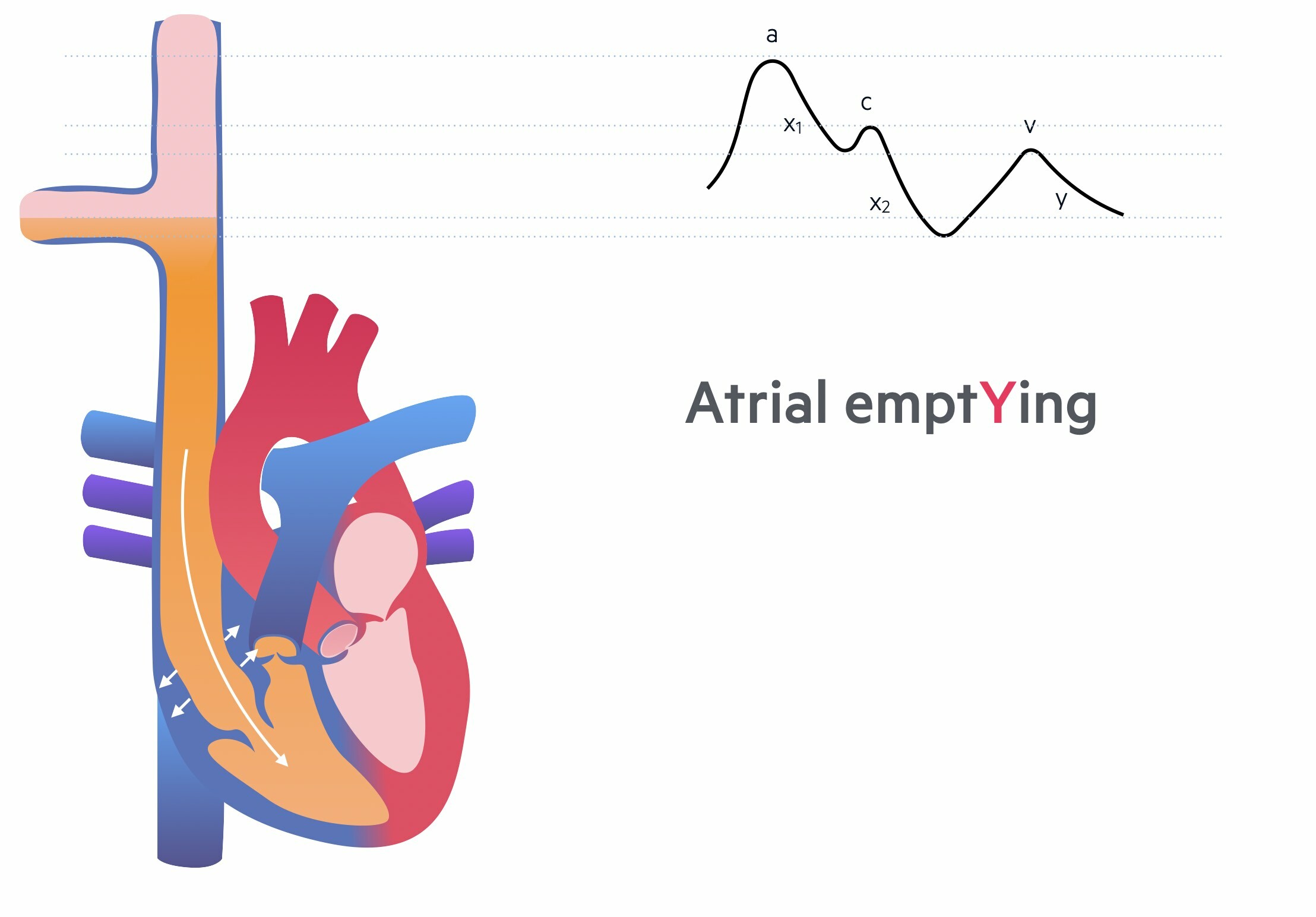
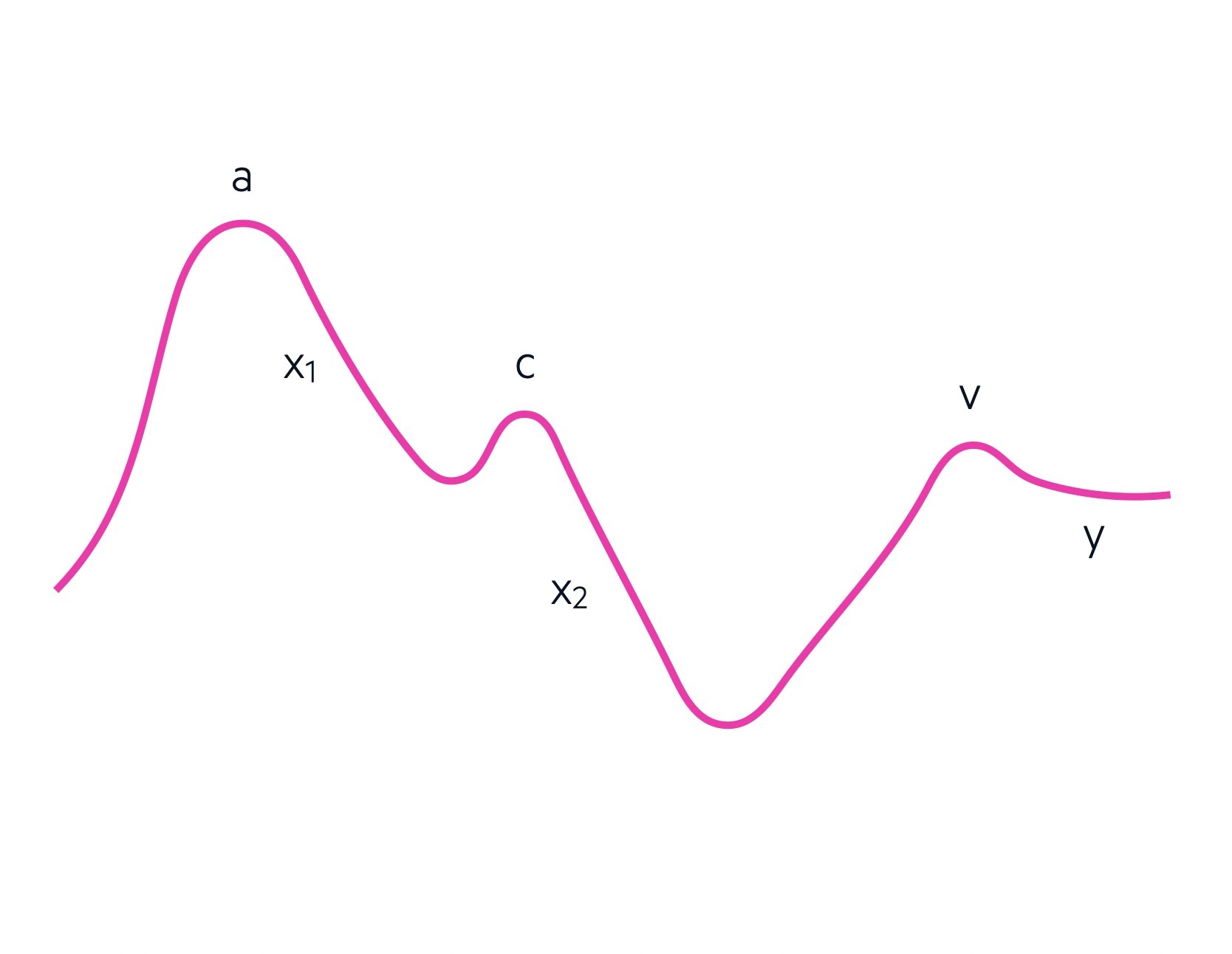
The JVP waveform is divided into 5 characteristic components with three accents (upstrokes) and two descents (downstrokes):
- a wave: Atrial contraction
- X1 descent: relaXation of the atrium and closure of the tricuspid valve
- c wave: ventricular Contraction and bulging of the tricuspid valve
