Chlamydia
Notes
Overview
Chlamydia is a common sexually transmitted infection caused by the bacterium Chlamydia trachomatis.
Chlamydia is considered the most common treatable bacterial sexually transmitted infection (STI). It is caused by the obligate intracellular bacterium Chlamydia trachomatis, which is also responsible for Lymphogranuloma venereum (LGV) and ocular infections.
The phrase ‘chlamydia’ is generally reserved for urogenital infections by C. trachomatis that is caused by certain serovars of the organism (D-K). Serovars are a way of groups organisms into species or subspecies based on the surface antigens.
The majority of chlamydia infections are asymptomatic (50% of males and ~70% of females). Untreated, chlamydia can cause significant long-term morbidity including pelvic inflammatory disease (PID) and infertility.
Epidemiology
Adults < 25 years old account for the majority of cases of chlamydia (~70%).
Chlamydia is a commonly acquired STI with >200,000 cases in both 2013 and 2014 reported by Public Health England (PHE). In 2019, 1.3 million chlamydia tests were completed in patients aged 15-24 years old with >130,000 positive cases.
Chlamydia is seen most commonly in those living in the most deprived areas. The rate of infection is similar amongst men and women, although women are more likely to be asymptomatic and have long-term complications.
Risk factors
Age <25 years old is a major risk factor for chlamydia.
- Age < 25 years
- New sexual partner
- Unprotected sexual intercouse
- ≥1 partner over last year
- Concurrent STI
- Previous STI
Aetiology & pathophysiology
Chlamydia is caused by the intracellular bacterium Chlamydia trachomatis.
C. trachomatis is considered a gram negative obligate intracellular bacteria. It is primarily transmitted through penetrative sexual intercourse with a transmission rate of 75%.
The majority of cases are asymptomatic (~50% men, ~70% women) and up to 50% of cases will resolve spontaneously within a year. The incubation period (time from acquisition to infection) is approximately 1-3 weeks.
Sites of infection
In men and transwomen, chlamydia infects the urethra. In women and transmen, it may establish infection in the cervix, urethra, uterine tubes or uterus. Depending on the site of acquisition of the bacterium, it may also infect the conjunctiva, pharynx and rectum.
If C. trachomatis infections ascends to infect the upper genital tract it is considered a ‘complicated infection’ and can lead to more serious complications:
- Women and transmen: causes pelvic inflammatory disease (PID). PID can cause systemic features, abdominal pain and lead to chronic scarring and infertility.
- Men and transwomen: causes epididymo-orchitis. Epididymo-orchitis can causes severe pain and swelling. It has been linked to infertily and hypogonadism (low testosterone levels).
Co-infection
A significant proportion of patients with chlamydia are co-infected with gonorrhoea. This is approximately 40% in women and 20% in men. It is therefore essential that patients are tested for both conditions.
Pathology
The natural history of chlamydia infection is poorly understood. Following transmission many patients remain asymptomatic and half of patients with spontaneously clear the infection.
C. trachomatis preferentially infects columnar epithelial cells such as those found at the squamous-columnar junction within the cervix. Here it initiates a local inflammatory response. Although an intracellular organism, it can survive in the extra-cellular environment as elementary bodies that are infectious particles of the bacterium. These bodies enter host cells and resist lysosomal destruction. They subsequently reorganise into reticulate bodies and undergo replication to infect more cells.
Serovars
C. trachomatis is divided into subspecies based on the antigens found on its surface. These subspecies are known as serovars and there are at least 15 known at present.
The serovars of C. trachomatis can cause a variety of infections in humans:
- Trachoma (A-C): contagious bacterial eye infection
- Urogenital (D-K): classic chlamydia infection
- LGV (L1-L3): genital ulcer disease
Clinical features
The majority of cases of chlamydia are asymptomatic.
