Hyperkalaemia
Notes
Overview
Potassium is the most abundant intracellular cation, with a normal plasma concentration of 3.5-5.5 mmol/L.
Hyperkalaemia may be defined as a blood potassium level ≥ 5.5 mmol/L. It can represent a life-threatening emergency requiring urgent management. Hyperkalaemia can be further divided as follows:
- Mild: 5.5-5.9 mmol/L
- Moderate: 6.0-6.4 mmol/L
- Severe: ≥ 6.5 mmol/L
Physiology
Potassium is primarily an intracellular cation. Approximately 98% of potassium within the body is found within cells.
An adult has approximately 3,500 mmol of potassium. In the normal individual, a daily intake of 90 mmol/day is recommended by the World Health Organisation.
Cellular uptake of potassium is controlled by sodium-potassium adenosine triphosphatase pumps (Na+/K+ATPase). Its action is stimulated by (amongst others) sympathetic stimulation and insulin. Acidosis results in decreased cellular uptake of potassium as it is released in exchange for hydrogen ions.
Potassium is excreted by renal and extrarenal methods. Renal excretion is most significant, accounting for up to 90% of excretion.
Aetiology
There are four main categories of causes that lead to a rise in potassium concentration.
- Impaired excretion (i.e. renal)
- Increased intake
- Extracellular shift in potassium
- Pseudohyperkalaemia.
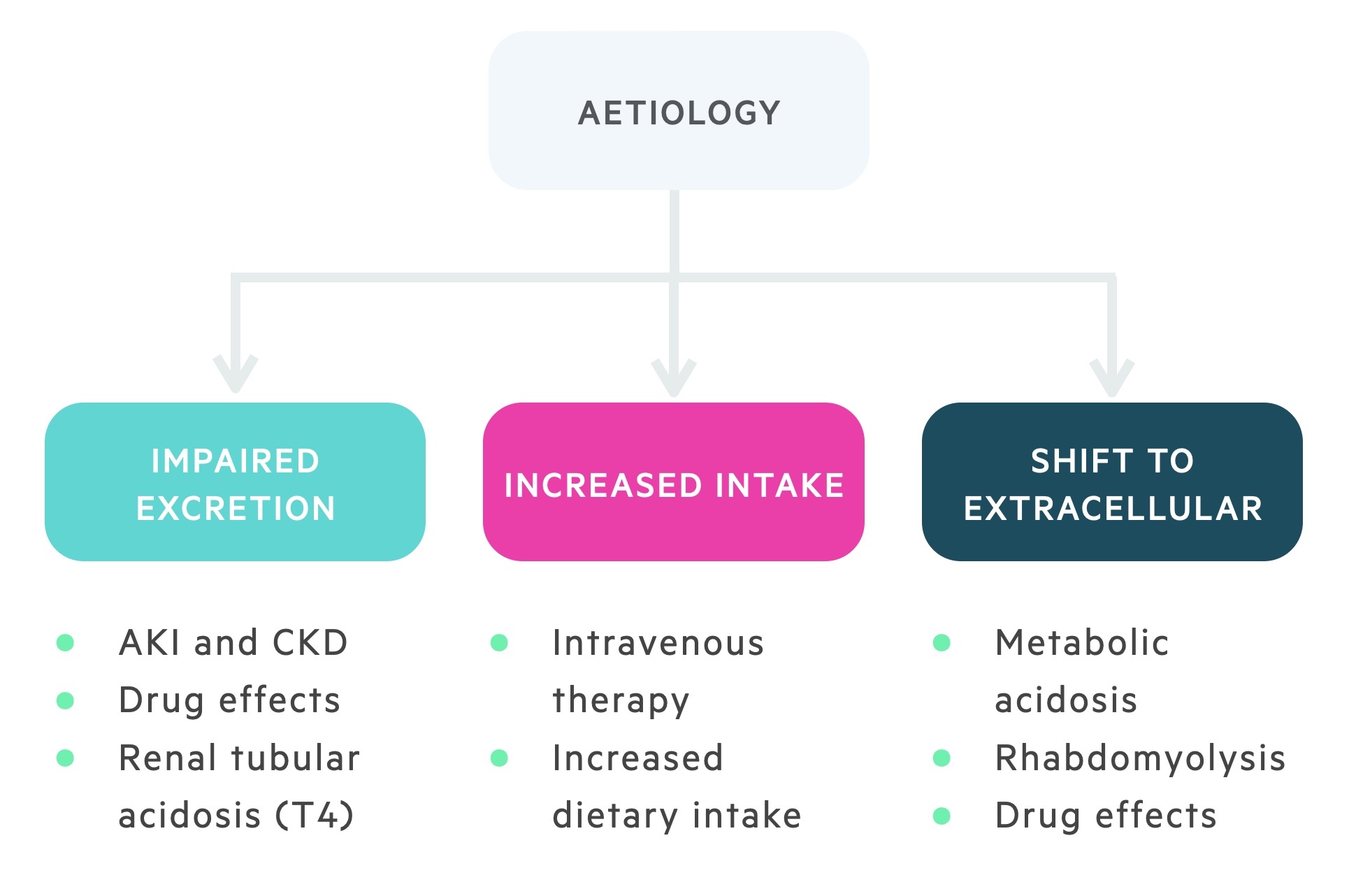
Impaired excretion
The kidneys are essential in the regulation of plasma potassium concentration with up to 90% of potassium excretion occurring via the kidneys. Therefore, damage to the kidneys or drugs that interfere with renal physiology can cause hyperkalaemia.
The major causes of impaired potassium excretion include:
- Acute kidney injury
- Chronic kidney disease
- Mineralocorticoid deficiency (i.e. a lack of aldosterone)
- Medications that inhibit aldosterone (i.e. spironolactone)
