Acne vulgaris
Notes
Introduction
Acne vulgaris is a common chronic dermatological condition resulting from inflammation of the pilosebaceous unit.
Acne vulgaris is extremely common in adolescence affecting up to 95% of young people. Though in most cases it is relatively mild, up to 1/3 have moderate or severe disease. It results in comedones and inflammatory lesions that typically affect the face, chest and back.
Beyond (and secondary to) its dermatological manifestations it can have a profound impact on self-esteem and mental wellbeing.
Most cases respond to topical and/or oral therapies (e.g. antibiotics and retinoids). Specialist dermatological and mental health support can be required.
Epidemiology
20-35% of adolescents are affected by moderate or severe acne vulgaris in western countries.
It is predominantly a condition of adolescents and young adults affecting up to 95%. It is estimated that 85% of patients are aged 12-24, 8% 25-34 and 3% 35-44.
It affects males more than females in adolescence but becomes more common in females in adulthood.
Pathogenesis
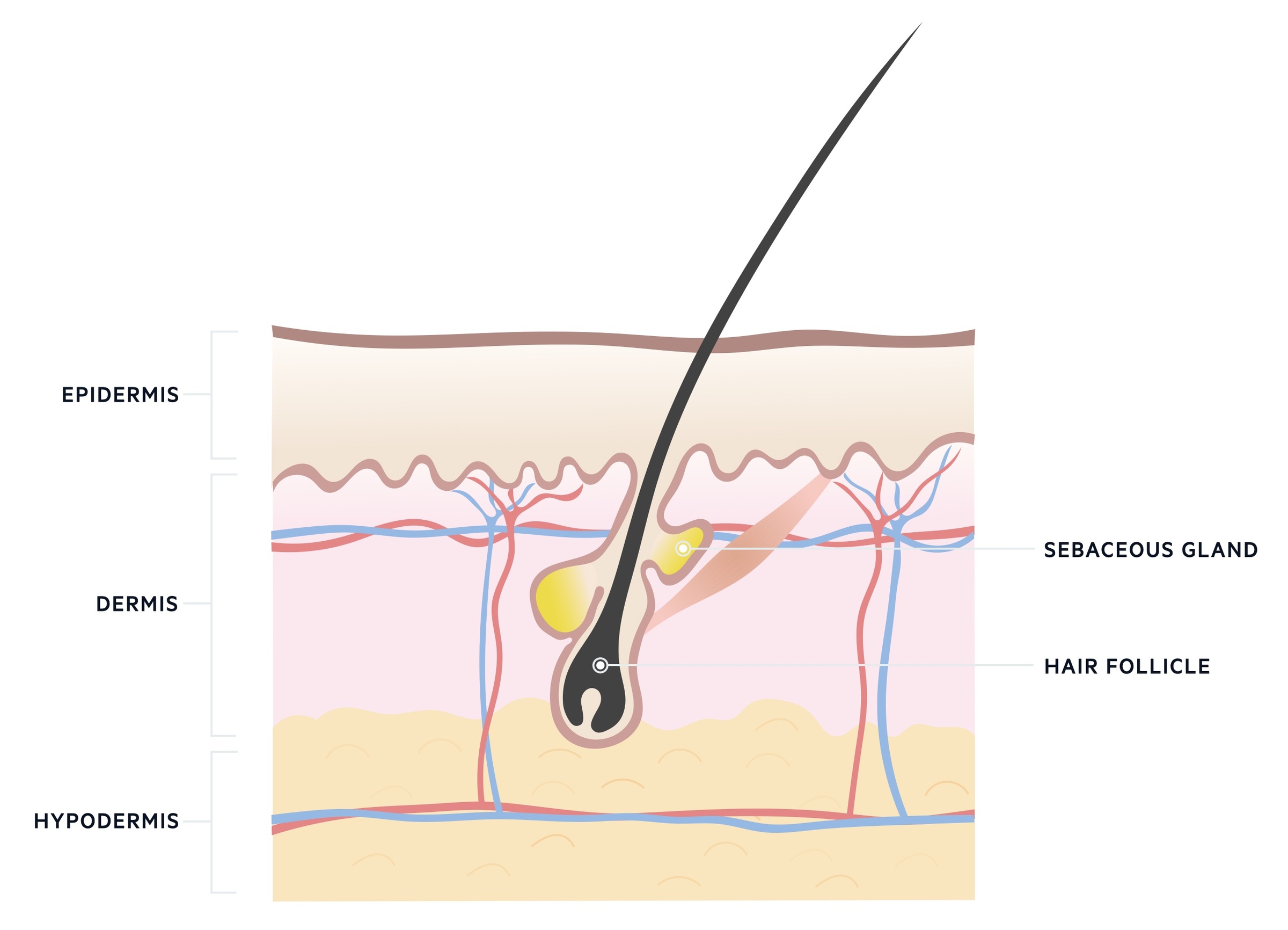
Acne vulgaris is an inflammatory disorder affecting the pilosebaceous unit.
