Peripheral neuropathy
Notes
Overview
Peripheral neuropathy is a broad term that refers to any disorder of the peripheral nervous system.
Peripheral neuropathy is a broad term that refers to damage to any of the peripheral nerves that make up the peripheral nervous system. The human nervous system is broadly divided into central and peripheral.
- Central nervous system: this encompasses the brain and spinal cord
- Peripheral nervous system: this encompasses the cranial nerves, spinal nerves, spinal roots, plexuses, peripheral nerves, and the neuromuscular junctions
The peripheral nervous system is important for passing information to and from the central nervous system. Nerves within the peripheral nervous system can be divided based on their gross function (e.g. motor, sensory, autonomic).
Each peripheral nerve is composed of a cell body, dendrites, and an axon that is insulated by a myelin sheath helping improve the speed of conduction. This is important because damage to peripheral nerves can affect the myelin sheath or the nerve axons.
Here, we give a concise overview of the different types of peripheral neuropathy. For more in-depth information, check out the following notes:
Terminology
Peripheral neuropathy is a very general term that refers to damage to the nerves of the peripheral nervous system.
Peripheral neuropathies can be further divided into different forms depending on the type and pattern of nerve involvement. These include:
- Polyneuropathy: refers to generalised involvement of multiple peripheral nerves
- Radiculopathy: refers to involvement of a spinal nerve root
- Plexopathy: refers to involvement of a network of nerves known as a plexus (e.g. brachial plexus)
- Mononeuropathy: refers to involvement of a single nerve
- Mononeuritis multiplex: refers to simultaneous or sequential involvement of ≥ 2 separate nerves
The terms polyneuropathy and peripheral neuropathy are often used synonymously, which can be confusing. Remember, polyneuropathy refers to a specific subset of peripheral neuropathies and ideally the terms should not be used interchangeably.
The term 'palsy' is also used commonly in clinical practice. Palsy generally references the motor component of a neuropathy (i.e. the weakness).
Aetiology & pathophysiology
There are many different causes of peripheral neuropathy.
Our peripheral nerves are susceptible to damage by many different insults. The pattern of involvement (e.g. polyneuropathy versus mononeuropathy), the speed on onset (e.g. acute or chronic) and the type of nerves involved (e.g. motor and/or sensory) are often dependent on the underlying aetiology.
As there are so many possible causes, it is often easier to consider them as part of a surgical sieve, which is a way of structuring the differential diagnosis into broad categories. There are many useful mnemonics for a surgical sieve (e.g. VITAMIN DC) that can be used to help remember the categories.
We have grouped the major causes of peripheral neuropathy into the categories below (not an exhaustive list):
- Idiopathic
- Vascular: vasculitis
- Metabolic: diabetes mellitus, hypothyroidism
- Infective: HIV, Lyme disease, hepatitis C
- Inflammatory: chronic inflammatory demyelinating polyneuropathy
- Autoimmune: Guillain-Barré syndrome, connective tissue diseases
- Neoplastic: paraneoplastic syndromes, multiple myeloma, tumours (causing compression)
- Nutritional: Vitamin B12 or folate deficiency
- Drugs: chemotherapy, Isoniazid, Metronidazole
- Systemic illness: critical illness, chronic kidney disease, chronic liver disease, amyloidosis
- Toxic: heavy metals, alcohol
- Trauma: usually due to compression
- Hereditary: Charcot-Marie tooth, familial amyloidosis
Regardless of the underlying aetiology, damage to peripheral nerves is caused by three major mechanisms:
- Axonal degeneration: damage to nerve axons. Typically causes a ‘dying-back phenomenon’ that starts distal and progresses proximally. Usually causes symmetrical polyneuropathy with weakness
- Wallerian degeneration: damage to the nerve axon due to a lesion or physical compression (e.g. carpal tunnel syndrome). Commonly seen in mononeuropathies with the portion of the nerve distal to the compression affected
- Demyelination: degeneration of the myelin sheath is seen. In pure demyelination, there is sparing of the axon. The clinical presentation is more variable
Polyneuropathies
Polyneuropathies often are often ‘length-dependent’ meaning more distal nerves are affected first.
Polyneuropathy is a broad term that refers to damage to multiple peripheral nerves. It is classically distally located with a ‘glove and stocking’ distribution (e.g. hands and feet), usually symmetrical, and may be sensory, motor, or mixed. Polyneuropathies are often ‘length-dependent’ meaning the more distal nerves are affected first and then progress proximally.