- Medications that affect autoregulation of renal blood flow (i.e. angiotensin-covering enzyme inhibitors, angiotensin II receptor blockers, non-steroidal anti-inflammatory drugs)
- Hyperkalaemic renal tubular acidosis (Type IV RTA)
- Other drugs (i.e. ketoconazole, digoxin, ciclosporin, tacrolimus)
Increased intake
A rise in plasma potassium concentration can occur due to increased potassium intake. This may be iatrogenic secondary to excess oral potassium supplements, an intravenous solution with potassium or blood products.
Extracellular shift in potassium
Potassium is predominantly an intracellular cation, in certain conditions potassium is shifted from the intracellular to extracellular space causing hyperkalaemia.
- Acidosis (including DKA)
- Tumour lysis syndrome
- Rhabdomyolysis
- Digoxin
- Burns
- Trauma
These tend to cause clinically significant hyperkalaemia in those with preexisting renal impairment.
Pseudohyperkalaemia
Pseudohyperkalaemia refers to a false or spurious elevation in potassium concentration.
Some of the common causes for a spurious potassium result include:
- Prolonged tourniquet time
- Haemolysed sample
- The length of storage of the specimen
- Marked leukocytosis (high white cell count) or thrombocytosis (high platelet count).
- Sample from a limb receiving potassium intravenously
Clinical features
Hyperkalaemia is frequently asymptomatic and therefore difficult to diagnosis without a laboratory sample.
On occasions, non-specific features may be present such as weakness and fatigue.
Symptoms
- Fatigue
- Generalised weakness
- Chest pain
- Palpitations
Signs
- Arrhythmias
- Reduced power
- Reduced reflexes
- Signs of the underlying cause (e.g. trauma leading to rhabdomyolysis)

Diagnosis & investigations
The diagnosis of hyperkalaemia is based on a laboratory sample of plasma potassium being ≥ 5.5 mmol/L.
In an emergency, a rapid assessment of electrolytes, such as potassium, can be achieved by completing a venous or arterial blood gas.