The pilosebaceous unit refers to the hair follicle, hair shaft, arrector pili muscle and sebaceous gland. It is thought that blockage and inflammation of these units leads to acne vulgaris.
Acne vulgaris is thought to result from the complex interplay of numerous factors. The condition is characterised by:
- Non-inflammatory comedones
- Inflammatory papules, pustules and nodules
These lesions are thought to arise from precursor lesions termed microcomedo. Factors thought to lead to the development of acne vulgaris include:
- Altered keratinocyte proliferation
- Increased sebum production secondary to androgens
- Bacteria (cutibacterium acnes formerly propionibacterium acnes)
- Inflammation of the pilosebaceous unit
Insulin resistance, stress and skin trauma have all been identified as possible risk factors. There is a great deal of interest in the relationship between acne vulgaris and diet though research is ongoing.
Clinical features
Acne vulgaris is characterised by inflammatory and non-inflammatory lesions that typically affects the face, chest and back.
As described above, acne vulgaris is characterised by inflammatory and non-inflammatory lesions:
- Non-inflammatory comedones: closed comedones, often called whiteheads, are plugged follicles whilst open comedones, often called blackheads, are follicles with dilated openings (which allow oxidisation of follicle content resulting in a black colour).
- Inflammatory papules, pustules, nodules and cysts: papules and pustules are superficial, small raised lesions less than 5mm in size. Nodules and cysts are deeper, larger lesions (>5mm) that may be fluctuant.
These lesions tend to be located in areas with a lot of pilosebaceous glands - as such acne vulgaris typically affects the face, chest and back. In darker skin lesions can be less apparent as the erythema that surrounds lesions may be less obvious.
In chronic disease, skin may be affected by scarring due to the healing of lesions. Post-inflammatory depigmentation and hyperpigmentation of affected skin may occur.
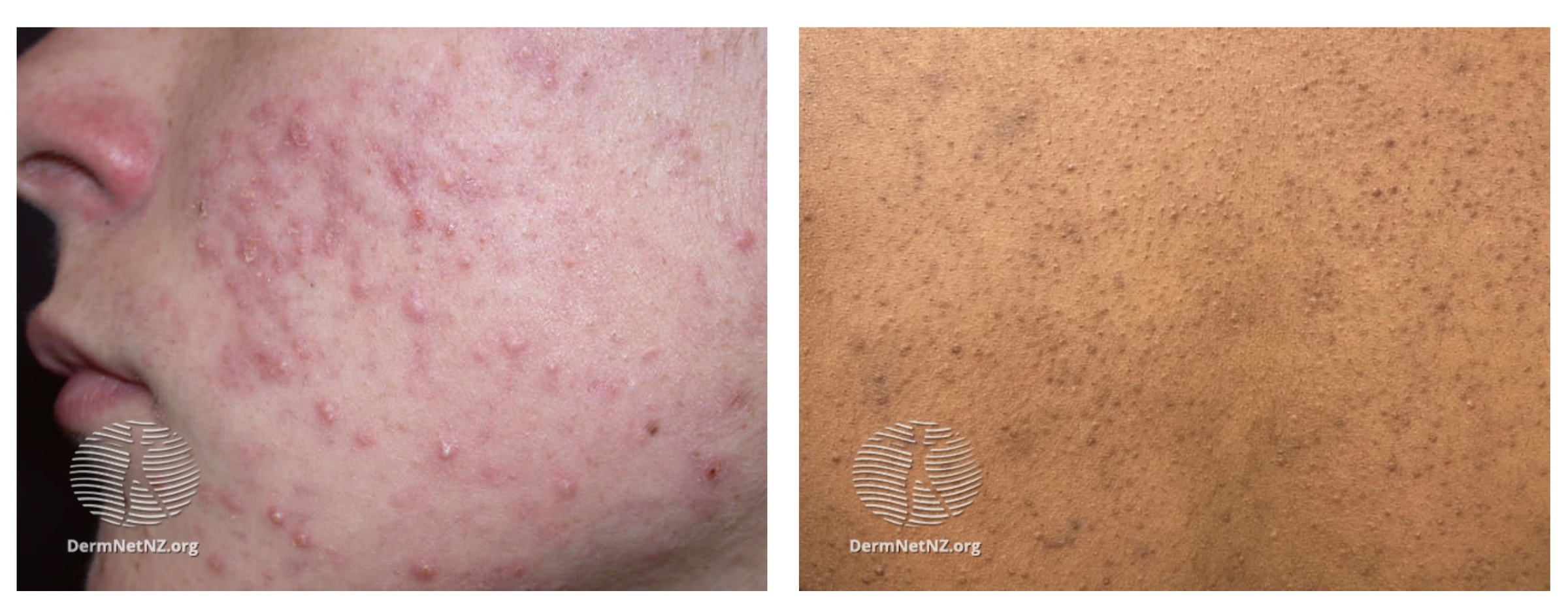
Acne vulgaris
Image courtesy of DermNet, Creative Commons licence
Acne conglobata
Acne conglobata is a rare and severe form of acne characterised by inflammatory nodulocystic disease with interconnecting sinuses and abscesses. It most commonly affects men between the ages of 18 and 30. Severe scarring may occur.
