Measles
Notes
Overview
Measles is a highly contagious viral infection caused by the measles morbillivirus.
Measles is a viral infection that was very common in childhood before the introduction of an effective immunisation programme. In countries where the measles vaccine is not part of a national immunisation programme it is still very prevalent.
Measles causes a classic presentation of fever, coryzal symptoms, and conjunctivitis followed by an exanthem. An exanthem is a widespread rash that usually occurs with systemic symptoms (e.g. fever). When it occurs in association with a virus it is known as a ‘viral exanthem’ and other common causes include rubella, roseola, and chickenpox.
Measles is a notifiable disease. It is usually a self-limiting illness and is treated with conservative management. However, certain groups are at increased risk (e.g. children < 1-year-old, pregnant, and immunocompromised).
Epidemiology
In the UK, measles is now a rare disease due to an effective vaccination programme.
Worldwide, measles is still a very prevalent childhood illness in areas with low vaccination rates. An overall population immunity > 95% is needed to stop ongoing measles transmission.
In the UK, measles is a rare condition due to the childhood vaccination programme. The UK health security agency releases the number of measles, mumps, and rubella cases each year.
Aetiology & pathophysiology
Measles is caused by a morbillivirus of the paramyxovirus family.
Measles is a viral infection caused by the measles morbillivirus. Humans are the only known reservoir of the virus. It is spread by person-to-person contact or airborne droplets through respiratory secretions. Viral particles enter the respiratory mucosa or through the conjunctiva of the eye.
The virus replicates locally before spreading to regional lymph nodes and then disseminating to other reticuloendothelial sites in the body. The virus then disseminates around the body again causing a viraemia, which is associated with the onset of symptoms.
The incubation period (time from acquisition of the pathogen to development of symptoms) is estimated between 6-21 days. People are considered infective around 5 days before and 4 days after the appearance of the rash. The period before the onset of rash is usually associated with a prodromal phase consisting of fever, fatigue, and cough.
Both natural infection and vaccination are thought to confer lifelong immunity to the virus.
Clinical features
Measles is characterised by several stages of infection.
Measles is characterised by the development of fever, coryzal symptoms, and conjunctivitis followed by an exanthem (widespread rash). This constellation of symptoms are divided into several stages of infection:
- Incubation period
- Prodromal period
- Period of exanthem
- Period of recovery
Incubation period
This is the period between the acquisition of the virus and the development of symptoms. Usually 6-21 days.
Prodromal period
This usually lasts for 2-4 days. It is characterised by:
- Fever
- Malaise
- Anorexia
- Conjunctivitis
- Coryza: runny nose, sore throat, nasal stuffiness
- Cough
Approximately 48 hours before the onset of rash (i.e. exanthem) characteristic spots known as ‘Koplik spots’ develop. These are white/greyish lesions approximately 1-3 mm in size that have an erythematous base. They are typically located on the buccal mucosa and can spread to involve the hard and soft palate.