Other investigations that are important in the workup of hyperkalaemia are as follows:
- Urinalysis
- ECG (see below)
- Full blood count
- U&Es
- Bone profile
- VBG/ABG
- CRP
- Blood cultures (if febrile)
- CK (If rhabdomyolysis suspected)
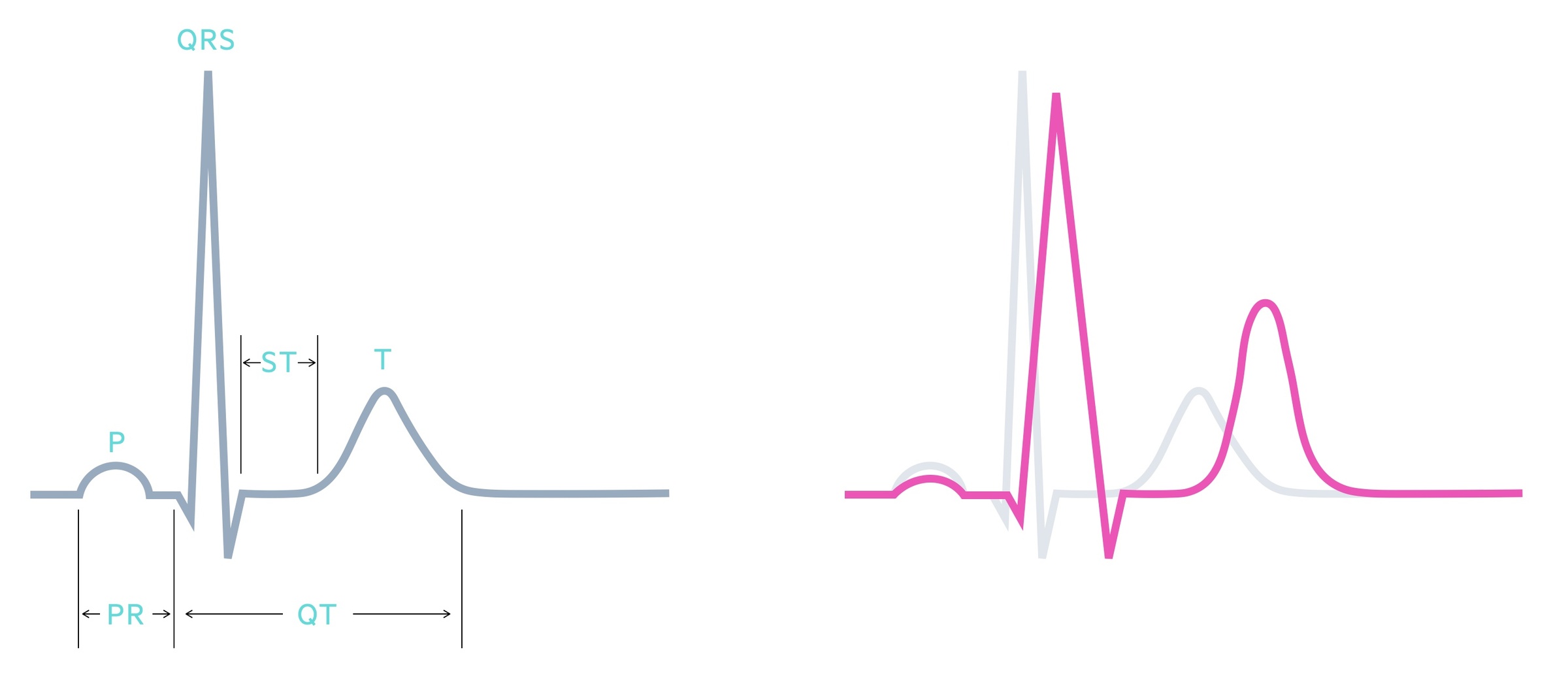
ECG changes
An ECG is an essential investigation in all patients with suspected hyperkalaemia because it can lead to life-threatening arrhythmias and cardiac arrest.
As hyperkalaemia progresses there are sequential changes that occur on the ECG. These generally correlate with the potassium level but can also reflect the rate of change - problems with cardiac conduction are more likely with acute changes in potassium concentration. An ECG should form part of the assessment of any patient with hyperkalaemia; mild, moderate or severe.
