Gout
Notes
Overview
Gout is a crystal arthropathy resulting from excess levels of uric acid leading to precipitation in joints and other tissue.
Gout is the most common inflammatory arthritis across the world. The overall prevalence of gout is increasing, estimated at 2.49% in the UK.
It is more common in the elderly and has a male predominance with a male to female ration of 4.3:1.
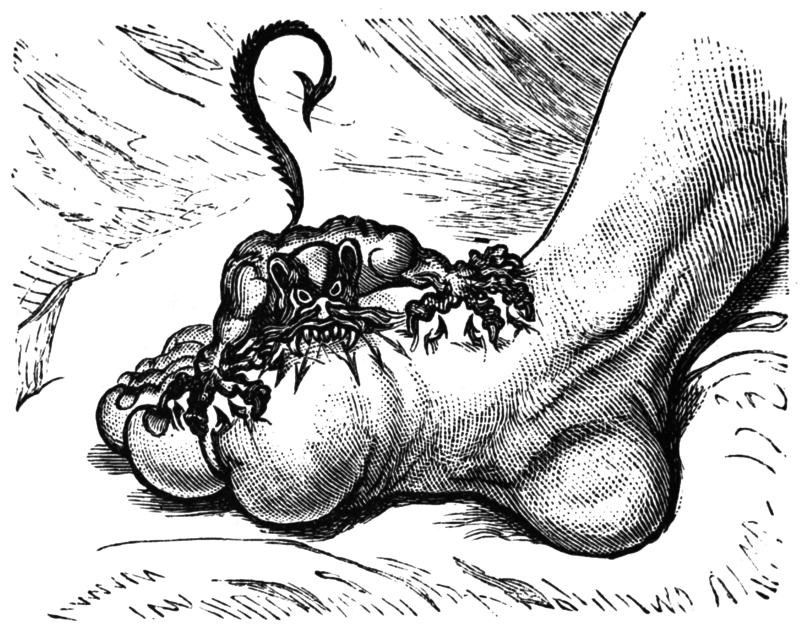
A caricature by James Gillray, an 18th century artist
Risk factors
High uric acid levels, or hyperuricaemia, is the single most important risk factor for the development of gout.
- Hyperuricaemia
- Alcohol
- Obesity
- Male gender
- Age
- Renal disease
- Dyslipidaemia
- Chemotherapy
- Diabetes mellitus
People with normal uric levels can still develop gout, and conversely, people with high uric acid levels may never develop gout. However, risk of gout increases significantly with increasing levels or uric acid.
The 5-year cumulative incidence of gout per 1000 people is 5 for uric acid levels < 420 micromol/L but 305 for uric acid level > 599 micromol/L.
Hyperuricaemia
Gout is a disorder of purine metabolism that results in increased levels of uric acid within the body.
Uric acid is a breakdown product of purines and it may precipitant in joints, soft tissue or urinary system leading to the clinical manifestations..
Uric acid is predominantly renal excreted (70%) with the remaining excreted via the gastrointestinal tract. When there is an imbalance between production and excretion of uric acid it may crystallise and deposit in soft tissue and joints.
There are three main mechanisms leading to the development of gout:
- Purine overproduction: This occurs when there is increased cell turnover or lysis of cells leading to release of purines and breakdown to uric acid. Causes include myelo- or lymphoproliferative disorders, psoriasis and use of chemotherapy agents.
- Increase purine intake: There are several foods and beverages that are rich in purines and increase the risk of developing gout. These include seafood (i.e. anchovies, sardines), red meat, alcohol and fructose-rich beverages.
- Decreased uric acid secretion: Uric acid is predominantly renal excreted so anything that affects the kidneys can increase the risk of developing gout. Causes include diuretics (i.e. furosemide), acute kidney injury, chronic kidney disease, ACE inhibitors and diabetes mellitus.
Crystal formation
Gout is the result of high uric acid levels leading to supersaturation and precipitation of monosodium urate crystals in soft tissue, joints and kidneys.
Monosodium urate crystals precipitate in peripheral joints (i.e. metatarsophalangeal joints) because they are less soluble at low temperatures. Urate forms needle-like crystals that can be detected on plane-polarised light. Characteristically, monosodium urate crystals are negatively birefringent.
The deposition of crystals within joints and soft-tissue may occur asymptomatically such as in chronic gout with the formation of small gouty tophi on the skin. However, during acute attacks, crystals trigger an acute inflammatory reaction leading to acutely painful swollen joints.
