Gram-positive infections
Notes
Introduction
Bacteria are prokaryotic (single-celled) microorganisms that are found in both human health and disease.
Bacteria range in size from approximately 0.5-5.0 micrometers in length and different in morphology. Typical shapes of bacteria include spheres (i.e. cocci) and rods (i.e. bacilli) .
The human body is colonised with trillions of bacteria in normal health. This collective is known as the human microbiota and is important for normal functioning. Bacteria are also the cause of many clinically relevant infections in humans.
Cell wall structure
The general structure of a bacterium includes the cell wall, cell membrane, capsule, flagella, fimbriae, nuclear material, cytoplasm and other intracellular components.
The cell wall forms the outer aspect of bacteria, which protects it against host immune defences and external osmotic pressures. The cell wall differs depending on whether the organisms is gram-positive or gram-negative. These are the two major groups of bacteria.
- Gram-positive organisms: have a thick peptidoglycan layer composed of polysaccharides and charged amino acids interlaced with other major polymers like teichoic acid. Underneath the peptidoglycan layers is the cell membrane.
- Gram-negative organisms: have an outer cell membrane that contains lipopolysaccharides (LPS). Beneath the outer membrane is a smaller peptidoglycan layer compared to gram positive organisms and then the cell membrane. LPS is the key feature of gram negative organisms that contains lipid A. When broken down and released into the circulation, lipid A stimulates a profound inflammatory response that can lead to septic shock.
NOTE: Some bacteria do not have a cell wall (e.g. mycoplasma).
Gram stain
Gram staining is a technique used to identify microorganisms under a microscope.
Gram staining follows a number of steps:
- Application of primary stain: Crystal violet staining cells blue/purple
- Application of mordant: Gram's iodine solution is added, forms a complex with crystal violet
- Decolourisation: Agent such as acetone added, thinner peptidoglycan layer of gram-negative bacteria cannot retain the crystal violet-iodine complex
- Application of counterstain: Such as safranin, stains decolourised cells red.
In gram-positive bacteria, the thick peptidoglycan layer results in retention of the violet crystal. In gram-negative bacteria, the thin peptidoglycan layer results in loss of the crystal allowing its cell wall to be counterstained red.
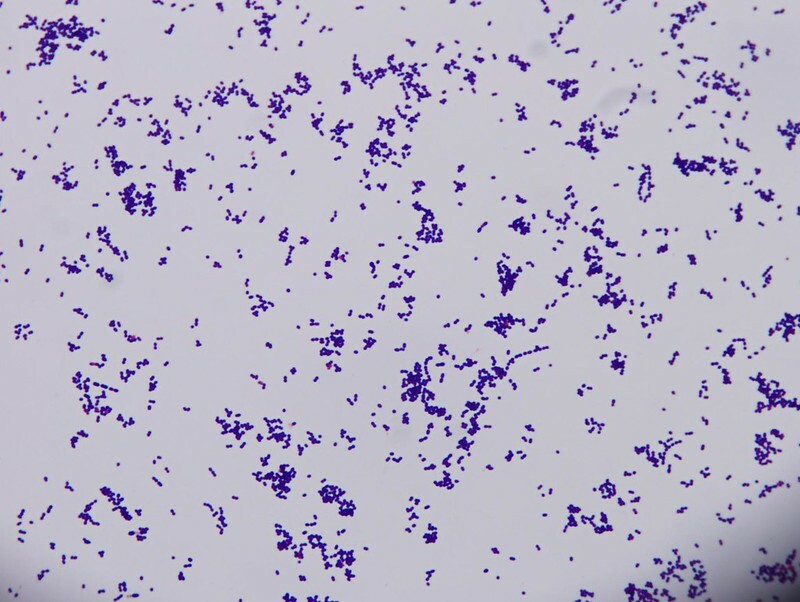
Gram-positive cocci, chains seen typical of a Strepococci
Image courtesy of Joe Rubin
Classification
Bacteria can be broadly divided into two main groups (gram-positive or gram-negative) based on gram staining of the bacterial cell well.
Gram-positive bacteria are further divided based on the morphology, which can be assessed under the microscope. The two major groups are cocci (spheres) and bacilli (rods).