Urogenital infections
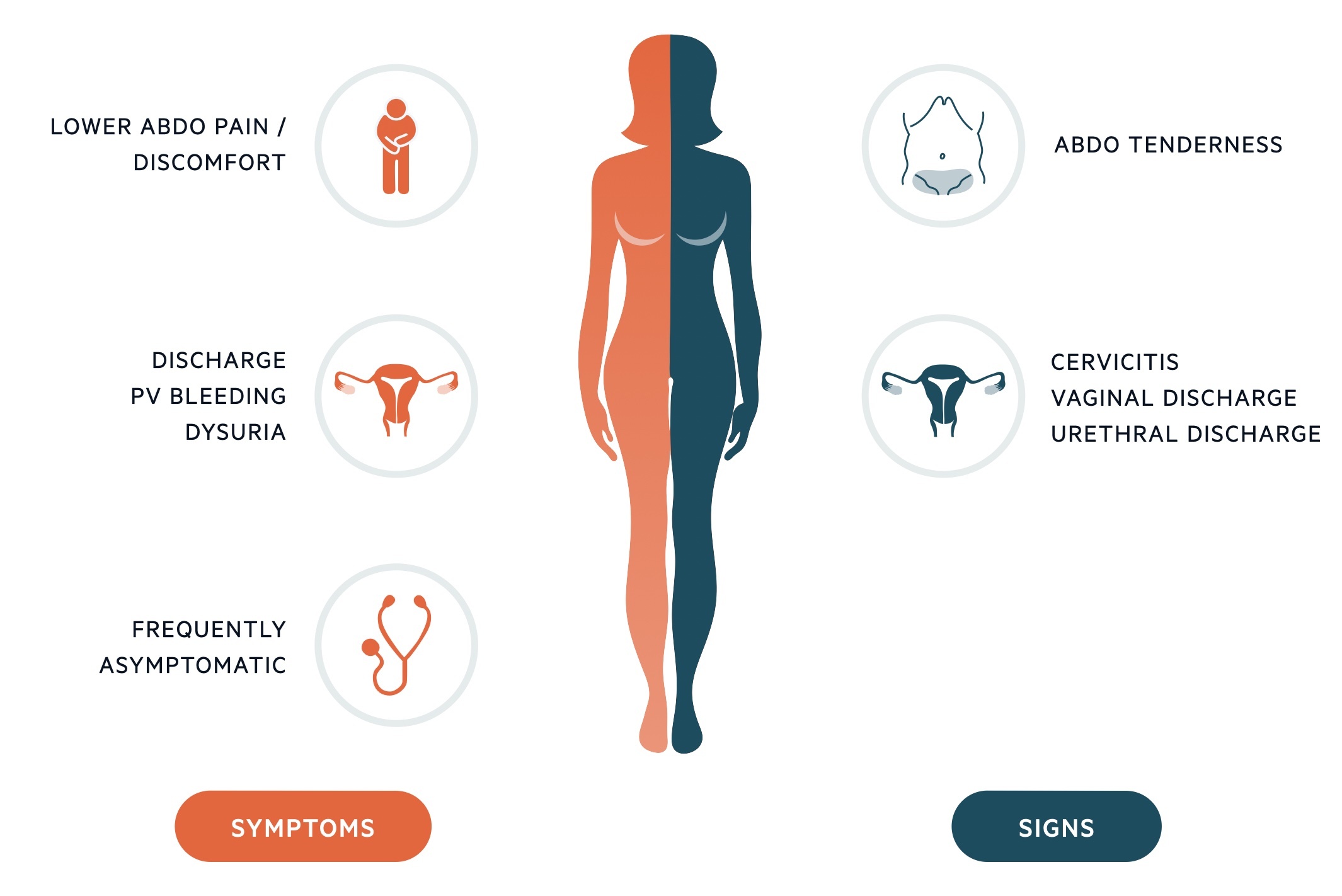
- Symptoms
- Women and transmen: vaginal discharge, post-coital bleeding, intermenstrual bleeding, dysuria, lower abdominal pain, deep dyspareunia
- Men and transwomen: urethral discharge, dysuria
- Signs
- Women and transmen: Cervicitis +/- mucopurulent discharge (on speculum examination), pelvic tenderness
- Men and transwomen: Urethral discharge
Cervical excitation refers to pain on movement of the cervix during vaginal examination. It is highly suggestive of PID.
Rectal infections
Most rectal infections are asymptomatic, but features can include
- Anal pain or discomfort
- Rectal discharge
Epididymo-orchitis
For more information see our notes on epididymo-orchitis.