- X2 descent: due to eXtra space within the pericardium to allow atrial filling
- v wave: increase in Volume of the right atrium due to filling
- y descent: emptYing of the right atrium with tricuspid valve opening
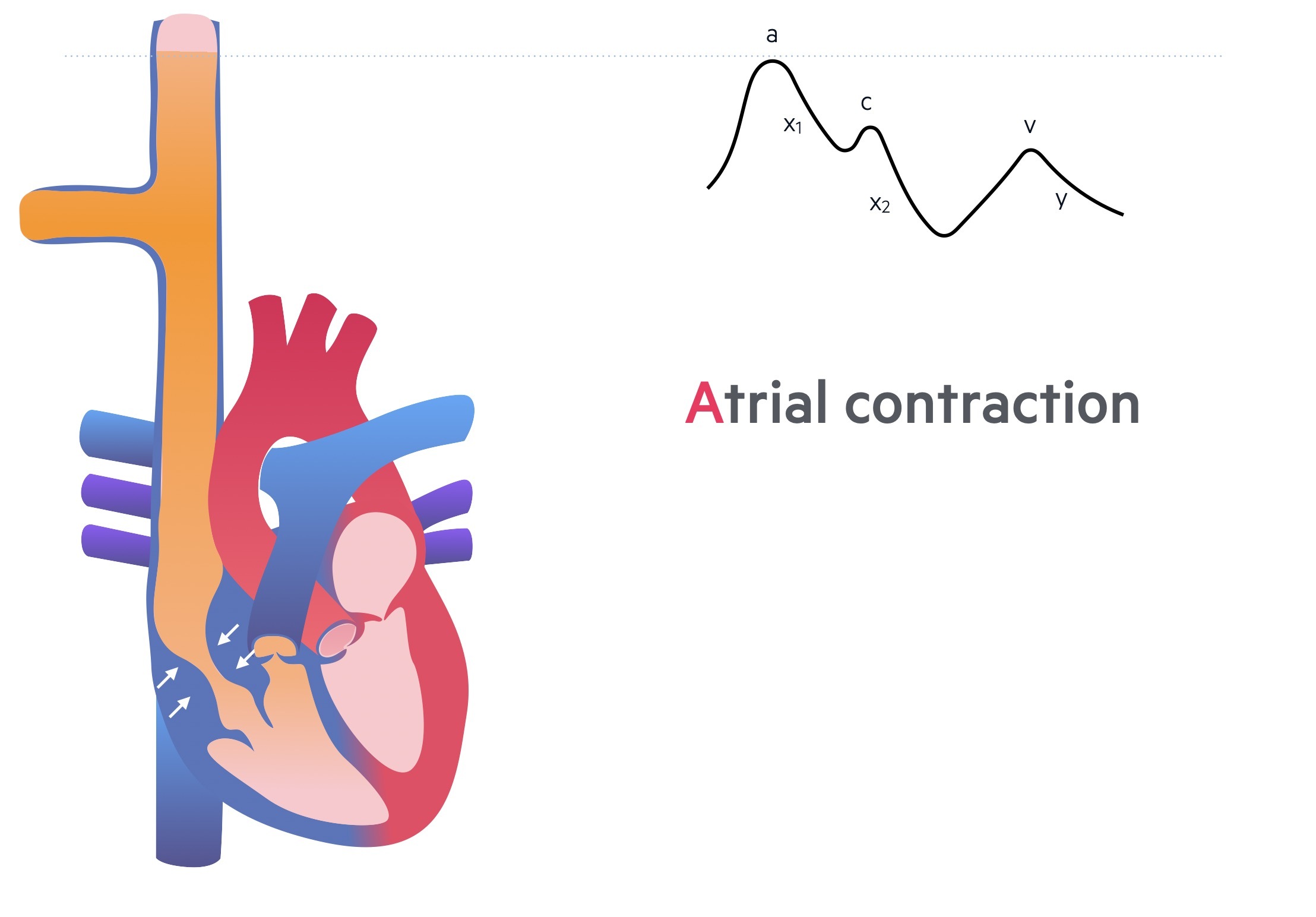
a wave
This is the initial accent of the JVP waveform that occurs due to atrial contraction. Blood is forced from the right