Vulvovaginal candidiasis
Notes
Overview
Vulvovaginal candidiasis or ‘genital thrush’ refers to a superficial fungal infection of the vulva and/or vagina.
Vulvovaginal candidiasis, or ‘thrush’, is a very common condition. Thrush is caused by a candidia infection and leads to a characteristic thick white discharge with symptoms or vulval and/or vaginal itching/soreness. Thrush is easily treated with over the counter anti-fungal creams.
Classification
Genital thrush can be divided into two types:
- Uncomplicated: refers to mild/moderate cases, which are sporadic or infrequent. This cases are due to C. albicansin patients without major co-morbidity (e.g. HIV, poorly controlled diabetes, non-pregnant).
- Complicated: refers to recurrent (≥4 episodes/year) and/or severe infection. In addition, considered complicated if caused by a Candida species other than C. albicans or in patients with major co-morbidity (e.g. HIV, poorly controlled diabetes, pregnancy).
Epidemiology
Vulvalvaginal candidiasis is a very common cause of vaginitis.
It is difficult to assess the true prevalence of thrush because many patients self-treat their condition. In addition, up to 20% of healthy women have asymptomatic carriage of candida.
In one cohort, 75% of women reported at least one episode of thrush during their lifetime and up to 45% reported two or more episodes.
Aetiology & pathophysiology
Vulvovaginal candidiasis is most commonly caused by the yeast Candida albicans.
C. albicans is the most common cause of thrush seen in up to 92% of cases. Other species of candida can cause thrush, which include:
- C. glabrata (5%)
- C. tropicalis
- C. parapsilosis
- C. krusei
- Others
Candida species are able to cause a superficial infection by infiltration of the vaginal epithelium leading to inflammation. Alteration in vaginal pH, sex hormones, sexual activity or even foreign bodies (e.g. contraceptive device) may disrupt the balance between candida and host immune response leading to overgrowth and superficial infection.
Up to 20% of women may be colonised with Candida but remain completely asymptomatic. How the condition transforms from asymptomatic carriage to superficial infection depends on both the host immune response and virulence factors within candida species
Risk factors
Patients with poorly controlled diabetes are at increased risk of vulvovaginal thrush.
- Oestrogen exposure: incidence rises after menarche. Rarely seen in post-menopausal women without other risk factors.
- Immunocompromised state (e.g. systemic corticosteroids)
- Poorly controlled diabetes mellitus
- Broad-spectrum antibiotic use: alters the vaginal flora
- Local irritants (e.g. vaginal hygiene products)
- Sexual activity: not a sexually transmitted infection (STI), but may be triggered by sex
- Hormone replacement therapy (HRT)
Clinical features
Vaginal thrush is characterised by a thick white discharge and vulvovaginal irritation.
The clinical history is usually enough to make a diagnosis of vaginal thrush. A formal examination using a speculum is usually not required, but consider if an alternative diagnosis is suspected or thrush is recurrent/severe.
Symptoms
- Vaginal itching
- Vaginal soreness
- Vaginal discharge: characteristically thick and white (‘cheese-like’). Non-malodorous
- Superficial dyspareunia
- Dysuria
Signs
- Vulvovaginal irritation: erythema affecting the vulva that can extend to the labia majora and perineum
- Vaginal fissuring
- Excoritation (scratching)
Diagnosis
The diagnosis of candidiasis is usually made on the history alone and further investigations are not required.
Investigations are usually not required in acute, uncomplicated vaginal thrush and the diagnosis can be made on history alone.
Differential diagnosis
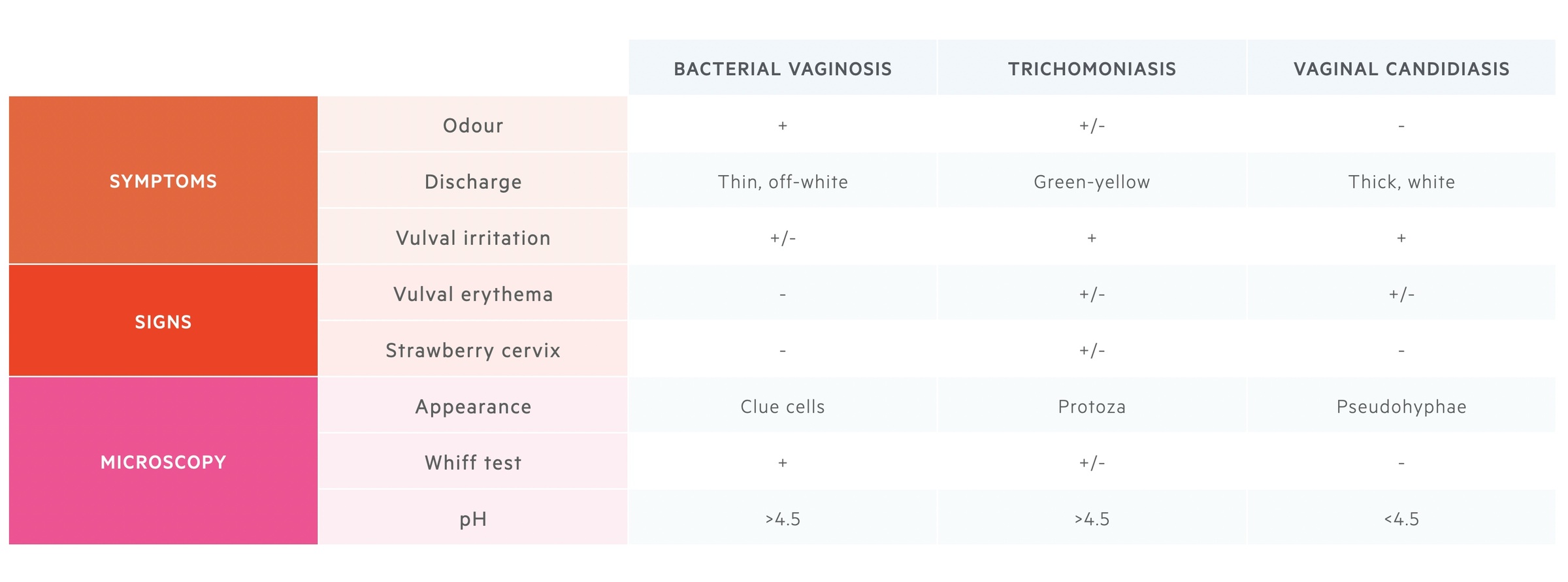
Other conditions such as trichomoniasis and bacterial vaginosis (BV) may present similarly to thrush. BV typically presents with an odorous discharge but without itching or soreness. Trichomoniasis usually presents with a green-yellow discharge and soreness. Trichomoniasis is considered an STI. Remember there could be co-infection and samples are usually required to differentiate between these pathologies.
