Cataracts
Notes
Overview
Cataracts occur due to opacification of the lens and are a major cause of blindness worldwide.
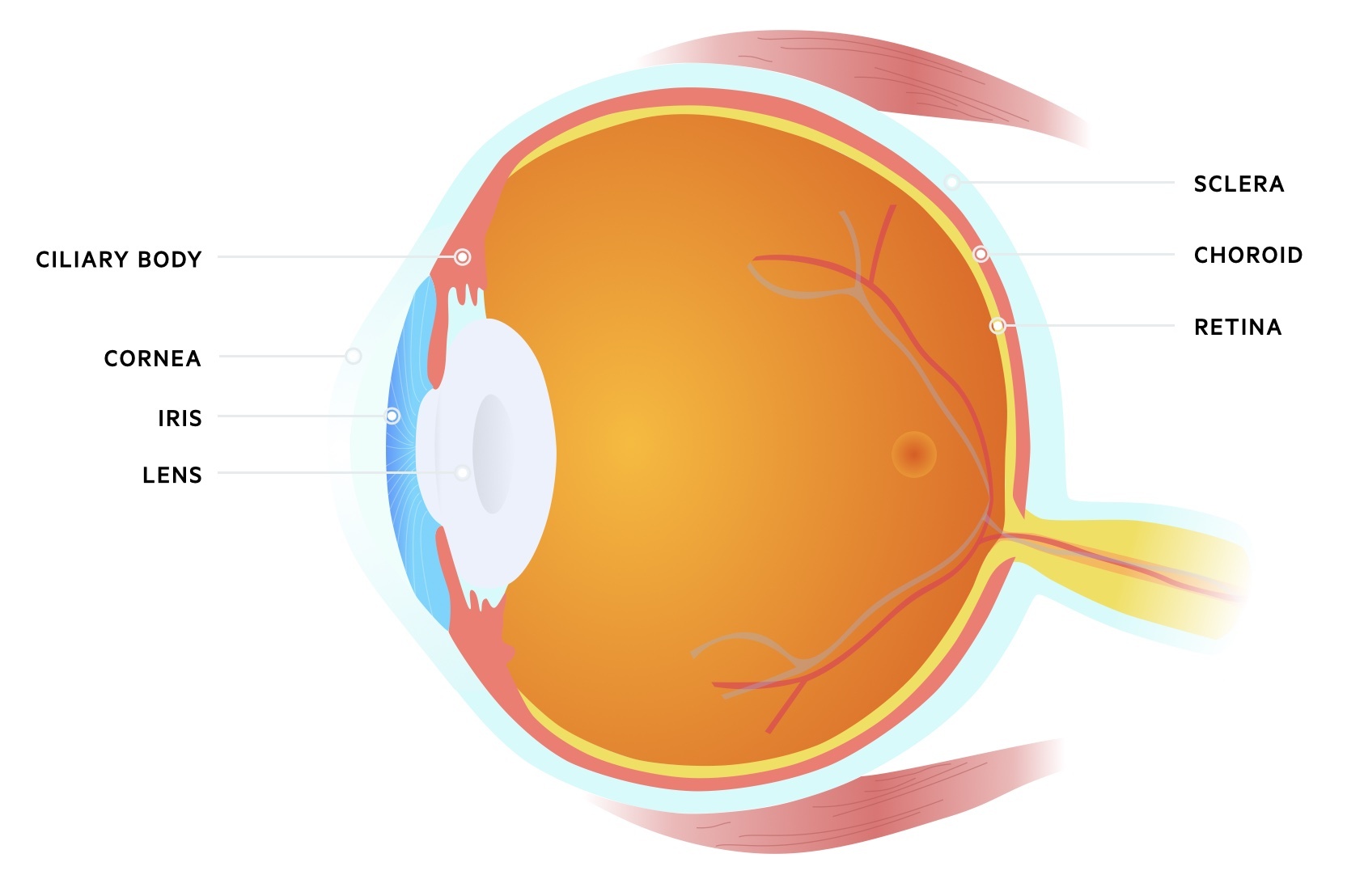
The lens is a clear, biconvex structure situated in the anterior portion of the eye. It lies posterior to the iris but anterior to the vitreous body. It is composed of a capsule, epithelium, cortex and nucleus. It is held in place by the suspensory ligaments that are attached to the ciliary bodies.
The lens is needed for normal vision and plays an important role in refraction and accommodation:
- Refraction: refers to the change in direction of light when it passes from one medium to another. Helps to converge light onto the retina.