Its development is thought to be related to the bacteria cutibacterium acnes. It may also result from steroid use/abuse or androgen-producing tumours.
Acne fulminans
Acne fulminans is defined differently in various texts but NICE (NICE NG 198) describes it as a severe form of acne conglobata with systemic features such a fever, arthralgia and lymphadenopathy. It is rare and again typically affects young males.
Patients with this condition should be urgently referred to the local on-call dermatology team for same-day assessment.
Severity
Classifying the severity of acne vulgaris can be helpful in guiding its management.
There is no single universal classification for the severity of acne vulgaris. Severity can refer to the number and type of lesion present or the impact on a person's health and well-being.
NICE guideline 198 (June 2021) describes severity based on the lesions presents:
Mild to moderate acne includes people who have 1 or more of:
- any number of non-inflammatory lesions (comedones)
- up to 34 inflammatory lesions (with or without non-inflammatory lesions)
- up to 2 nodules
Moderate to severe acne includes people who have either or both of:
- 35 or more inflammatory lesions (with or without non-inflammatory lesions)
- 3 or more nodules
Management
The management of acne vulgaris involves skincare advice, topical and oral therapies and support for any associated mental health disorder.
Skincare advice
NICE guideline 198 (June 2021) offers the following skincare advice:
- Advise people with acne to use a non-alkaline (skin pH neutral or slightly acidic) synthetic detergent (syndet) cleansing product twice daily on acne-prone skin.
- Advise people with acne who use skincare products (for example, moisturisers) and sunscreens to avoid oil-based and comedogenic preparations.
- Advise people with acne who use make-up to avoid oil-based and comedogenic products, and to remove make-up at the end of the day.
- Advise people that persistent picking or scratching of acne lesions can increase the risk of scarring.
Medical therapy
There are a number of topical and oral treatments for acne vulgaris. The options depend on patient factors, preference and whether they are pregnant (or plan on getting pregnant) or breastfeeding. The side effect profile of each treatment should be considered and explained.
Patients should be advised that good adherence for several weeks (typically at least 6-8 weeks) is needed before beneficial effects are seen.
There are many options, here we give a brief outline of some of the most commonly used medications:
- Topical adapalene: a topical retinoid compound with anti-inflammatory effects. It is thought to reduce microcomedone formation.
- Topical benzoyl peroxide: is a keratolytic medication that also has antibacterial effects. It reduces the amount of the bacteria cutibacterium acnes.
- Topical tretinoin: has a combination of comedolytic and anti-inflammatory effects. It is also thought to reduce microcomedone formation.
- Topical clindamycin: is a bacteriostatic antibiotic that is active against cutibacterium acnes. It also has anti-inflammatory properties.
- Oral tetracyclines (doxycycline or lymecycline): are antibiotics that inhibit protein synthesis in bacteria.
For mild to moderate acne the following options should be considered:
- Topical adapalene with topical benzoyl peroxide: applied once daily in the evening. Cannot be used in pregnancy and caution is needed in breastfeeding. Side effects include skin irritation, burning sensation, bleaching (of hair and clothes) and photosensitivity.
- Topical tretinoin with topical clindamycin: applied once daily in the evening. Cannot be used in pregnancy or in those breastfeeding. Can cause skin irritation and photosensitivity.