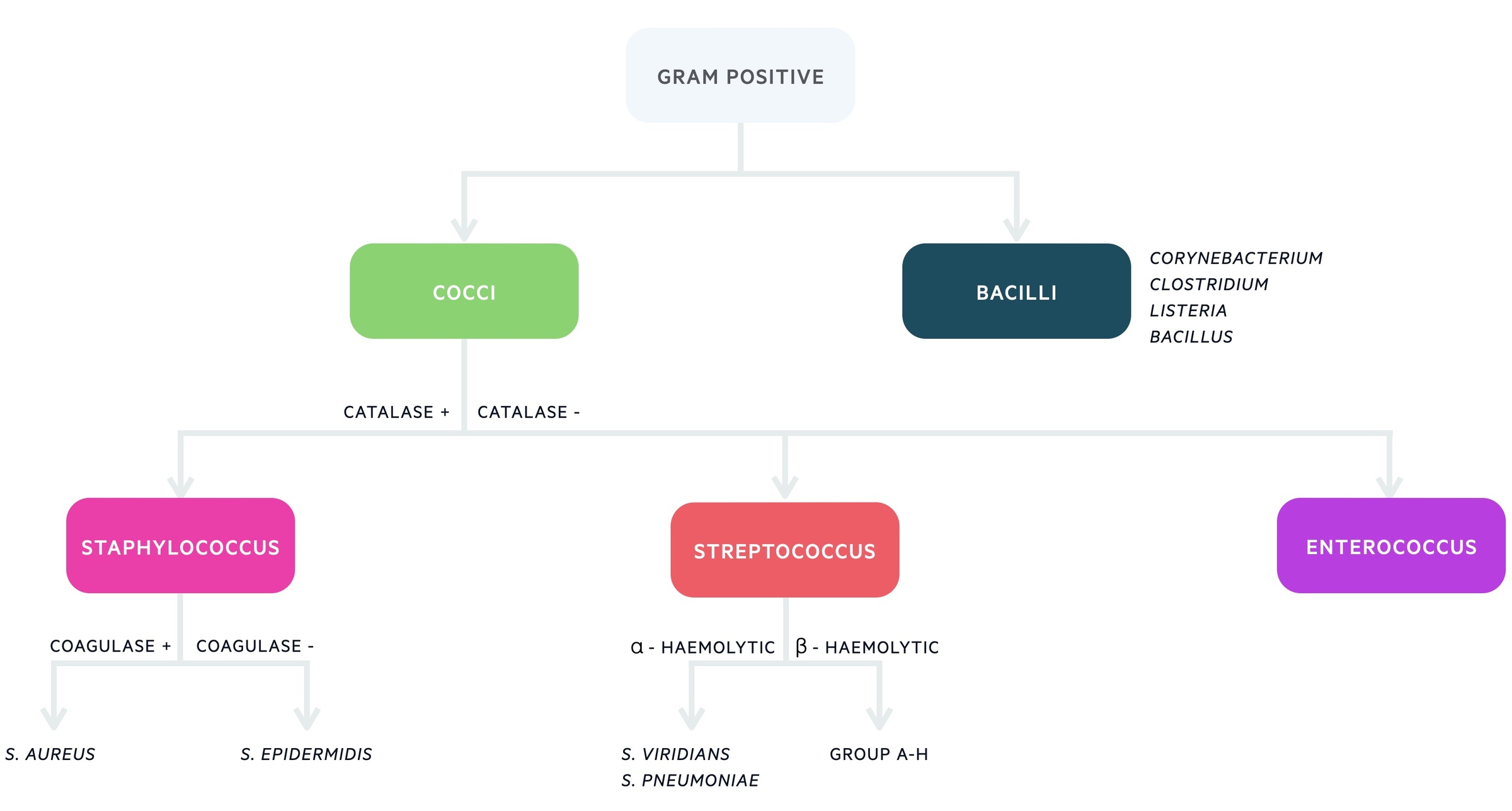
Further differentiation is then based on laboratory and molecular techniques that assess the different characteristics of gram positive bacteria.
Staphylococcus
Staphylococcal infections are common and are divided into coagulase-positive (e.g. S. Aureus) and coagulase-negative (e.g. S. saprophyticus)
Types
There are three main types of Staph to be aware of:
- Staphylococcus aureus (methicillin-sensitive: MSSA)
- Staphylococcus aureus (methicillin-resistant: MRSA)
- Coagulase negative Staphylococcus (CoNS)
CoNS consists of a group of > 40 microorganisms that are generally considered together in clinical practice. They are usually detected when there is contamination during blood sampling. This is because they are commonly found on the skin. However, they can cause significant infections in patients with indwelling foreign material (i.e. lines).
Shape
Staphylococcal microorganisms form cocci in clusters.