- Accommodation: refers to the ability to maintain focus on an image as distance varies. The lens achieves this by altering its shape through contraction or relaxation of the ciliary bodies.
In cataracts, there is opacification of the normal lens that can be unilateral or bilateral. Worldwide, cataracts is a major cause of blindness but very treatable condition. This is because the diseased lens can be replaced with an artificial one through a simple surgical operation. This operation is the most common elective procedure in the UK.
Epidemiology
Cataracts is much more common as we age.
In one UK cohort, >70% of patients over 85 years old had visually-impairing cataracts. The estimated global prevalence in patients >60 years old worldwide is >50%.
Cataracts in adults
Cataracts is a major cause of blindness among older adults.
Cataracts is frequently seen as part of normal ageing. Cataracts associated with ageing is referred to as ‘age-related cataracts’ or ‘senile cataracts’ . However, the latter term is largely outdated.
In adults, other causes of cataracts are referred to as ‘non-age-related’. These include:
- Trauma
- Uveitis: inflammation of the uvea, which refers to the pigmented layers known as ciliary bodies, choroid and iris.
- Scleritis: inflammation of the sclera
- Intra-ocular tumours
- Radiation
- Medications (e.g. corticosteroids)
- Systemic disease (e.g. diabetes mellitus, myotonic dystrophy, severe atopic dermatitis)
Cataracts in children
Cataracts may be congenital (present from birth) or develop during childhood.
Cataracts may occur in children. The prevalence of congenital cataracts is estimated at 1-3 per 10,000 in developed countries. Congenital cataracts is usually present from birth (or develops within the first year of life) whereas developmental cataracts occurs during childhood.
Causes of cataracts in children can broadly be divided into three groups:
- Inherited (~1/3rd): often autosomal dominant, but various inheritance patterns exist
- Systemic disease (~1/3rd): multiple conditions. Examples include intrauterine infections (e.g. rubella), metabolic syndromes (e.g. Fabry disease) or craniofacial syndromes (e.g. Crouzon syndrome).
- Idiopathic (~1/3rd): idiopathic means the cause is unknown.
Cataracts in children is not reviewed further in this note.
Classification
There are different types of cataracts depending on the location of the lens affected.
- Nuclear: primarily involves the central nucleus of the lens. Clinically there is central opacification, significant loss of colour and slow progression.
- Cortical: primarily involves the cortex of the lens. Less degradation of vision and slow progression.
- Posterior subcapsular: involves the subcapsular cortex. Causes disabling glare to bright lights and has a quicker progression. Linked to diabetes mellitus and corticosteroid use.
Pathophysiology
The lens is composed of the soluble protein crystallin, which is important in the refraction of light.
The lens has a unique and highly organised structure. The tight packing of proteins, including crystallins, are important for its transparency. Overtime, this transparency can be lost due to the process of normal ageing but the precise mechanism is unknown.
Due to the lack of blood supply, containment within a capsule and inability to shed non-viable cells, this means the lens is susceptible to damage from normal ageing and environmental insults (e.g. UV light and oxidative stress). Collectively, this contributes to the loss of transparency as the central nucleus may become compressed, hardened and undergo nuclear sclerosis, which is seen clinically as opacification. Without transparency, light is unable to be refracted onto the retina to enable vision.
The underlying mechanism leading to opacification and loss of transparency may differ depending on the aetiology, especially among causes of non-age-related cataracts.
Clinical features
The hallmark of cataracts is painless loss of vision.
Symptoms
- Visual loss: usually described as loss of acuity
- Blurred vision
- Poor night vision
- Sensitivity to light and glare
- Seeing ‘Halos’ around lights
- Polyopia: refers to visualising multiple images
- Reduction in colour intensity: mainly noticed in blues
- Changes in glasses prescription
NOTE: With increasing opacification there may be an improvement in nearsightedness, but deterioration in longsightedness. This is due to the effect of the opacification on the refractive power of the lens, often termed ‘myopic shift’.