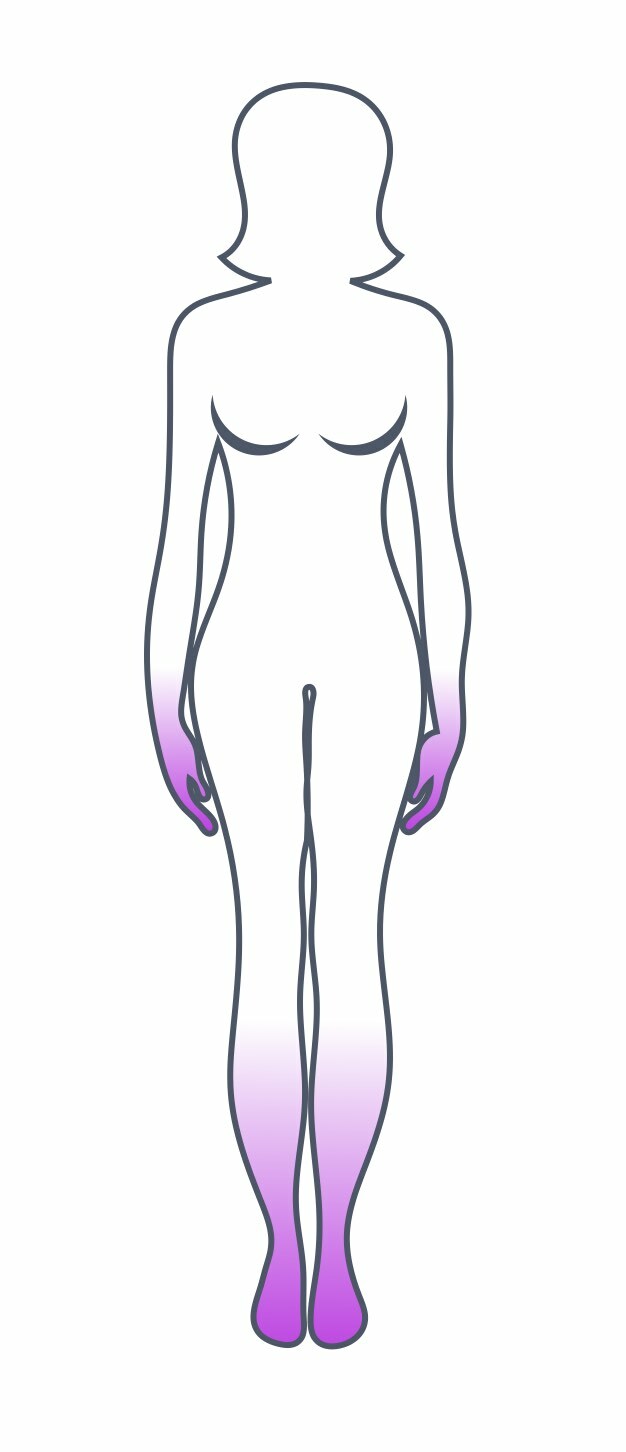
Polyneuropathy with 'glove and stocking' distribution
There are many different causes of polyneuropathy and the onset and disease course largely depends on the aetiology. For example, diabetic polyneuropathy often starts as a slowly progressive sensory/painful polyneuropathy. On the other hand, Guillain-Barré syndrome can cause an acute, rapidly progressive polyneuropathy with predominant weakness.
For more information see our Polyneuropathies note.
Radiculopathies
Radiculopathy refers to symptoms or impairments related to the involvement of a spinal nerve root.
The spinal nerve roots serve as the main communication between the central nervous system (i.e. the spinal cord) and the peripheral nerves. The spinal cord is divided into four main regions termed cervical, thoracic, lumbar, and sacral. This is further divided into 31 spinal cord segments. Arising from the 31 spinal cord segments are the paired ventral and dorsal spinal nerve roots, which join to form the 31 paired spinal nerves (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal).
Damage or impingement of a spinal nerve root is known as radiculopathy. Each spinal nerve root carries important sensory/motor functions along a specific distribution. These are known as myotomes and dermatomes:
- Myotome: a collection of muscles innervated by a single spinal nerve root
- Dermatome: an area of skin supplied by a single spinal nerve root
Therefore, radiculopathy leads to symptoms and/or impairment in the distribution of the nerve roots myotome and/or dermatome. This can lead to weakness in some or all of the muscles innervated by that nerve root and sensory changes (e.g. paraesthesia, pain, sensory loss) in the skin corresponding to that nerve root.
