5. Bradycardias
Notes
Introduction
Bradycardia refers to an abnormally slow heart rate.
Bradycardia is usually defined an abnormally slow heart rate less than 60 bpm. We refer to all the abnormally slow heart rhythms as bradyarrhythmias.
Bradyarrhythmias may develop due to a variety of intrinsic or extrinsic factors.
Intrinsic
Within the heart, a slow rate may occur due to failure to initiate, or transmit, electrical activity.
Failure to initiate electrical activity can cause another part of the heart to take over as the primary pacemaker. This is called an escape rhythm. For example, if the sinoatrial note (SAN) fails to undergo spontaneous depolarisation the atrioventricular node (AVN) may initiate electrical activity. Escape rhythms are typically slow (e.g. < 60 bpm).
When there is failure to transmit normal electrical activity this leads to a ‘block’ in the electrical pathway. This can occur within the SAN, AVN or bundle branches. Depending on the level and severity of the block, it may appear as a bradyarrhythmia.
These intrinsic abnormalities in conduction leading to bradycardia are commonly due to degenerative fibrosis, ischaemia, hypertensive heart disease or infiltration (e.g. amyloid).
Extrinsic
Most commonly, an increase in parasympathetic activity (i.e. vagal tone) may lead to a reduction in heart rate through its control on the SAN. This is usually seen in athletes who have a low resting heart rate.
Bradycardia may develop due to numerous external factors including hypothermia, increased intracerebral pressure, autonomic dysfunction, metabolic disturbances (e.g. hypocalcaemia, hyperkalaemia) or carotid sinus stimulation. Iatrogenic causes of bradycardia are also very common with the widespread use of rate-controlling medications (e.g. beta-blockers, calcium-channels blockers).
Escape rhythms
Each of the specialised structures involved in cardiac conduction has an intrinsic rate of autorhythmicity.
Autorhythmicity refers to the rate of spontaneous depolarisation, and therefore, the number of times the heart beats per minute. Each part of the conducting system has its own intrinsic rate.
- SAN: 60-100 bpm
- AVN: 40-60 bpm
- Ventricles: 20-40 bpm
The rate of autorhythmicity is highest in the SAN, which is why conduction is initiated here. If the SAN fails to undergo spontaneous depolarisation, electrical activity can be initiated lower down. This may occur in another part of the atrium, the AVN or the ventricles. When this happens, we can it an ‘escape’ rhythm.
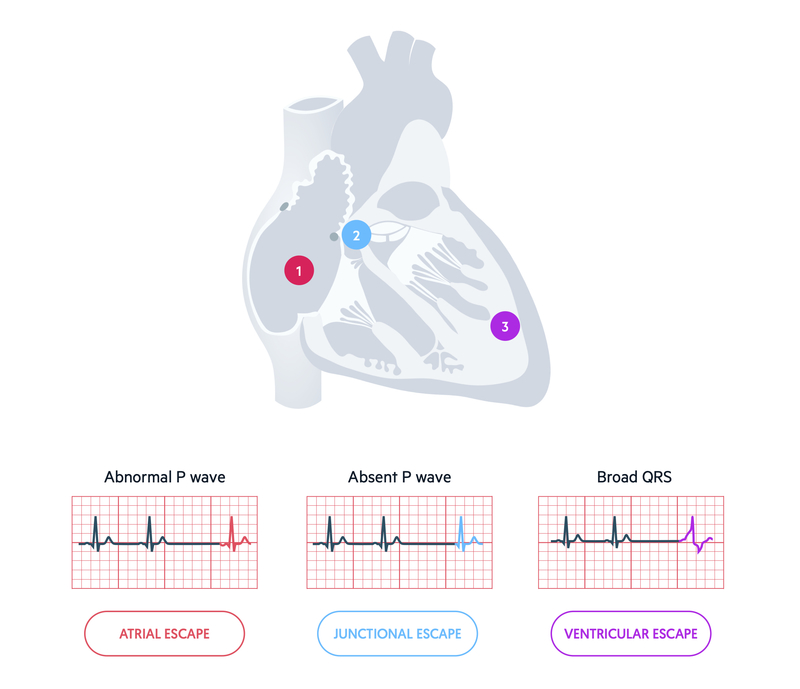
An escape rhythm may occur as a single beat or a sustained rhythm. A sustained escape rhythm is more likely to happen if there is complete failure of the conduction system above the level of the escape rhythm (e.g. AVN escape rhythm because SAN fails) or there is a disconnection between the atria and ventricles (e.g. complete heart block). A single beat may occur when part of the conduction system temporarily fails, then kicks back in (e.g. sinus pause).
