Menopause
Notes
Overview
Menopause is the natural cessation of menstruation due to loss of ovarian follicular activity.
It most commonly occurs between the ages of 45 - 55 with a mean age of 51. As hormonal levels change, many will experience irregular periods and vasomotor features (e.g. hot flushes). This is followed by the cessation of menstruation.
There are a number of key terms that students should be aware of:
- Premature menopause: in some women, menopause occurs early for a myriad of reasons. If it occurs prior to 40 it is termed premature menopause.
- Perimenopause: occurs prior to menopause and is characterised by an irregular menstrual cycle and vasomotor symptoms.
- Postmenopause: describes the time after periods have ceased for 12 months.
Physiology
Menopause is a naturally occurring phase of a women’s life.
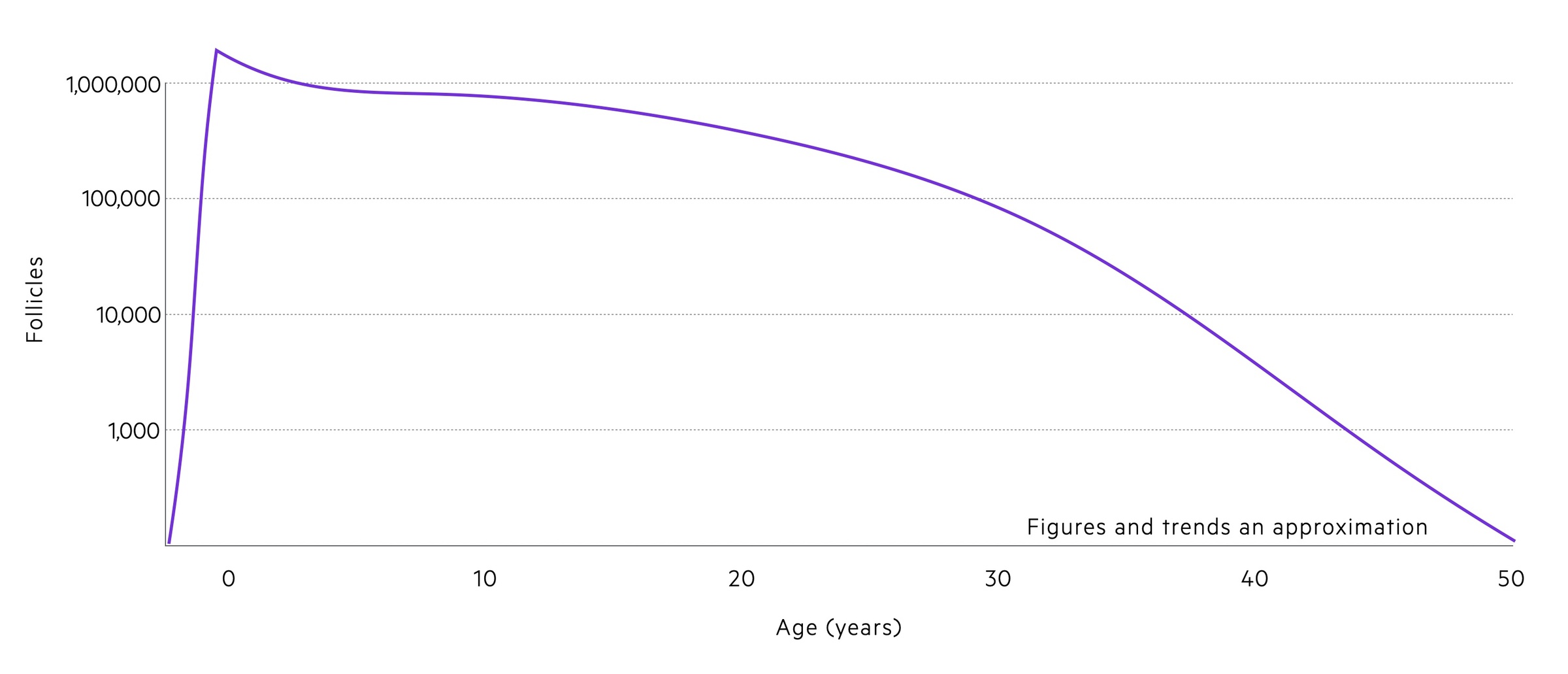
The number of oocytes in each women’s ovaries is fixed during the foetal period. It is at its peak at around 20-28 weeks gestation and falls with each menstrual cycle.
As the supply of oocytes falls, follicular activity falls. This results in a marked reduction in oestrogen and inhibin. As a result, negative feedback on the pituitary is alleviated resulting in increased levels of LH and FSH.
The decrease in oestrogen also results in the development of vasomotor symptoms including flushing and sweats and further disruption of the normal cycle. As anovulatory cycles occur estradiol (an oestrogen hormone) production fails, preventing thickening of the endometrial lining and resulting in amenorrhoea.
These changes result in a permanently lowered level of oestrogen and high levels of both FSH and LH.
Features
The perimenopause phase is characterised by menstrual irregularity and vasomotor symptoms.
Menstrual irregularity
Irregular cycles often last several years, with cycles becoming longer, shorter or variable. Periods may become heavier for a time. In a small proportion of women, periods come to an abrupt halt.