Pelvic inflammatory disease
PID is a major complication of chlamydia. Up to 16% of patients with untreated infections are at risk. The risk of tubal infertility is 1-20% following PID.
Features include:
- Systemic upset: fever, malaise, anorexia
- Symptoms: low abdominal pain, abnormal vaginal bleeding, vaginal discharge or cervical discharge
- Signs: marked abdominal pain, cervical excitation, mucopurulent discharge
- Long-term complications: infertility, ectopic pregnancy, chronic pelvic pain
- Short-term complications: Tubo-ovarian abscess, Fitz-Hugh-Curtis syndrome (see below)
Fitz-Hugh-Curtis syndrome
This is a rare complication of PID in some patients that presents with right upper quadrant pain due to peri-hepatitis. More common with chlamydia, but also seen with gonorrhoeal PID. Analgesia, antibiotics and treating the underlying PID is key.
Diagnosis & investigations
Nucleic acid amplification tests (NAATs) are the main diagnostic tests for chlamydia.
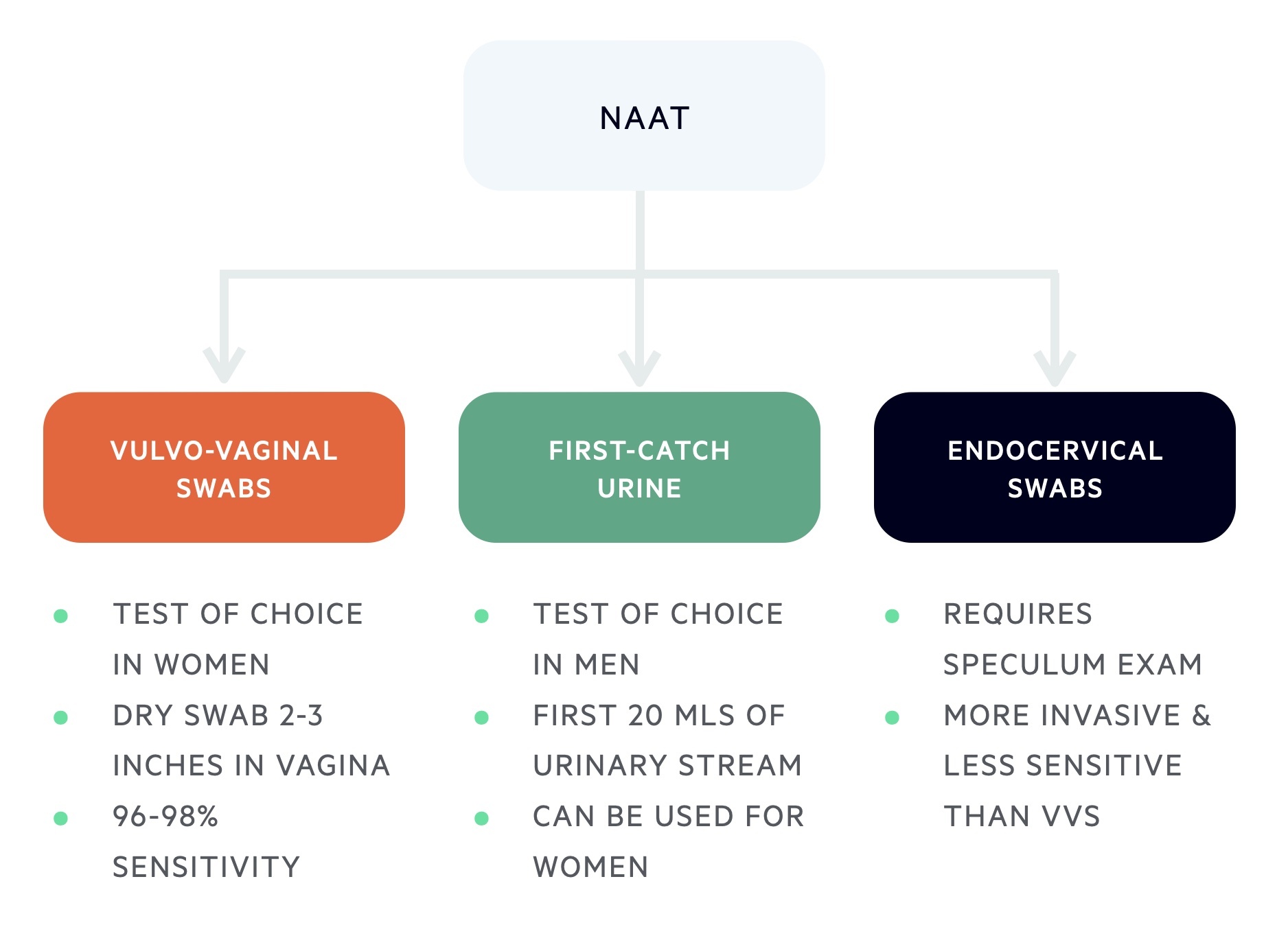
Diagnosis of chlamydia is based on a NAAT that can be completed on a first-catch urine sample or genital swab.