Sinus bradycardia
Sinus bradycardia refers to sinus rhythm with a heart rate < 60 bpm.
Under normal circumstances at rest, our heart should be in sinus rhythm with an accompanying rate of 60-100 bpm. If the defining features of normal sinus rhythm are met but the heart rate is slow (< 60 bpm), we call it sinus bradycardia.
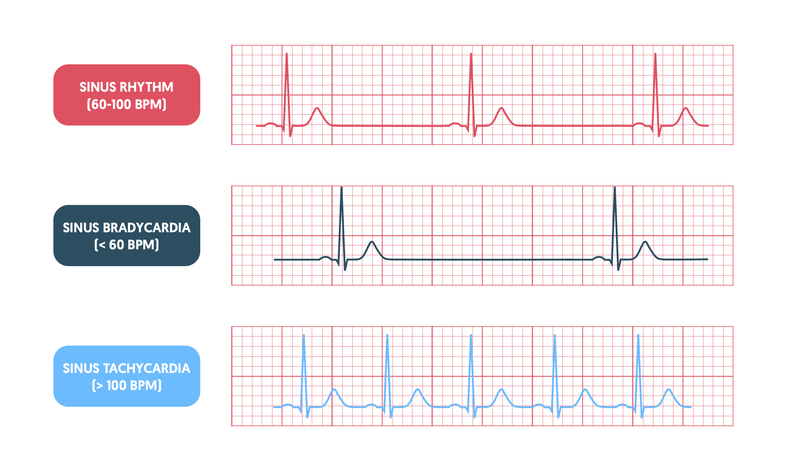
Sinus bradycardia may be normal in young, fit and healthy individuals. It would be unusual for an athlete to have a high resting heart rate. However, in older patients, or those with co-morbidities, sinus bradycardia may be suggestive of underlying SAN disease.
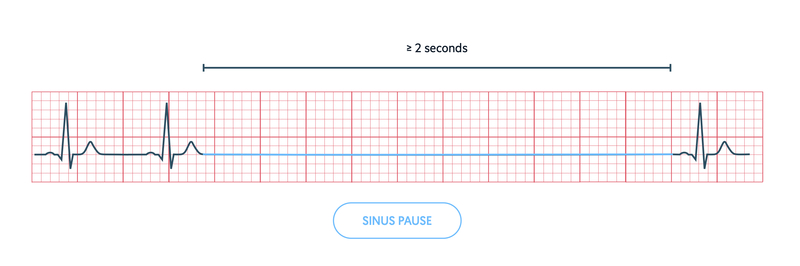
Sinus pause/arrest
Failure of the SAN to initiate electrical activity can be seen as an absent P wave on the ECG.
The SAN is the main pacemaker of the heart that initiates electrical activity. Dysfunction of the SAN may manifest as failed initiation of conduction (e.g. pauses/arrest) or failed transmission of electrical activity (e.g. sinoatrial exit block).
A sinus pause is defined as a transient absence of P waves that lasts from 2 seconds to several minutes. It is due to failure of the SAN to initiate electrical activity. It may be followed by resumption of normal electrical activity from the SAN or appearance of an escape rhythm (e.g. atrial or junctional escape).