atrium across the tricuspid valve into the right ventricle. Increased right atrial pressure causes a temporary pulsation in the JVP.
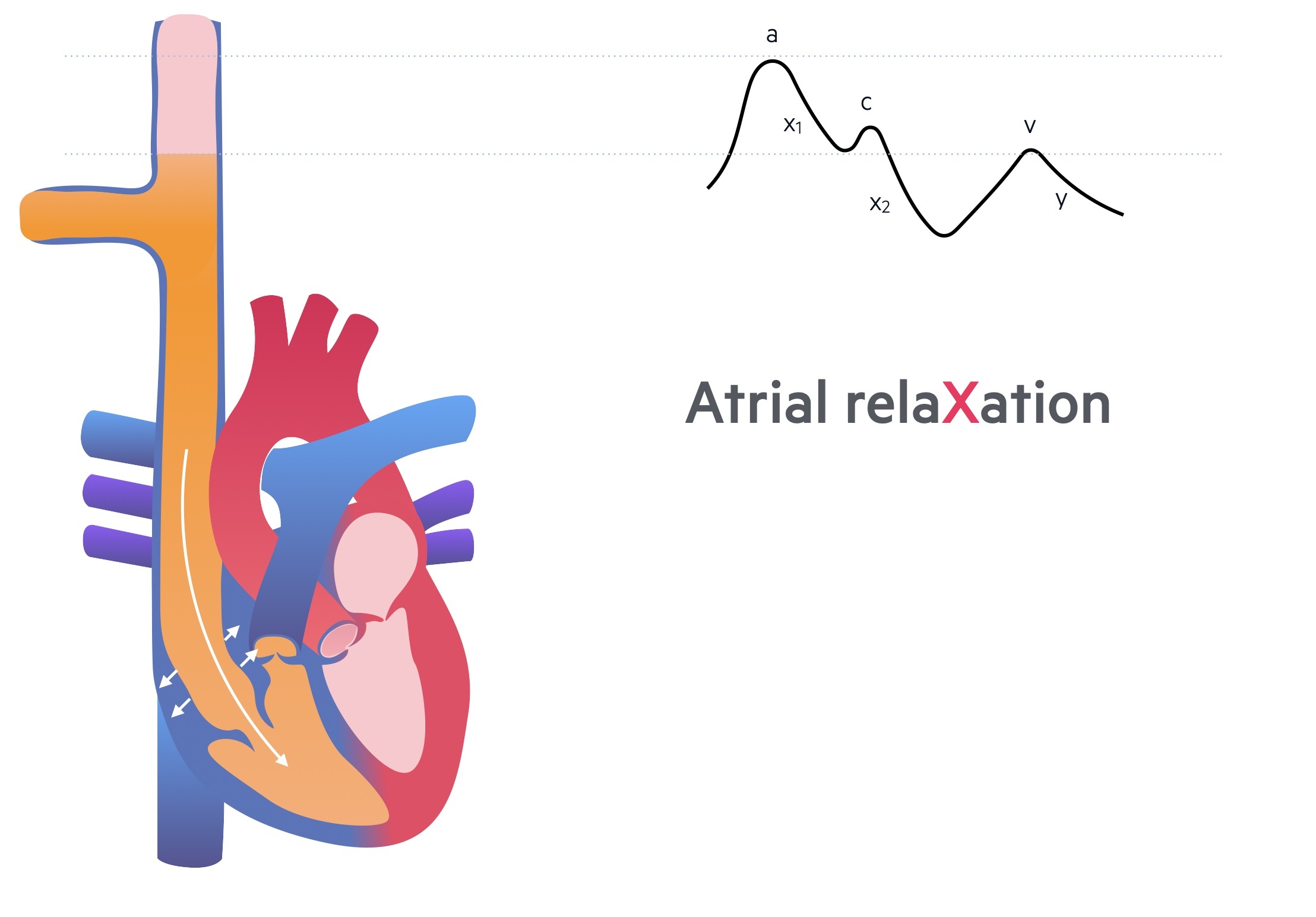
x1 descent
The x descent is divided into two parts. The first x descent occurs due to relaxation of the right atrium following atrial contraction that allows blood to fill from the superior vena cava.