Any nerve root can be affected although by far the most common are the lumbosacral nerve roots (e.g. L5 and S1). When multiple nerve roots are affected together, it is known as polyradiculopathy.
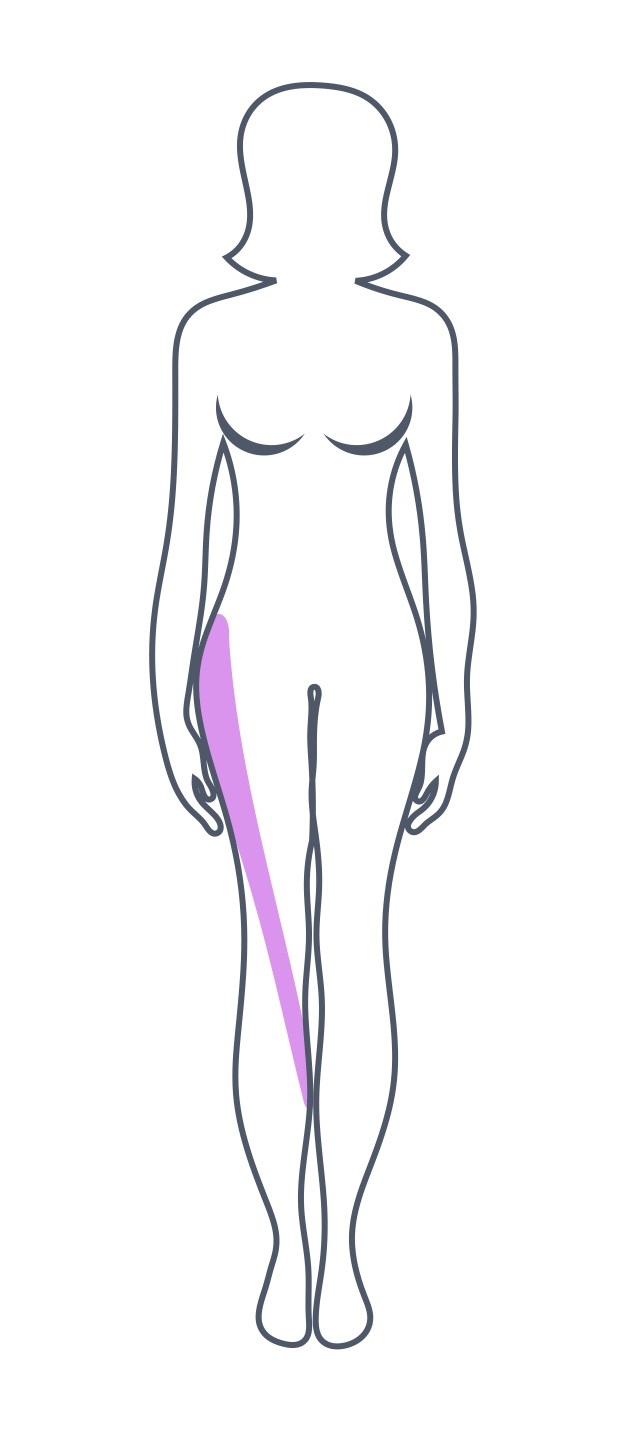
Dermatomal distribution of the L3 nerve root
Sciatica
One important point is the term sciatica. Sciatica is a non-specific clinical description of pain affecting the back and/or leg.
It is typically used to describe a sharp or burning pain that radiates from the buttock along the course of the sciatic nerve down the posterior/lateral leg and usually to the foot or ankle. The sciatic nerve is formed by a combination of nerve roots L4, L5, S1, S2, and S3. Therefore, the involvement of any of these nerve roots alone or in combination can cause a variety of sciatic-like symptoms.
Sciatica is therefore the clinical manifestation of lumbosacral radiculopathies. However, the difficulty arises in the fact that the term is used more generally as a reference to lower back pain that may be non-radicular in origin (i.e. not caused by radiculopathy). Therefore, when a patient has ‘sciatica’ it is important to determine exactly what is meant by the term and whether there is ‘radicular’ quality to the pain.