NAAT
NAATs are the most sensitive test for chlamydia and commercial kits are widely available. They detect chlamydia through amplification of any C. trachomatis genetic material from relevant samples.
- Vulvo-vaginal swabs (VVS): test of choice in women. Taken with a dry swab 2-3 inches into the vagina and rotating for 10-30 seconds (96-98% sensitivity).
- Endocervical swabs: requires a speculum examination and swab taken from the endocervix. More invasive and less sensitive than VVS.
- First-catch urine (FCU): test of choice in men. The First 20 mls of urinary stream collected and analysed. Better or equivalent to urethral sampling. Can be completed in women but less sensitive compared to VVS.
- Urethral swabs: good results, but superseded by urine samples and VVS.
- Extra-genital swabs: the rectum, pharynx and other extra-genital sites can all be appropriately swabbed.
If the initial test is negative, but there has been significant sexual exposure in the last two weeks, the patient will need a repeat test in two weeks.
Other investigations
Patients with suspected chlamydia require referral and assessment at a genitourinary medicine (GUM) clinic. This enables a full sexual health screen including testing for other STIs such as Gonorrhoea, syphilis and HIV. Home testing kits for these common STIs are now available.
Management
A seven day course of doxycycline is an effective treatment for chlamydia.
General advice
Patients should be advised to avoid sexual contact until both themselves and partners have completed treatment. If they have received single dose therapy, they need to wait a minimum of 7 days.
Contact tracing
Contact tracing should be completed with advice from a GUM clinic. It is recommended that all contacts within the last four weeks for men or transwomen with urethral symptoms or all contacts within the last six months for all other cases (asymptomatic patients, symptomatic women or transmen). Notified partners should be encouraged to undertake a full sexual health screen.
Test of cure
This refers to repeat testing after the course of treatment. Routine test of cure (TOC) is not required in uncomplicated cases. Test of cure is recommended in patients with suspected poor compliance, pregnancy, rectal infections or ongoing symptoms. Generally performed not less than three weeks following treatment.
Repeat testing
Patients < 25 years old who are diagnosed with chlamydia should be offered a repeat chlamydia test in 3-6 months. This is because there is a higher risk of reinfection (2-6x higher), which also increases the risk of PID and infertility.
Pharmacological management
Treatments for chlamydia depend on whether the infection is complicated or uncomplicated, the site of infection, and co-morbidities (e.g. HIV co-infection, pregnancy).
In uncomplicated urogenital infections, Doxycycline is generally the first line, which is given over 7 days, and azithromycin is a second-line treatment. However, in pregnancy, azithromycin is preferred because tetracyclines are contra-indicated.
Complicated infections
Patients with PID or epididymo-orchitis should be treated according to local guidelines and may require inpatient admission for intravenous antibiotics. Local guidelines and specialist advice should always be sought.
Complications
Untreated, chlamydia can lead to long-term complications including infertility.
- Pelvic inflammatory disease
- Peri-hepatitis (Fitz-Hugh-Curtis syndrome)
- Endometritis
- Ectopic pregnancy
- Tubal infertility
- Sexually acquired reactive arthritis (SARA)
Last updated: October 2024
Further reading
British Association for Sexual Health and HIV (BASHH) guidelines.
Have comments about these notes? Leave us feedback