Sinus node dysfunction
Sinus node dysfunction is a collective term that refers to conduction abnormalities affecting the SAN and surrounding tissue.
Sinus node dysfunction (SND), or ‘sick sinus syndrome’, comprises a variety of disturbances affecting both generation of electrical activity from the sinus node and transmission within the atria. It manifests clinically as a variety of ECG abnormalities including sinus bradycardia, sinus pause or arrest, sinoatrial exit block or chronotropic incompetence. Chronotropic incompetence refers to an inappropriate heart rate response to a physiological stimulus (e.g. exercise).
In addition to bradyarrhythmias, SND is associated with atrial tachyarrhythmias including atrial tachycardia, atrial fibrillation and atrial flutter. Often, patients may develop the well known ‘tachy-brady syndrome’, which presents with alternating bradyarrhythmias (e.g. sinus pause) and tachyarrhythmias (e.g. atrial fibrillation with fast ventricular response).

SND occurs due to depression of the normal autorhythmicity of the SAN and surrounding tissue. This may be due to intrinsic (e.g. fibrosis, ischaemia) or extrinsic factors (e.g. anti-arrhythmic agents).
Heart block
Interference of the normal transmission of conduction within the AVN can lead to varying degrees of ‘block’.
We commonly refer to abnormal conduction through the AVN as ‘heart block’. These may be differentiated into three types: first-degree, second-degree and third-degree.
- First-degree heart block: common. Delayed conduction. Prolongation of PR interval > 200ms
- Second-degree heart block: usually indicates underlying conduction disease. Intermittent failure in conduction. Dropped beats on ECG (i.e. no QRS to corresponding P wave). Differentiated into Mobitz type I (Wenckebach) and Mobitz type II.
- Third-degree heart block: always indicates conduction disease. Complete failure in conduction with AV dissociation. Complete dissociation between P waves and QRS complexes on ECG.
For more information on 'heart block' see our Conduction notes.
Clinical features
The clinical presentation of bradyarrhythmias may range from asymptomatic to shock.
Clinical features associated with bradyarrhythmias may be permanent, or occur intermittently due to the paroxysmal nature of the arrhythmia. They can present with a wide range of symptoms and signs.
- Fatigue, lethargy
- Dizziness, pre-syncope
- Syncope: transient loss of consciousness
- Dyspnoea: may suggest pulmonary oedema
- Chest pain: may suggest myocardial ischaemia
- Shock: low BP (< 90 mmHg), pallor, sweating, cold
- Impaired consciousness
The four cardinal features that suggest an unstable arrhythmia include: syncope, myocardial ischaemia (chest pain), heart failure (breathlessness) and shock (BP < 90 mmHg).
Management
The acute management of any bradyarrhythmia should follow an assessment using the principle ABCDE.
Assessment of an unwell patient should be completed using the structure airway (A), breathing (B), circulation (C), disability (D) and exposure (E). This remains true for any patient with a bradyarrhythmia. The resuscitation council guidelines provide a clear structure on the acute management of bradyarrhythmias.
Pharmacological therapy
Medications may be used in an attempt to increase the heart rate. Two common choices include atropine and isoprenaline.
- Atropine (antimuscarinic): reversible antagonist of muscarinic acetylcholine receptors. Blocks the action of the vagus nerve on the SAN and AVN. Leads to increased SAN electrical activity and increased conduction through the AVN. Given as IV bolus, which can be repeated.
- Isoprenaline (non-selective beta-adrenoreceptor agonist): positive inotropic and chronotropic effects on the heart via beta-receptors. Leads to an increase in heart rate and improved contractility. Given as IV infusion.
Medications usually act as a bridge to more definitive pacing or while the underlying cause of bradycardia is treated. If these medications fail, temporary or permanent pacing may be indicated.
Pacing
Pacing (temporary or permanent) delivers electrical stimuli to the heart via pacing leads.