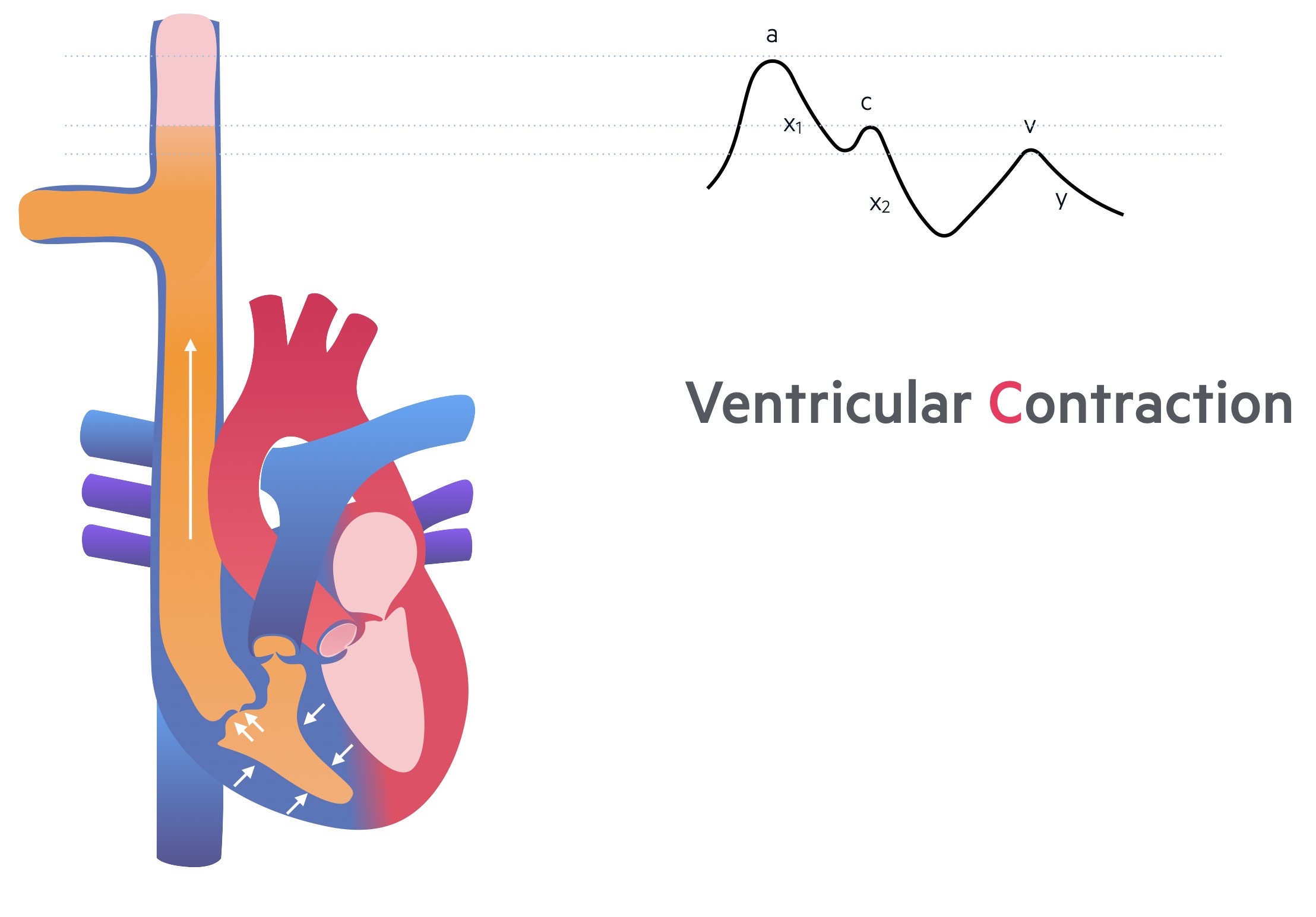
c wave
Forceful contraction of the right ventricle leads to upward motion on the tricuspid valve that bulges into the right atrium. This increases pressure within the right atrium and the force is transmitted into the superior vena cava to form the c wave.