Typical changes on the ECG in patients with hyperkalaemia include:
- Peaked or ‘tall tented’ T waves
- Prolonged PR interval (> 200 ms)
- Widening of the QRS interval (> 120 ms)
- Small, or absent, P waves
- AV dissociation (no correlation between P waves and QRS complexes)
- Sine wave pattern (terminal sign)
- Asystole
Management
Hyperkalaemia is a common medical emergency. All patients should be assessed with respect to Airway, Breathing, and Circulation (ABC).
The treatment of hyperkalaemia generally depends on the plasma concentration of potassium and the presence or absence of ECG changes. Most trusts will have their own protocol for the management of hyperkalaemia, additionally, the resuscitation council's produces their own guidance.
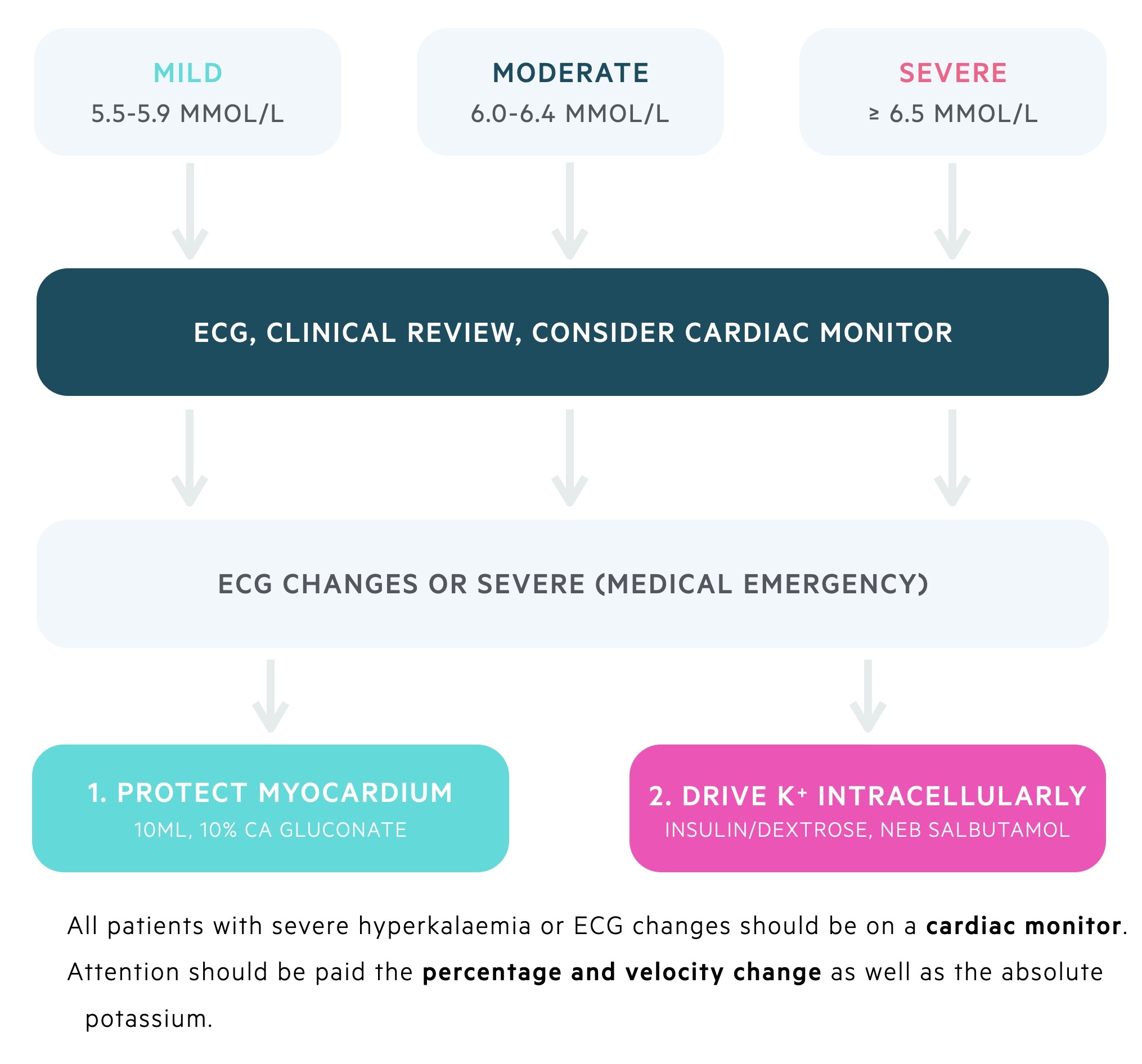
Initial assessment
- ABCDE assessment
- ECG
- Consider cardiac monitoring
- Stop any potassium-containing fluid or medication
Protect the myocardium
In patients with significant hyperkalaemia (i.e. > 6.5 mmol/L) or ECG changes, 10 ml of 10% calcium gluconate over 10 minutes should be given to protect the myocardium. This should improve changes on the ECG and is able to transiently stabilise the myocardium for 30-60 minutes.