Pacing may be required in an emergency setting (acute bradyarrhythmia), following myocardial infarction (ischaemia disrupts normal conduction) or as a long-term option in patients with bradyarrhythmias (i.e. completed semi-electively).
Temporary pacing
Methods of temporary pacing include non-invasive (transcutaneous) and invasive (epicardial or transvenous).
- Transcutaneous pacing: used in an emergency setting with severe bradycardia. Temporary measure before definitive pacing (i.e. transvenous, permanent). Completed using defibrillator and chest pads.
- Epicardial pacing: specialist device used within cardiothoracic surgery.
- Transvenous pacing: typically a single pacing wire is inserted into the right ventricle under fluoroscopic guidance (use of x-rays). Usually completed in a cardiac angiography suite.
Permanent pacing
A pacemaker is a permanent electronic device that is inserted under the skin, usually in the upper left chest wall.

Pacemaker scar at typical site of insertion.
The pacemaker box is attached to wires, which are inserted into the heart via the transvenous route. These can be seen on plain film radiograph.
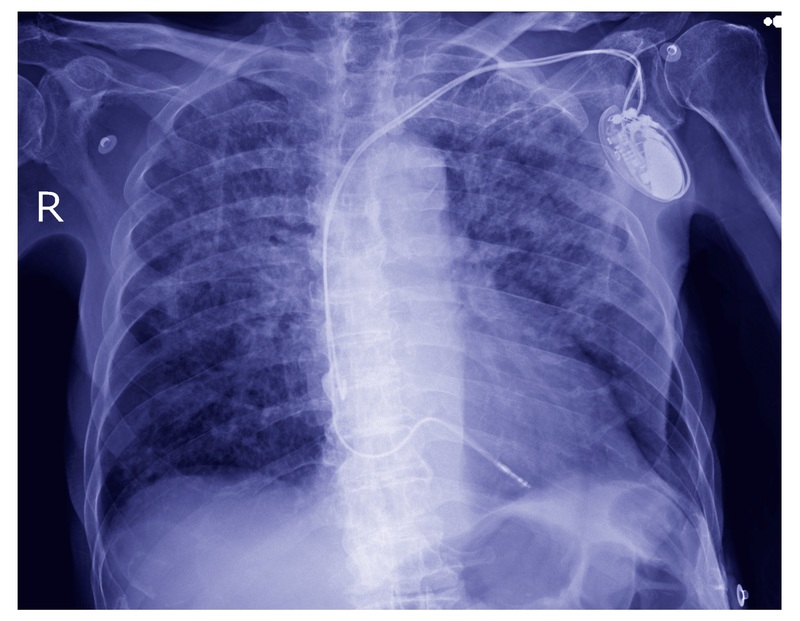
Dual chamber pacemaker seen on chest radiograph.
Permanent pacemaker indications
The European Society of Cardiology broadly divides indications for pacemaker insertion into three classes: I, II, III. This focuses on the risk/benefit of pacemaker insertion. A class I recommendation means the benefits outweigh the risk. A class I example is complete heart block.
There are three main types of pacemaker:
- Single chamber: single lead implanted into the right atrium or ventricle
- Dual chamber: two leads implanted, one in the right atrium and one in the right ventricle
- Biventricular (cardiac resynchronisation): left ventricular and right ventricular pacing. Used in heart failure.
Pacemaker codes
Pacemakers have a five letter code, which tells you how it is functioning. The first three letters refer to its anti-bradycardic function.
- First letter: refers to chamber being paced (A = atrium, V = ventricle, D = dual)
- Second letter: refers to chamber being sensed (A = atrium, V = ventricle, D = dual)
- Third letter: refers to response to sensing (T - triggered, I = inhibited, D = dual)
- Fourth letter: refers to rate modulation (i.e. rate changes in response to physiological demand)
- Fifth letter: refers to the anti-tachycardic function (P = pacing, S = shock, D = dual)
Last updated: October 2022
Have comments about these notes? Leave us feedback