Clinical features
The classical presentation of gout is an acutely painful and swollen joint that begins abruptly, reaches intensity within 12 hours and lasts less than 2 weeks if left untreated.
Gout typically affects the first metatarsalphalangeal joint (approximately 70% of first attacks). Other common joints include the knees ankles, wrists, finger joints. In addition, gout may affect more than one joint at a time known as polyarticular gout. However, polyarticular gout usually only presents in 10% of cases.
If hyperuricaemia is left untreated it can lead to chronic tophaceous gout, which is characterised by the development of multiple tophi (collections of urate crystals in soft tissue). These are classically located on the helix of the ear, fingers, toes, prepatellar bursa and by the olecarnon. Overtime, recurrent flares of acute gout can lead to chronic polyarticular arthritis.
Classical presentations
- Acute monoarticular gout
- Joint pain, swelling, erythema
- Most commonly 1st MTP
- Acute polyarticular gout
- Join pain, swelling, erythema
- Typically fingers, toes, wrists, ankles and knees
- Chronic tophaeous gout
- Tophi
- Degenerative arthropathy
Investigations
Gout is usually a clinical diagnosis though joint aspiration can be used to confirm.
Serum uric acid
Levels should be taken 4-6 weeks following an acute attack. Though suggestive, elevated levels are not themselves diagnostic of gout. Normal serum uric acid does not exclude gout.
NOTE: During an acute attack, plasma urate levels often fall.
Joint aspiration
This is the gold standard investigation for the diagnosis of gout but is often not required. A joint aspiration should always be completed if there is concern about septic arthritis or where the diagnosis is in doubt.
In addition to crystal microscopy joint fluid should be sent for microscopy, culture and sensitivities. Gout is diagnosed by the presence of needle-shaped monosodium urate crystals that are negatively birefringent under plane-polarised light.
Plain radiographs
Plain radiographs are typically normal in acute episodes of gout. It helps to exclude a number of differentials and may show subcorticol cysts or bone erosion.
Further investigations
Gout may result from and indicates increased risk of other systemtic conditions. Patients should be screened for cardiovascular and renal disease.
Acute management
The management of gout can be divided into the acute management and long-term prevention.
- General advice: Advise rest, ice and elevation. Lifestyle measures such as weight loss, diet and alcohol consumption should be discussed.
- First-line therapy: Offer NSAIDs (e.g. naproxen) or oral colchicine. Co-prescribe a PPI for gastric protection if giving an NSAID. Aspirin is not indicated.
- Second-line therapy: If NSAIDs or colchicine are ineffective or contraindicated then a short course of oral steroids or an intra-articular injection of steroids can be considered.
Prevention
Urate-lowering drugs should be discussed with all patients diagnosed with gout.
They should generally be initiated once an acute attack has resolved. In particular the following patient groups should be advised to commence urate-lowering drugs:
- Two or more attacks within 12 months
- Tophi
- Chronic gouty arthritis
- Arthropathy
- Renal impairment
- Renal calculi
- Young age onset
- Diuretic use
First-line therapy
- Medical therapy: Allopurinol is the first-line urate-lowering agent, it is a xanthine-oxidase inhibitor that prevents the conversion of hypoxanthine to xanthine and xanthine to uric acid.
- Monitoring: After allopurinol has been initiated, uric acid levels should be measured every four weeks and the dose of allopurinol can be uptitrated in relation to levels. Aim to bring uric acid levels under 300 micromol/L.
- Cautions: Care must be taken in renal impairment. Allopurinol may rarely cause a severe, at times life-threatening, hypersensitivity sydrome.
Second-line therapy
- Medical therapy: Febuxostat (xanthine oxidase inhibitor) may be used if allopurinol is contraindicated. Patients should have LFTs prior to and after commencing febuxostat, a known cause of acute liver injury.
- Monitoring: After febuxostat has been initiated, uric acid levels should be measured every four weeks and the dose of febuxostat can be uptitrated in relation to levels. Aim to bring uric acid levels under 300 micromol/L.
- Cautions: Care must be taken in renal impairment. It has been noted hypersensitivity to allopurinol and/or renal impairment may indicate hypersensitivity to febuxostat.
Prophylaxis against urate-lowering therapy induced acute gout
Clinicians should consider prescribing colchicine cover when starting (or increasing) urate lowering therapies such as allopurinol or febuxostat to prevent acute attacks. This may continue for six months.
NOTE: If already established on treatment, do not stop allopurinol / febuxostat during an acute attack.
Last updated: March 2021
Have comments about these notes? Leave us feedback