Patients on digoxin are at risk of toxicity - follow local trust guidelines. Further calcium gluconate may be given at 5-minute intervals with a maximum of three doses.
Drive potassium intracellularly
Insulin is the main medication that is used to drive potassium intracellularly to cause a transient fall in plasma potassium concentration. It is usually given as 10 units of a short-acting insulin (e.g. ACTRAPID) alongside dextrose (e.g. 50 ml 50% or 100 ml 20%) over 30 minutes.
This combination is given intravenously and should lead to a reduction in potassium concentration by 0.5-1.0 mmol/L within 15 minutes. Plasma potassium should be checked 30 minutes following the infusion via a venous blood gas and formal U&Es checked 1-2 hours later. The patient's blood sugar should be monitored.
You may also give nebulised salbutamol. This leads to the activation of beta-receptors, which promotes the intracellular shift of potassium. Salbutamol can be given as back-to-back 5 mg nebulisers at a combined dose of 10-20 mg. This should reduce the potassium concentration by 0.5-1.0 mmol/L within 15-30 minutes.
Sodium bicarbonate may be given to those with acidosis (normally with pH < 7.2) to help normalise the potassium, this should only be commenced under the guidance of an experienced renal or critical care physician.
Potassium elimination
While the above treatments can stabilise the myocardium and drive potassium intracellularly, they are ineffective at eliminating potassium from the body. The only effective ways of eliminating potassium are:
- Loop diuretics (e.g. furosemide)
- Potassium-binding resins (e.g. Patiromer or sodium zirconium cyclosilicate)
- Haemodialysis
These are advanced treatments and can cause significant harm if given to the wrong patients so their use is senior-led. Furosemide may have a role in hyperkalaemia in patients with fluid overload. Haemodialysis is reserved for patients with refractory hyperkalaemia despite medical therapy. Modern potassium-binding resins are having an increasing role in the management of hyperkalaemia. Older resins (e.g. sodium polystyrene sulfonate) were limited by significant gastrointestinal side-effects and fell out of favour. Newer agents include Patiromer and sodium zirconium cyclosilicate that bind potassium in the gut. They are better tolerated and have a rapid onset of action (sodium zirconium cyclosilicate acts within 1 hour). They are commonly used in chronic hyperkalemia (e.g. chronic kidney disease) but they are being increasingly used in acute hyperkalaemia.
Ongoing management
Once initial management has been completed, the patient will require repeated 12-lead ECGs, and U&Es checked 4-6 hourly.
A medication review should be undertaken to look for any drugs known to cause hyperkalaemia and offending agents stopped. If hyperkalaemia is still an issue, acute treatment can be continued. Patients who are initiated on newer potassium-binding resins can continue them with close monitoring of potassium levels. It is important to note the dose of these medications changes after loading.
Refractory hyperkalaemia
In refractory cases, clinicians should liaise with the intensive treatment unit (ITU) for consideration of dialysis.
Last updated: December 2022
Have comments about these notes? Leave us feedback