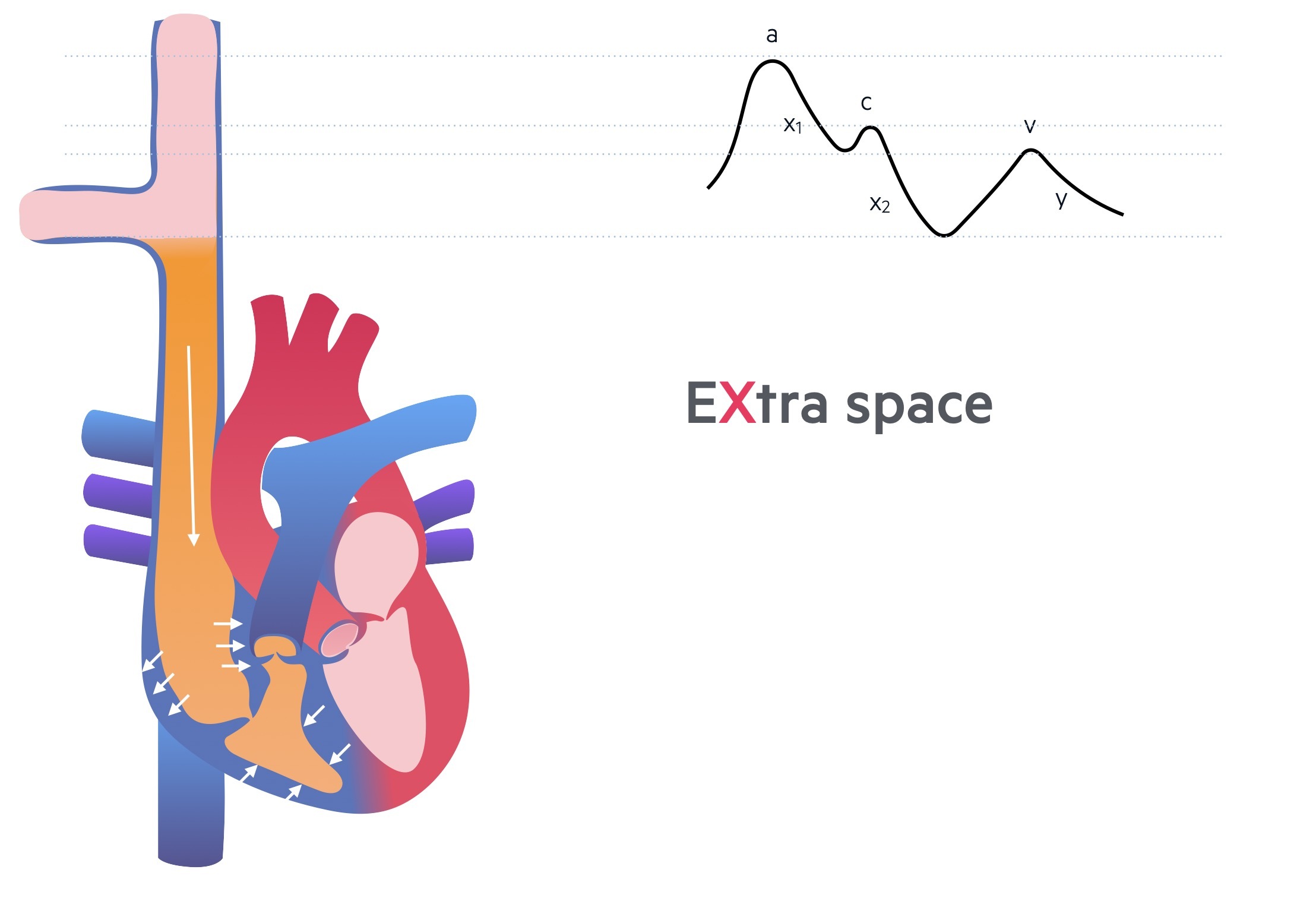
x2 descent
The second X descent is perhaps the hardest to conceptualise. As the right ventricle contracts, it actually takes up less space that leads to increased space within the pericardium. This enables the right atrium to expand and fill with blood, which is initially seen as a fall in right atrial pressure.