- Topical benzoyl peroxide with topical clindamycin: applied once daily in the evening. Side effects include skin irritation, burning sensation, bleaching (of hair and clothes) and photosensitivity. It may be used with caution during pregnancy and breastfeeding.
For moderate to severe acne the following options should be considered:
- Topical adapalene with topical benzoyl peroxide: applied once daily in the evening. Cannot be used in pregnancy and caution is needed in breastfeeding. Side effects include skin irritation, burning sensation, bleaching (of hair and clothes) and photosensitivity.
- Topical tretinoin with topical clindamycin: applied once daily in the evening. Cannot be used in pregnancy or in those breastfeeding. Can cause skin irritation and photosensitivity.
- Topical adapalene with topical benzoyl peroxide plus either oral lymecycline or oral doxycycline: the topical medications are applied once daily in the evening with a once-daily oral antibiotic. Cannot be used in pregnancy or during breastfeeding. Tetracyclines are known to cause photosensitivity. Topical therapies may cause skin irritation, photosensitivity and bleaching. Cannot be used in under 12’s.
- Topical azelaic acid plus either oral lymecycline or oral doxycycline: the topical azelaic acid is applied twice daily whilst the antibiotic is taken once daily. Cannot be used in pregnancy or during breastfeeding. Tetracyclines are known to cause photosensitivity. Cannot be used in under 12’s.
The effect of treatment should be reviewed at 12 weeks. Generally, antibiotics should not be continued for longer than 6 months and should be stopped as early as possible.
If treatment has failed consider an alternative. In those with moderate to severe disease who have not had a regimen with an antibiotic, a regimen with an antibiotic should be considered. If they have already been on antibiotics, referral to dermatology should be made. In mild-moderate disease, referral should generally be considered after two treatment regimens have failed.
Oral isotretinoin
Isotretinoin is derived from vitamin A and is a powerful anti-inflammatory agent. It decreases sebum release and is thought to lead to a reduction in bacteria in the skin. It has a number of severe side effects and its use should be controlled by consultant dermatologists.
Oral isotretinoin is reserved for those with severe disease not responding to treatment and acne that is at risk of causing permanent scarring. It is only used in those over the age of 12 after appropriate counseling and consideration of the risks. Courses often last for 16-24 weeks.
NICE guideline 198 (June 2021) advises considering its use in those over the age of 12 who have failed treatment with topical therapies and systemic antibiotics. Examples include:
- Nodulocystic acne
- Acne conglobata
- Acne fulminans
- Acne at risk of permanent scarring
It may be given alongside a limited course of oral corticosteroids if the oral isotretinoin causes an acute flare. Oral corticosteroids can also be given at the onset of treatment in those with acne fulminans to prevent an acute flare.
Oral isotretinoin is teratogenic. Patients must understand this and follow the MHRA ‘Oral retinoid medicines: revised and simplified pregnancy prevention educational materials for healthcare professionals and women’.
It is also contraindicated in those with hypervitaminosis A, hyperlipidaemia, liver dysfunction or allergies to any of its constituents. It must be used with caution in those with renal impairment, diabetes and dry-eye syndrome.
It is important to assess the psychological well-being of patients both prior to and during therapy. There have been rare reports of sudden and severe worsening of depressive symptoms and suicide in those taking oral isotretinoin but a causal relationship is yet to be formally established.
For more information see this MHRA guidance.
Referral
Specialist review should be sought in patients acne conglobata or nodulocystic acne and where there is any diagnostic uncertainty.
Referral should also be considered in those not responding to treatment, with scarring or with persistent pigment changes.
In those suffering with significant or persistent psychological distress referral to both dermatology and mental health services should be considered.
Complications
Complications of acne vulgaris include permanent skin changes and effects on mental wellbeing.
Skin changes
Healing lesions can result in hypertrophic and/or atrophic scars. Hyper and/or hypopigmentation may also occur.
Psychological impact
The psychological impact varies between patients. It can have a significant effect on self-esteem often at a key time in a young person's development. There is an increased risk of anxiety, depression and suicide.
All patients should have their mental wellbeing checked, suicide risk assessed and offered a contact point if they should need it. This assessment should be repeated during their follow-up care.
Prognosis
Acne vulgaris tends to resolve at the end of growth.
Treatment regimens are effective in reducing or eliminating symptoms in many patients. The disease itself normally resolves as the individual reaches maturity and enters adulthood. Permanent scarring and/or pigment changes can occur.
A minority of patients are affected in adulthood, whilst others develop late-onset disease.
Last updated: August 2021
Have comments about these notes? Leave us feedback