For more information see our Radiculopathies note.
Mononeuropathies
A mononeuropathy refers to damage or dysfunction of a single peripheral nerve.
Mononeuropathy is a broad term that refers to damage or dysfunction of a single peripheral nerve. This typically leads to a characteristic set of clinical features with motor and/or sensory dysfunction relating to the usual function of the nerve involved.
Mononeuropathies are commonly due to entrapment or compression as peripheral nerves have to travel through small openings and between other major structures. Compression of the nerve may be internal (e.g. nerve tumour), or external (e.g. fracture, compressive clothing, unusual posture).
There are many peripheral nerves in the body and each may be affected in different ways as the course of each nerve is different. We can broadly think of mononeuropathies in three groups:
- Cranial mononeuropathies: relates to the 12 paired nerves arising from the brain and brainstem
- Upper limb mononeuropathies: relates to the peripheral nerves involved in upper limb function
- Lower limb mononeuropathies: relates to the peripheral nerves involved in lower limb function
Common nerves in the upper limb that can present as a mononeuropathy include the median, ulnar and radial nerves. Common nerves in the lower limb that can present as a mononeuropathy include the common peroneal and tibial nerves.
For more information see our Mononeuropathies note.
Plexopathy
A plexus refers to a collection of proximal segments of peripheral nerves.
When spinal nerve roots exit the spinal cord they may enter a plexus. A plexus simply refers to a branching network of nerves (or vessels). They may arise from the merging of spinal nerves (e.g. cervical plexus, lumbosacral plexus) or the merging of autonomic nerves around major organs (e.g. cardiac plexus, coeliac plexus).
With spinal nerve plexuses, they are formed by a merging and intertwining of proximal segments of peripheral nerves before they form individual nerves more distally. This means that information from multiple spinal nerve roots may be conveyed along a single peripheral nerve.
The two major plexuses are the brachial and lumbosacral. When there is damage or dysfunction of a plexus it is known as a plexopathy.
Brachial plexus
This is formed by the nerve roots C5-T1. It is divided into different regions known as trunks, divisions, cords, and terminal branches. There are different causes of brachial plexopathy that may be broadly divided into traumatic and non-traumatic. The clinical presentation depends on the pattern of involvement of the brachial plexus:
- Traumatic: contact sport, difficult birth (e.g. Erbs’ palsy with the arm held in Waiter’s tip position), road traffic accident
- Non-traumatic: neuralgic amyotrophy (an inflammatory disorder of brachial plexus), other rare causes (e.g. thoracic outlet syndrome)
Lumbosacral plexus
The lumbosacral plexus is formed by the nerve roots L1-S4. Each root divides into anterior and posterior branches that subsequently merge and intertwine to form individual nerves. Damage to the lumbosacral plexus is commonly due to trauma and leads to a constellation of symptoms including asymmetrical weakness, numbness, and paraesthesia in the distribution of multiple lumbosacral nerve roots.
Mononeuritis multiplex
Mononeuritis multiplex refers to simultaneous or sequential involvement of ≥2 separate nerves.
Mononeuritis multiplex is a type of peripheral neuropathy that results in isolated damage or dysfunction to at least two separate nerves that may occur simultaneously or sequentially. Importantly, the nerves are noncontiguous (i.e not adjacent to one another).
Mononeuritis multiplex is also known as multiple mononeuropathy. It is one of the classic presentations of vasculitis affecting the peripheral nerves. Vasculitis leads to inflammation of the small vessels that provide the blood supply to nerves (known as the vasa nervorum). This inflammation leads to obstruction and eventually infarction of peripheral nerves. Other mechanisms that can result in mononeuritis multiplex include ischaemia (e.g. diabetes mellitus), inflammatory/immune-mediated (e.g. sarcoidosis, multifocal motor neuropathy), infections (e.g. Lyme, Leprosy), mechanical (e.g. multiple entrapments), or even drug-induced (e.g. Sulfonamides).
In mononeuritis multiplex patients may present with a single mononeuropathy (e.g. common peroneal neuropathy), which is followed by a second mononeuropathy (e.g. ulnar neuropathy). The clinical features relate to the affected nerve (e.g. foot drop in a common peroneal neuropathy). Consequently, mononeuritis multiplex is often an asymmetrical, painful, peripheral neuropathy. As the disease progresses, it may mimic a more generalised polyneuropathy as contiguous (i.e. adjacent) nerves become affected.