Signs
- Reduced visual acuity: tested by Snellen charts
- Loss of red reflex: seen during direct ophthalmoscopy
- White/grey pupil: due to opacification
- Nystagmus
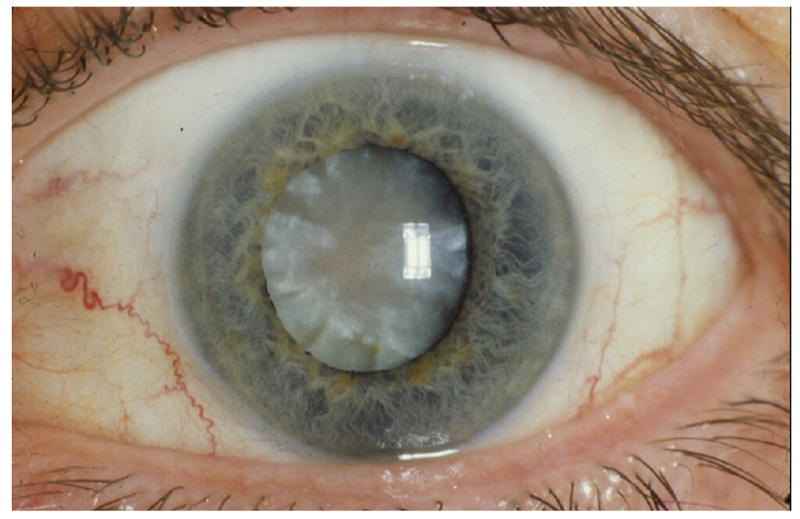
Opacification of the lens seen in cataracts.
Diagnosis
Cataracts is usually diagnosed clinically with a direct ophthalmoscope or slit-lamp.
Cataracts is a clinical diagnosis, which is made through the identification of opacification on simple direct ophthalmoscopy.
Findings that support the diagnosis of cataracts include:
- Loss, or darkening, of the red reflex
- Opacification seen within the red reflex
- Obscuration of ocular detail (due to opacification and crystallisation)
Patients with suspected cataracts should be referred non-urgently for further assessment by an ophthalmologist/optometrist with slit-lamp examination. This is important to confirm cataracts, the type, and exclude other causes of visual loss (e.g. glaucoma).
Differential diagnosis
Cataracts is one of several causes of progressive, painless loss of vision.
In ophthalmology it is important to have differentials for major presentations such as painful red eye, sudden loss of vision or chronic painless loss of vision.
Differential chronic visual loss
- Refractive error
- Corneal disease
- Presbyopia: longsightedness caused by loss of elasticity of the lines
- Age-related macular degeneration (ARMD)
- Open angle glaucoma
- Retinopathy (e.g. diabetes, drugs)
- Uveitis (chronic)
- Inherited eye disorders (e.g. retinitis pigmentosa)
Management
The definitive treatment of cataracts is surgical replacement of the diseased lens.
Cataracts surgery is indicated when vision is impaired to the point it is having a significant effect on activities of daily living (ADL). It is important to assess for co-existing disease and how much this is contributing to visual loss. This helps the ophthalmologist determine how much improvement the patient will get from surgical intervention.
Surgical intervention
Surgery involves surgical removal of the diseased lens and replacement with an artificial lens. It is usually completed on an outpatient basis under local anaesthetic. It is estimated that >95% of patients without pre-existing ophthalmic conditions will achieve 6/12 vision with surgery. There is also improvement to clarity and colour of vision.
There are two main techniques:
- Phacoemulsification
- Standard extracapsular cataract extraction
Phacoemulsification involves making a small incision, breaking up the diseased lens and aspirating the left over content. In this procedure the lens capsule remains in situ. A new lens is then placed into the capsule through the small incision.
Extracapsular cataract extraction involves whole removal of the diseased nucleus and aspiration of the lens cortex. The capsule is left in situ and a new rigid lens is inserted. In this procedure the incision is bigger than phaecomulsification.
Surgical complications
Overall, cataracts is considered a low-risk procedure, but complications do occur (~2%). They can broadly be divided into immediate and delayed.
Immediate:
- Endophthalmitis: bacterial or fungal infection of the intra-ocular fluid (vitreous/aqueous)
- Corneal oedema
- Cystoid macular oedema: inflammatory fluid in the retina.
- Malposition of the lens
- Posterior capsule rupture
- Toxic anterior segment syndrome: inflammatory response to non-infectious contaminants of equipment or solutions
- Hemorrhagic occlusive retinal vasculitis (HORV): associated with use of intra-ocular vancomycin (Antibiotic)
Delayed:
- Retinal detachment
- Macular degeneration
- Posterior capsule opacification: common problem. Due to proliferation of remnants of lens epithelial cells. Gradually improves after surgery. Can be treated with laser surgery.
Last updated: May 2021
Have comments about these notes? Leave us feedback