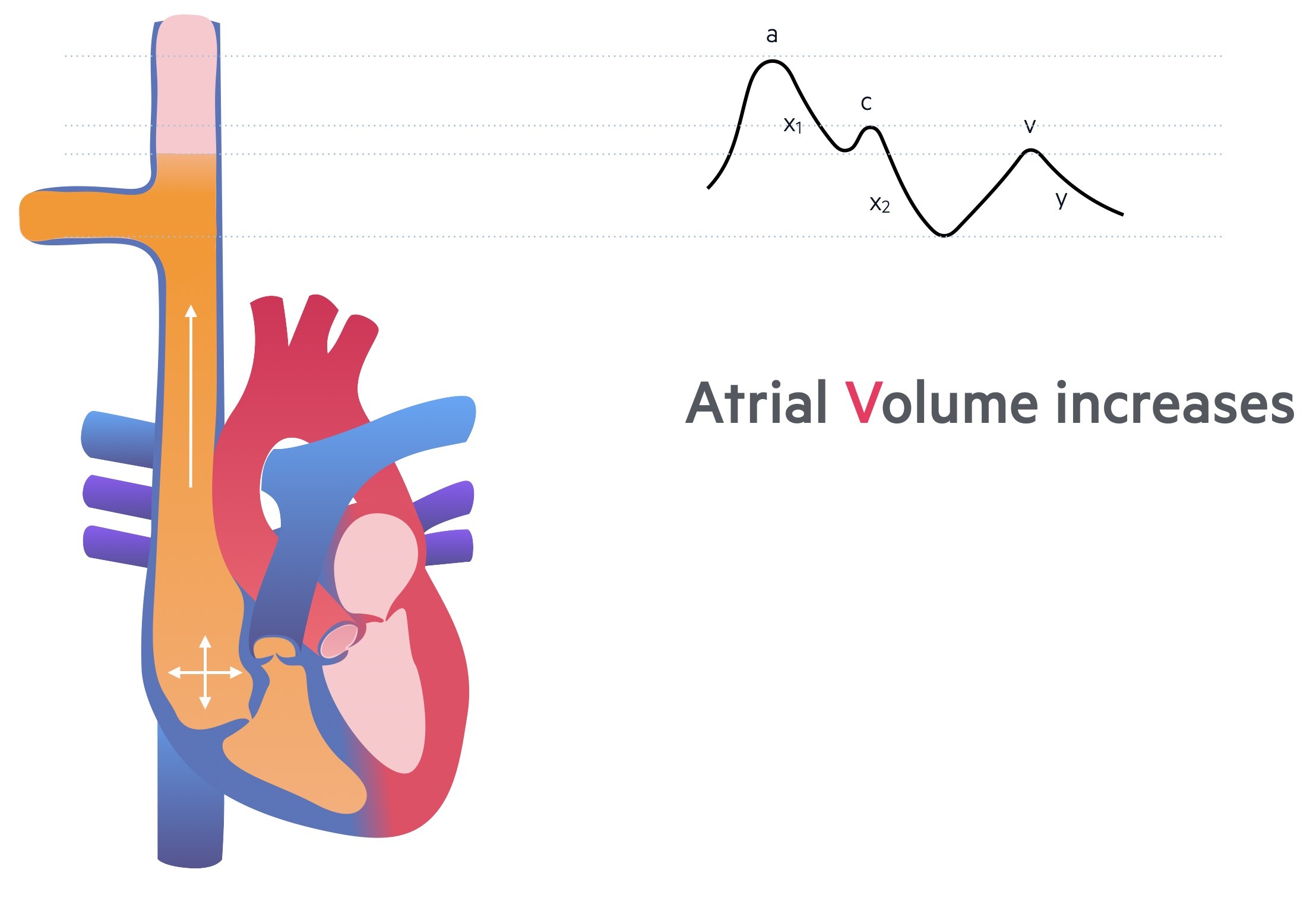
v wave
The right atrium continues to fill with blood against a closed tricuspid valve. As this occurs, the pressure within the right atrium slowly increases and the maximum pressure obtained from filling is see as the v wave.
y descent
The final component is the y descent that reflects tricuspid valve opening. This allow rapid ventricular filling prior to the onset of right atrial contraction.
Waveform abnormalities
Several characteristic abnormalities are seen in the JVP waveform.
A variety of JVP waveform abnormalities may be seen due to disruption of the normal pressure changes that occur within the right side of the heart during the cardiac cycle
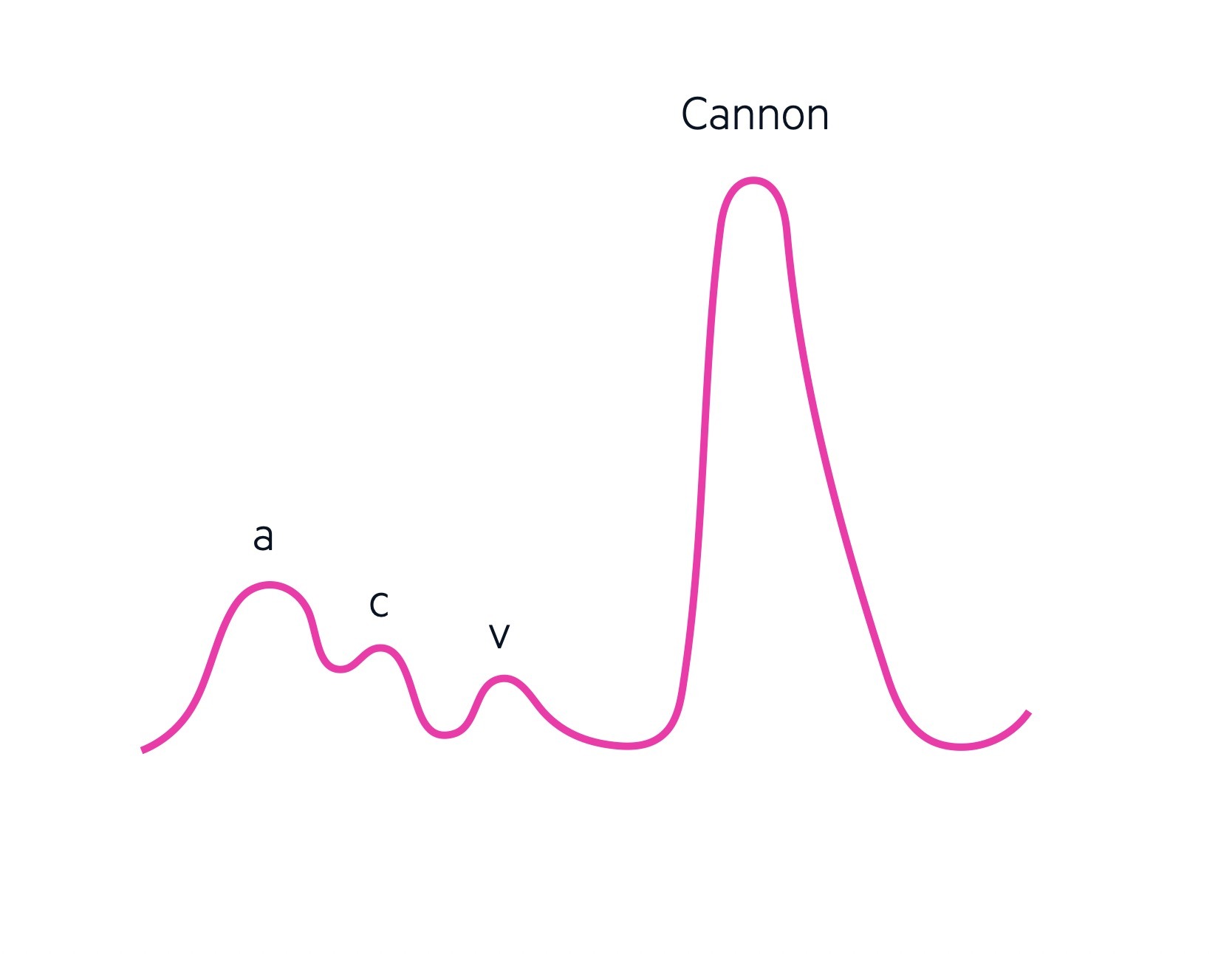