Diagnosis & investigations
Electromyography and nerve conduction studies are key investigations to confirm peripheral neuropathy.
A variety of investigations can be requested depending on the type of peripheral neuropathy, the pattern of involvement and suspected underlying aetiology.
The need for extensive investigations depends on the suspected cause and the severity. For example, in patients with mild polyneuropathy secondary to known diabetes mellitus, extensive testing is probably not necessary. However, in a patient with new mononeuritis multiplex, extensive investigation to exclude a serious underlying cause such as vasculitis would be warranted.
Often, in cases of polyneuropathy, the cause may not be immediately apparent so numerous investigations need to be requested to determine the underlying cause.
Electrodiagnostic tests
Electrodiagnostic tests can be used to confirm peripheral neuropathy and these should be requested and interpreted in line with the clinical presentation. The two main tests include electromyography (EMG) and nerve conduction studies (NCS):
- Electromyography (evaluates muscle units): this refers to an assessment of the electrical activity of muscles. It can assess activity during rest and voluntary contraction. It is important in the assessment and diagnosis of neuromuscular disease. It helps to differentiate between the different types of peripheral neuropathy (e.g. motor mononeuropathies, plexopathy) as well as muscle abnormalities (e.g. neuromuscular junction, myopathy). EMG records the electrical potentials generated in a muscle belly through the insertion of a needle
- Nerve conduction studies (evaluates peripheral nerves): this refers to an assessment of individual peripheral nerve function. It essentially involves activating nerves electrically over several points on the skin of the upper/lower limbs and measuring the response. The test involves assessing both the size (i.e. amplitude) and speed (i.e. velocity) of signals through the motor and sensory fibres. These studies can determine the type of injury (e.g. demyelinating, axonal degeneration or conduction block from compression).
Each test has its own strength and limitations. The combination of both helps to better localise the pathology and narrow down the possible underlying aetiology.
Other investigations
A wide number of investigations can be requested to determine the cause of peripheral neuropathy. The choice of test largely depends on the type of peripheral neuropathy, clinical presentation and pattern of involvement.
Some example investigations are discussed below, but this is not an exhaustive list:
- Full blood count: may show macrocytic anaemia suggestive of vitamin B12 or folate deficiency. Macrocytosis may also be a feature of some haematological malignancies and alcohol excess
- Renal function: assess for chronic kidney disease
- HbA1c: assess for diabetes mellitus
- Thyroid function tests: assess for hypothyroidism
- Immunological: immunoglobulins and protein electrophoresis for plasma cell disorders (e.g. myeloma)
- Autoimmune tests: ANA, ENA, Anti-CCP, complement for connective tissue diseases
- Virology/Infection: serology for hepatitis C, syphilis, or Lyme disease
- Heavy metals: copper, lead
- Vitamins: B12, folate, pyridoxine
- Imaging: MRI, CT or US may be needed if there is concern about compression or structural lesions
- Biopsy: a nerve biopsy may be rarely performed
- Genetic testing: specialist test that may be considered for hereditary causes
Management
Management of peripheral neuropathy depends on the underlying cause.
The management of peripheral neuropathy is highly variable and depends on the underlying aetiology. In many cases, there is no specific treatment for peripheral neuropathy, and management aims to treat or address the underlying cause.
Patients with mononeuropathies are more likely to have a specific problem (e.g. carpal tunnel syndrome causing median nerve mononeuropathy) that may be addressed with specific treatment (e.g. carpal tunnel release). Chronic polyneuropathies are often only mildly disabling and slowly progressive so can just be monitored over time. Addressing underlying factors such as good diabetic control or administration of vitamin B12 is essential. Acute polyneuropathies such as Guillain-Barré syndrome can be life-threatening and require urgent treatment such as intravenous immunoglobulin.
It is important to also consider the symptoms of the patient who may be experiencing painful paraesthesia and/or motor weakness. These patients may require neuropathic pain medications to reduce the severity of the symptoms (e.g. Gabapentin, duloxetine) and may require additional help from allied health professionals (e.g. physiotherapy and occupational therapy if disabling foot drop).
We cannot give in-depth treatment for all possible aetiologies but hopefully, this gives an insight into how to approach the management of a patient with peripheral neuropathy.
Last updated: July 2022
Have comments about these notes? Leave us feedback