Locations
Common locations include skin, mouth, nose and throat. They live harmlessly on the skin of 1 in 3 people.
Infections
Typical infections associated with Staphylococcus include:
- Skin infections (i.e. cellulitis impetigo)
- Endocarditis (often in association with IVDU)
- Septic arthritis
- Osteomyelitis
Staphylococcus can release an exotoxin leading to specific infections including acute gastroenteritis, toxic shock syndrome and scalded skin syndrome.
- Toxic shock syndrome (TSS)
- TSS toxin-1
- Diffuse erythematous rash, diarrhoea, vomiting, fever, desquamation of palms and soles with septic shock
- Classically following infected ‘lost tampon’ used during menses
- However, 50% cases now unrelated to menses
- Scalded skin syndrome (SSS)
- Exfoliative toxin A & B
- Classically affects neonates
- Widespread blistering rash with exfoliation of skin
- Fluid loss and heat loss are most common problems
Treatment
Management depends on resistant patterns and allergy status, but options typically include flucloxacillin (MSSA) or vancomycin (CoNS, MRSA).
Streptococcus
Streptococcal microorganisms cause a wide range of clinically relevant infections.
Streptococcal classification is more complex and bacteria are broadly divided into three groups: alpha-, beta- and gamma-haemolytic.
Types
Streptococcal microorganisms are divided by their haemolytic properties. The two major groups are alpha- and beta-haemolytic. Beta-haemolytic bacteria are further divided based on Lancefield grouping.
- Alpha-haemolytic
- Streptococcus pneumonia
- Streptococcus viridans
- Beta-haemolytic
- Group A (S. pyogenes)
- Group B (S. agalactiae)
- Group C (S. dysgalactiae)
- Group D (S. Bovis)
- Others
Traditionally, enterococcal microorganisms were classified as beta-haemolytic group D streptococci. However, they have now been reclassified to an independent genus.
Shape
Streptococcal microorganisms typically form cocci in chains. Some Streptococci, like S. Pneumoniae, form diplococci (two bacteria together).
Locations
Streptococci are commonly found on the skin and in the throat.
Infections
Infections associated with streptococci depend on the type (i.e. alpha vs. beta-haemolytic) and include the following:
- Group A - beta-haemolytic
- Tonsillitis/pharyngitis
- Cellulitis +/- Necrotising fasciitis
- Scarlet fever
- Rheumatic fever
- Group B - beta-haemolytic
- Neonatal infections (meningitis, pneumonia, sepsis)
- Found in vaginal flora in high percentage of pregnancies
- Alpha-haemolytic
- Pneumonia
- Meningitis
- Endocarditis (usually left-sided from alpha-haemolytic microorganisms)
- Dental infections
Enterococci (re-classified from streptococci) can form part of the normal bowel flora. They are commonly associated with UTIs, biliary infections, intra-abdominal infections and endocarditis.
Treatment
Antibiotics used to treat streptococcal infections include beta-lactams (i.e. penicillin, ceflasporins). In severe cases, or those with high resistance, glycopeptides (i.e. vancomycin) or carbapenems (i.e meropenem) are used.
Gram-positive bacilli
There are four major gram-positive bacilli that cause clinically significant infections in humans.
They can be divided into spore-forming (Bacillus, Clostridium) and non-sporing (Listeria, Corynebacterium). They are briefly discussed below.
Clostridium
Clostridium is an anaerobic gram-positive rod that causes a range of clinically important infections related to toxin release.
- Clostridium difficile (i.e. 'C. Diff')
- Profuse, watery diarrhoea due to secretions of two toxins (A & B)
- Commonly associated with antibiotic use and overgrowth of 'C. diff' in the bowel
- In severe cases causes pseudomembranous colitis and toxic mega colon
- Clostridium botulinum
- Causes flaccid paralysis due to secretion of neurotoxin.
- Toxin now commercially available as Botox
- Clostridium Tetani
- Causes tetanus from release of tetanus toxin, vaccinations available
- Clostridium perfringens
- Cause of gas gangrene via alpha toxin leading to myonecrosis
Listeria
Listeria monocytogenes can cause meningitis, often in neonates, or patients who have consumed unpasteurised milk.
Bacillus
Bacillus cereus is a common cause of food poisoning (i.e. gastroenteritis). It classically occurs following consumption of re-heated rice.
Corynebacterium
Corynebacterium diphtheria releases an exotoxin that causes the potentially fatal condition diphtheria. Widespread vaccination programme now in place.
Last updated: March 2022
Have comments about these notes? Leave us feedback
