Pediculosis pubis
Notes
Overview
Pediculosis pubis refers to pubic lice and it is due to infection by Phthirus pubis (crab louse).
Pediculosis pubis, or pubic lice, is more colloquially known as ‘crabs’ due to infection by the crab louse called Phthirus pubis. P. pubis is one of three types of lice than can infect humans.
- Phthirus pubis: crab louse. Infects the pubic region.
- Pediculosis humanus capitis: head louse. Infects the head.
- Pediculosis humanus corporis: body louse. Infects different regions of the body.
Due to the location, pediculosis pubis is usually sexually transmitted although the lice can extend to other parts of the body, including eye lashes (pediculosis ciliaris).
Epidemiology
Pediculosis pubis is most commonly seen in teenagers and young adults.
There has been a general decrease in the incidence of pediculosis pubis, which may be due to the increase in people choosing to remove pubic hair.
Aetiology & pathophysiology
Pediculosis pubis is caused by the crab louse, which is 0.8-1.2 mm in size.
The crab louse is a small parasite that is translucent and attaches to the pubic hair via its legs.
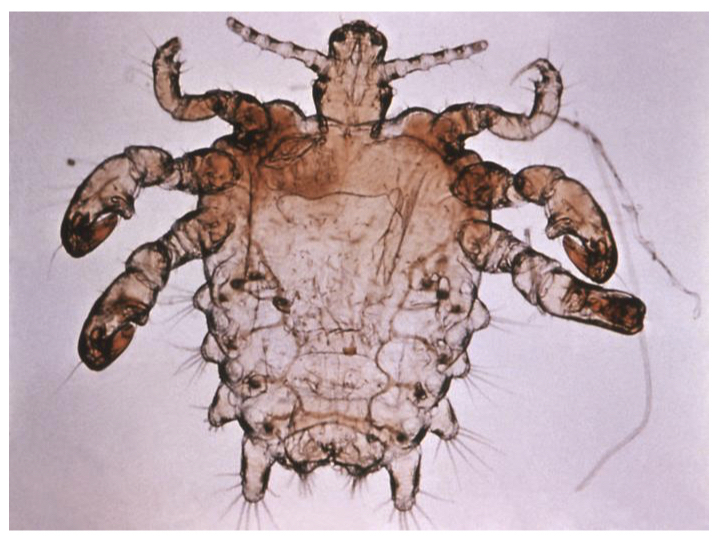
Crab louse. Courtesy of CDC.
A female crab louse can survive for 3-4 weeks. During this time it is able to lay up to three eggs per day, which hatch after 6-8 days. These eggs are known as ‘nits’ and attach firmly to the base of hairs.
Direct contact with an infected areas (genital region or contaminated clothing) leads to transmission.
Clinical features
Pediculosis pubis is characterised by pruritus (itching).
Signs and symptoms
- Pruritus
- Visible lice
- Small bluish macules (0.5-1.0 cm): due to prolonged infestation and injection of natural anticoagulant from lice saliva during feeding.
- Lymphadenopathy (rarely)
Typical sites
- Pubic hair
- Perianal area
- Other: Axilla, Eyebrows, Chest hair
Diagnosis
Diagnosis is based on identification of crab lice or nits (eggs).
Direct visualisation with the naked eye or microscopic examination can be used to identify the lice/nits.
Important to consider and screen for other sexually transmitted infections (STIs) including chlamydia, gonorrhoea, HIV and syphilis as appropriate. In children, presence of pubic lice may be a sign of sexual abuse, which needs further investigation.
Management
Topical permethrin is the treatment of choice for pediculosis pubis.
General advice
Topical therapy alongside removal of lice/nits with a nit comb should be completed as part of standard management. There is no requirement to shave hair of affected area if therapy advice is followed.
Contact tracing should be completed for all sexual parters within 3 months of the onset of symptoms. Partners should be examined for infestation and treated as necessary. Patients should abstain from sexual contact until they have been treated and reassessed to ensure infestation has resolved.
Bedding and environment
Bedding and clothing of infected patients should be appropriately washed. This means washing any item used within the last 2-3 days prior to treatment in a washing machine with hot water followed by hot dryer. Aim for temperature >54º.
If unable to wash clothes and bedding, items can be placed in sealed bags for 48 hours. Lice will die within 48 hours after removal of the host.
Topical treatments
The two topical treatment options include permethrin 1% cream and pyrethrins 0.33% with piperonyl butoxide 4%. Permethrin works by inhibiting sodium ion influx in neuronal membranes of parasites that leads to paralysis and death.
Methods for application include:
- Ensure affected area is cool and dry
- Apply to affected site
- Wash after 10 minutes
- Remove nits/lice with comb (alternatively can use fingernails or tweezers)
- Put on clean clothes post treatment
Re-treatment is recommended routinely in 7-10 days time.
Oral treatments
Rarely oral treatment is needed. The main option is Ivermectin given at 200 mcg/kg as two single doses seven days apart. Ivermectin interrupts with chloride channels on nerve and muscle cells leading to paralysis and death.
Last updated: June 2021
Have comments about these notes? Leave us feedback