Cannon wave
A 'cannon', 'giant' or 'large' A wave is seen when there is simultaneous atrial and ventricular activation leading to contraction of the right atrium against a closed tricuspid valve. This leads to a sharp, and pronounced, elevation in the JVP pressure. They occur due to rhythmic dissociation between atria and ventricles (e.g. complete heart block, ventricular tachycardia).
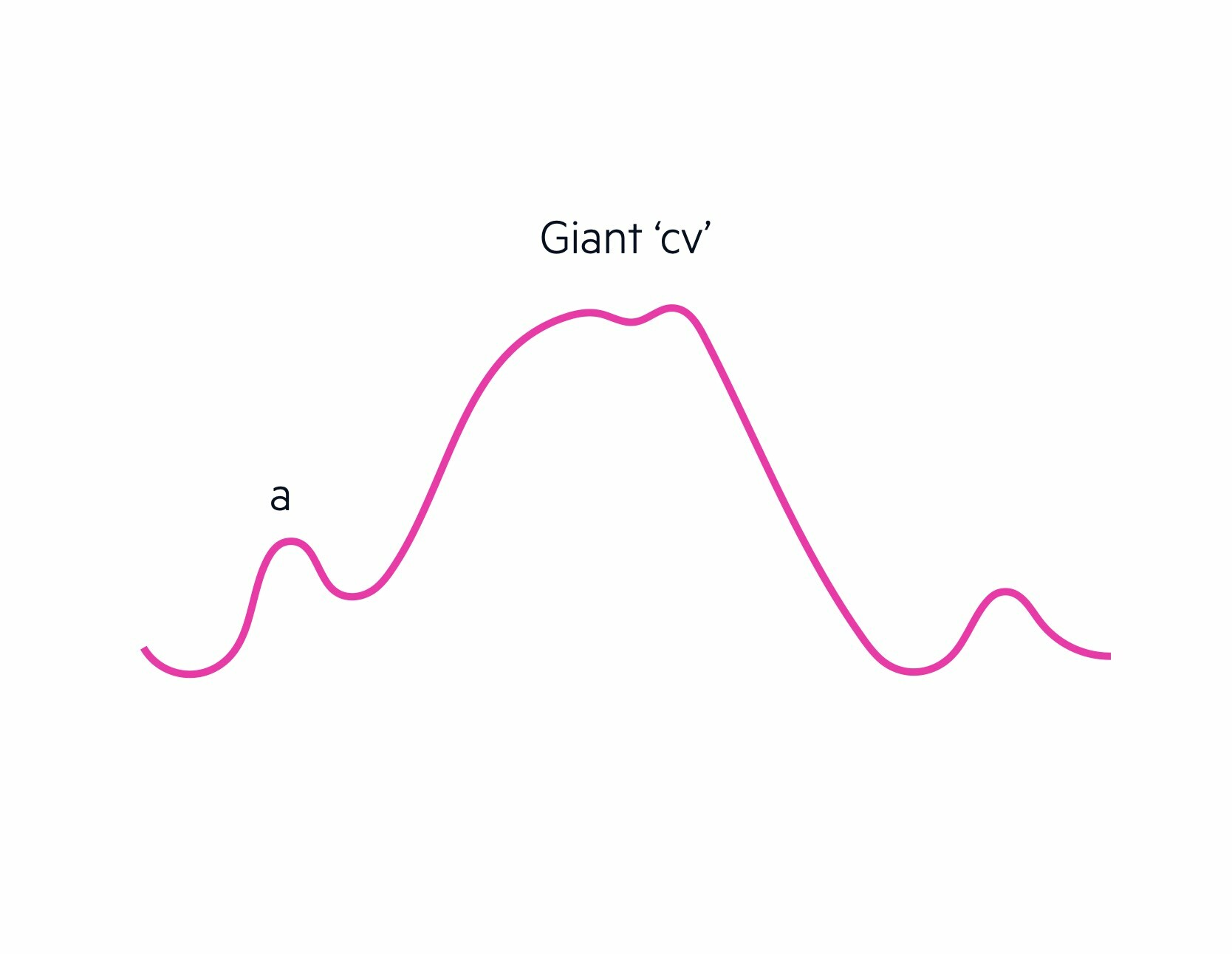
Giant ‘cv’ waves
Giant ‘cv’ waves or tall ‘v’ waves are due to tricuspid regurgitation. Blood regurgitates through the tricuspid valve during ventricular systole (i.e. when the right ventricle contacts). If severe, the c wave obliterates the v wave leading to the term ‘cv’ wave.