Investigations
Investigations may be required in patients where an alternative diagnosis is suspected or thrush is severe, recurrent or chronic.
It is important to consider screening patients for high-risk sexual behaviour and need for a formal sexual health screen at a genitourinary medicine (GUM) clinic.
If further investigations are needed, this should start with a formal assessment and speculum examination at the bedside. Swabs can be taken at the time of examination.
Bedside
- Vulval examination (external female genitalia): assess for lesions, discharge, ulcers and inflammation.
- Speculum examination: visualise the cervix and vaginal walls. Take high vaginal swabs.
Vaginal discharge testing
Samples should be taken from the lateral wall and tested for pH using a low-range pH paper. Normal vaginal pH in women of child-bearing age is 3.5-4.5. Can help differentiate between thrush, bacterial vaginosis (BV) and trichomoniasis.
Samples can be checked for Clue cells by using microscopy. Clue cells refer to vaginal epithelial cells that have many coccobacilli adherent to their surface. This gives cells a studded appearance with a less sharply defined border. This suggests co-infection with bacterial vaginosis.
Microbiology
- High vaginal swabs: taken for gram stain and to rule out other causes (e.g. STI testing). Can be used in recurrent cases to assess for candida species and resistance patterns. Swab can be completed blind by the patient. May require a specific request to assess for non-candida species.
- Mid-stream urine (MSU): to exclude urinary tract infection if features consistent.
Bloods
- HIV: consider as part of a sexual health screen in severe or recurrent cases.
- HbA1c: consider in severe or recurrent cases.
STI screen
Consider testing for the following STIs and referring as necessary to a GUM clinic among patients who are considered high-risk:
- Chlamydia
- Gonorrhoea
- Trichomoniasis
- HIV/syphilis
Management
Genital thrush is treated easily with over the counter anti-fungal creams.
Treatment recommendations
The treatment of thrush depends on whether it is complicated or uncomplicated. All women should be provided with self-management advice on hygiene and washing.
- Uncomplicated
- Intravaginal anti-fungal cream, pessary (e.g. clotrimazole 10% cream as single dose or clotrimazole pessary for 2 nights), or oral anti-fungal agents (e.g. fluconazole as a single dose)
- Complicated
- Oral anti-fungal agents or intravaginal anti-fungal pessary, but both at a higher dose than in uncomplicated infections
- Extended courses considered in patients who are immunosuppressed (e.g. HIV)
Topical agents may be added for patients with vulval symptoms.
NOTE: in girls aged 12-15 years old, consider topical clotrimazole rather than intravaginal or oral preparations. Alternatively, seek specialist advice.
Treatment failure
In patients with uncomplicated vaginal thrush who fail to respond to treatment within 7-14 days, it is important to:
- Confirm treatment course and adherence
- Reassess risk factors (e.g. HbA1c and diabetes mellitus)
- Consider alternative diagnosis (e.g. BV): may require examinations and vaginal swabs
- Consider alternative treatment: alternative drug, preparation or extended treatment course
Recurrent episodes
Recurrent vulvovaginal candidiasis is defined as ≥4 episodes per year. In the presence of recurrent thrush consider an alternative diagnosis, undertake a formal assessment including speculum examination and swabs and reassess for risk factors (e.g. diabetes mellitus).
Treatment of recurrent thrush should involve:
- Induction course: oral anti-fungal (e.g. fluconazole) or 10-14 day course of anti-fungal pessary
- Maintenance course: oral anti-fungal or anti-fungal pessary given as needed if symptoms recur. Alternatively, give a six month maintenance course then review.
Genital thrush in pregnancy
Patients with thrush during pregnancy should avoid oral anti-fungal treatments. Topical and intravaginal pessaries can be used, typically for a more extended period (e.g. 7 days).
Specialist referral
Consider referral to a specialist (GUM/Gynaecology) in the following situations:
- Aged 12–15 years
- Diagnosis doubtful
- Treatment failure or ongoing symptoms
- Non-albicans candida
Complications
Treatment failure can occur in up to 20% of patients.
Treatment failure is defined as ongoing symptoms despite 7-14 days of treatment if uncomplicated. Patients with thrush may develop psychosocial problems, particularly if recurrent and there is an increased risk of balanitis in male partners (infection of the glans penis).
Last updated: March 2021
Further reading
British Association for Sexual Health and HIV (BASHH) guidelines.
Have comments about these notes? Leave us feedback