Vasomotor symptoms
These are common and may be the first symptoms noticed. They normally last several years with a median duration of 7. Symptoms include:
- Hot flushes
- Night sweats
Each woman is affected differently, some experience none or very mild symptoms whilst others suffer from debilitating episodes. In the US, studies have shown African-American women are more likely to suffer from vasomotor symptoms.
Urogenital symptoms
- Vaginal dryness
- Dyspareunia
- Urinary tract infections
Other
- Anxiety/depression
- Difficulty concentrating
- Sleep disturbance
- Reduced libido
- Musculoskeletal pains
Diagnosis
In healthy women over the age of 45, the diagnosis of menopause can be made based upon clinical features.
NICE guidance advises menopause can be diagnosed in healthy women over the age of 45 with:
- Perimenopause based on vasomotor symptoms and irregular periods
- Menopause in women who have not had a period for at least 12 months and are not using hormonal contraception
- Menopause based on symptoms in women without a uterus
In this group of healthy women over the age of 45, blood tests are not routinely required.
Hormone replacement therapy
HRT may help with many symptoms of menopause but have a number of side-effects patients should be counselled on.
HRT has been shown to help with vasomotor symptoms, mood changes and urogenital symptoms that may occur secondary to menopause.
Types of HRT
HRT may be given as ‘unopposed’ oestrogen or as a combination of oestrogen and progesterone. They can be offered in an oral or transdermal form. The choice is dictated by the presence or absence of a uterus:
- Women with a uterus: combined oestrogen and progesterone HRT
- Women with a without uterus: oestrogen-only HRT. Oestrogen-only HRT increases the risk of endometrial cancer so should never be used in women with a uterus.
Topical HRT is also available. Typically this is used to help with vaginal dryness.
Benefits and risks
Breast cancer: combined HRT (oestrogen and progesterone) is associated with an increased risk of breast cancer. Oestrogen monotherapy is associated with no or a very small increased risk. Importantly research shows HRT does not increase the chances of dying from breast cancer. HRT should not be routinely offered to those with a history of breast cancer or who are at elevated risk. These patients should be discussed with specialists.
Ovarian cancer: there appears to be a relatively small increased risk of ovarian cancer from HRT.
Venous thromboembolism: there is an increased risk of VTE with oral HRT when compared to the baseline population. However, there does not appear to be an increased risk of VTE with transdermal HRT use at normal doses.
Coronary heart disease: HRT appears to have a minimal or no improvement in the risk of CHD and does not impact the risk of death from CHD in women under the age of 60. Oestrogen alone has been associated with no or reduced risk of CHD whilst combination therapy is associated with no or minimal increase in risk.
Stroke: oral oestrogen is associated with an increased risk of stroke though this is small. Transdermal oestrogen does not appear to cause this.
Osteoporosis & MSK health: the risk of fragility fractures is reduced whilst taking HRT. There is some evidence it may help increase muscle mass and strength.
Management
Care should be centred around each individual patient and their needs.
Medical input may or may not be needed during the perimenopause and menopause period. Clinicians should be guided by the experience, wants and needs of each individual woman. These may change with time as the symptoms each person experiences develop.
Patients should have regular review after starting new medications and at least annually once symptoms are stable. Discuss the national health screening programmes (e.g. Breast and Cervical cancer) and the importance of attending. In those in whom symptoms do not improve, have contraindications to HRT or other concerns exist, referral to specialist care should be made.
Lifestyle modifications
Exercise can help with vasomotor symptoms, low mood and anxiety. Vasomotor symptoms may also be improved by sleeping in a cool room and wearing looser clothing. Where appropriate, weight loss can be advised.
Good sleep hygiene helps not only with sleep itself but mood disturbances and lack of concentration.
Contraception
Women should be advised HRT will not act as contraception. In addition, they may be fertile:
- Under 50: at least two years after their last period
- Over 50: at least one year after their last period
As such, if needed contraception should be continued to cover this period.
Specific symptomatic management
Vasomotor symptoms: hormone replacement therapy (HRT) can be offered to women with vasomotor symptoms after appropriate discussions. Lifestyle modifications as discussed above can also be of help.
Urogenital atrophy: vaginal oestrogen should be offered including to patients on systemic HRT. If symptoms do not improve or for women in whom systemic HRT is contraindicated, NICE advise discussion with a healthcare professional with appropriate expertise. Any women using vaginal oestrogen should report any ‘unscheduled’ vaginal bleeding to their GP.
Psychological symptoms: NICE describe a number of therapeutic options to help with these symptoms. Patients thoughts and feelings should be carefully explored and any suicide or self-harm risk promptly escalated and discussed with the relevant services. Symptoms of low mood that arise from menopause may benefit from HRT or cognitive behavioural therapy. Of course, depression and other psychological illness may occur independently to (and be exacerbated by) the menopause. Guidance for each independent condition should be followed.
Last updated: June 2021
Further reading
- NICE guideline NG 23: Menopause: diagnosis and management
- NICE guideline NG101: Early and locally advanced breast cancer: diagnosis and management
Have comments about these notes? Leave us feedback