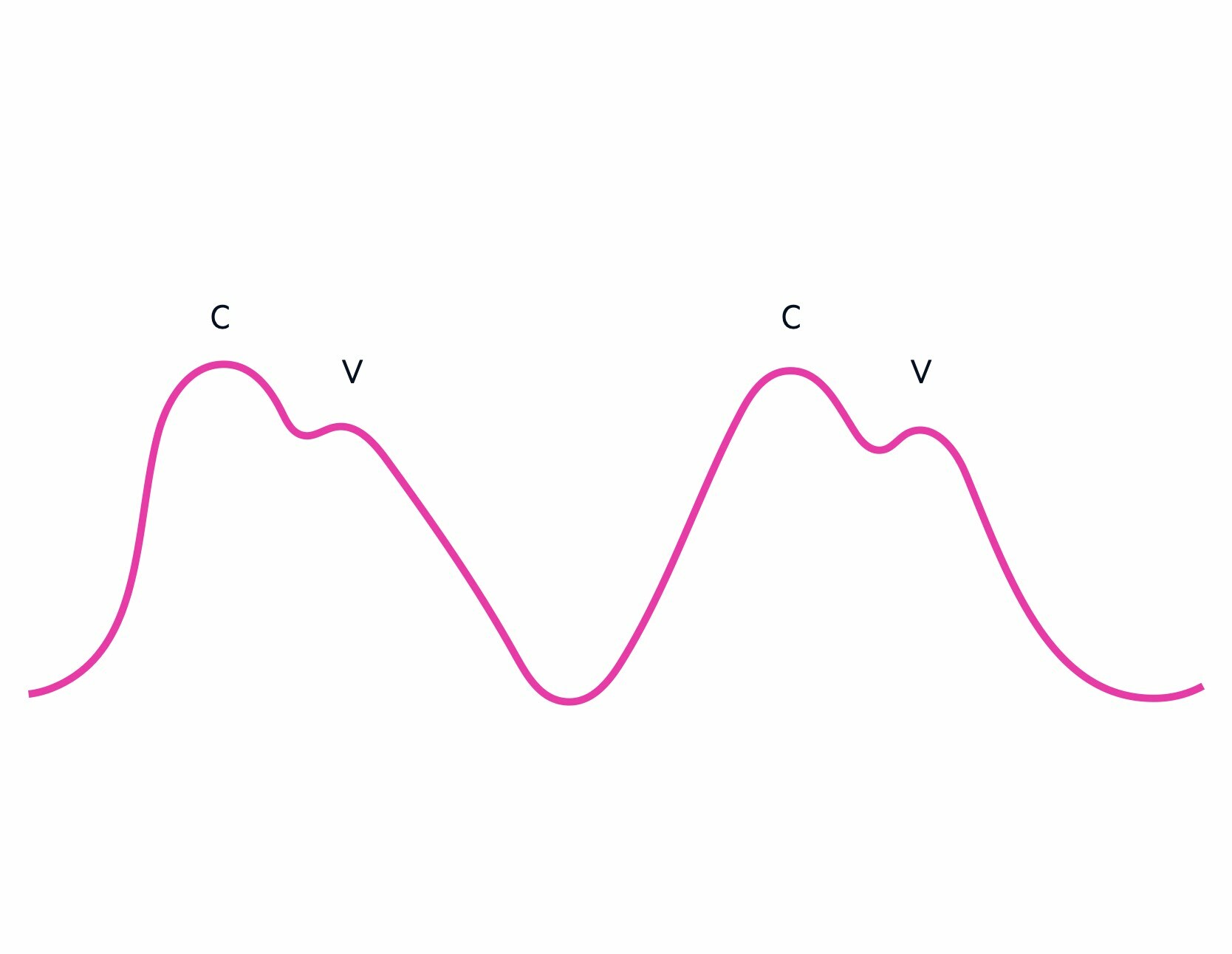
Absent a waves
The a wave represents atrial contraction. Therefore, in conditions such as atrial fibrillation when there is rapid, chaotic, atrial firing these waves are absent.
Slow y descent
When filling of the right ventricle is impaired following the opening of the tricuspid valve, this may lead to a slow or absent y descent. Examples include tricuspid stenosis or pericardial tamponade because there is equalisation of pressure across all chambers.
Last updated: May 2022
Have comments about these notes? Leave us feedback