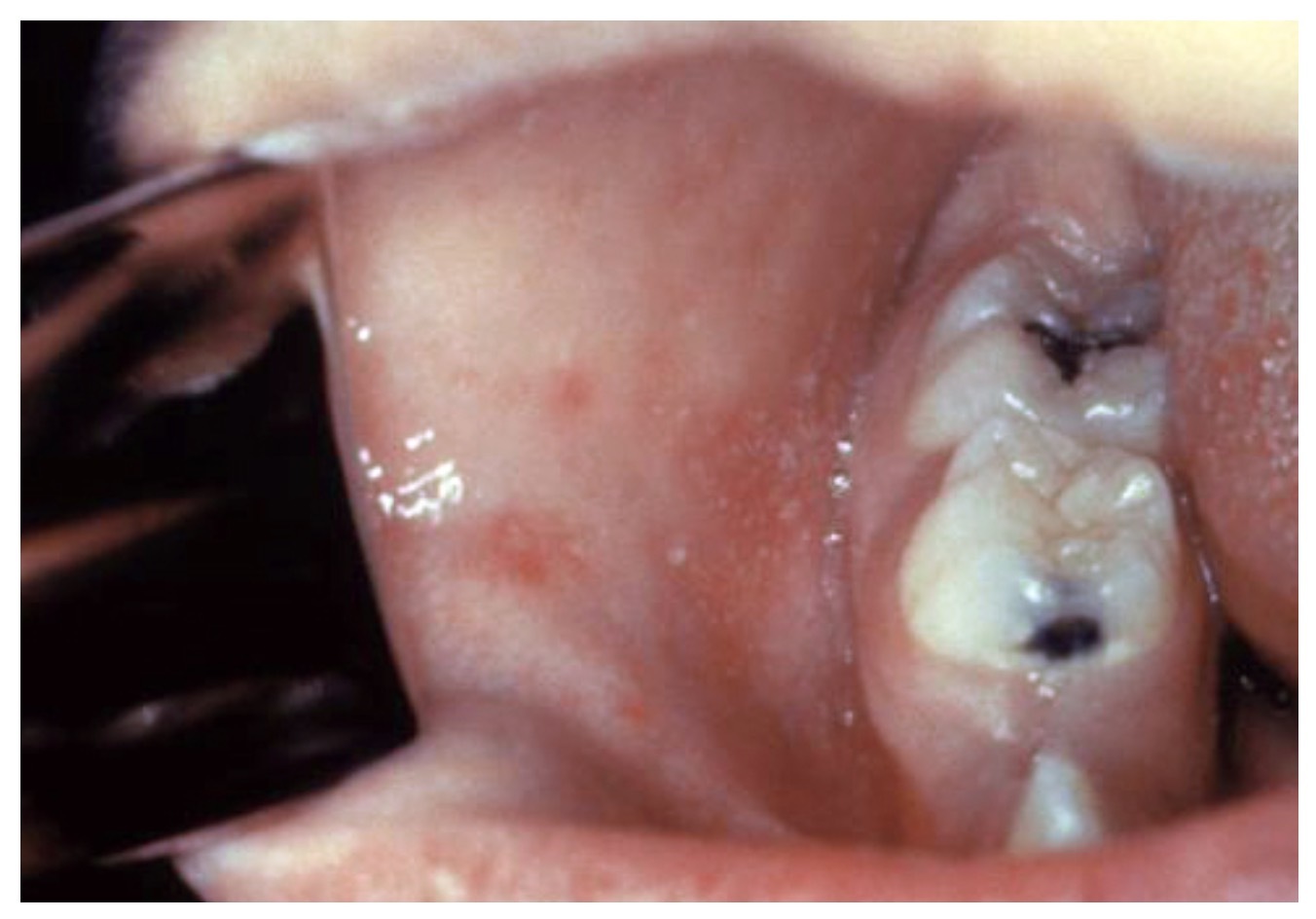
Koplilk spots located on the buccal mucosa
Period of exanthem
This refers to the development of a widespread erythematous rash. It typically starts on the face and then spreads to involve the neck, trunk, and extremities. It is usually a maculopapular, blanching rash that may become non-blanching in the later stages.

Classic appearance of exanthem from measles on dark and light skin tone
Period of recovery
Symptoms usually improve within 48 hours of rash onset. The rash usually starts to fade after 3-4 days and lasts 6-7 days in total. If the rash does not begin to fade after 4 days it may be a sign of complications. The cough may persist for weeks.
Diagnosis & investigations
The diagnosis of measles is based on antibody testing and viral PCR.
Measles is a rare condition in the UK but should be suspected when there is a characteristic history, known exposure to measles, and commonly no previous immunisation or an immunocompromised state.
A formal diagnosis can be made based on checking antibodies directed against the virus in blood or oral secretions. This is usually combined with viral polymerase chain reaction (PCR) testing.
- Serology: IgM and IgG antibodies directed against the measles virus can be detected in blood or oral secretions following the onset of illness. IgM is the initial antibody response, whereas IgG is a long-lasting response that appears second. Measles IgM antibodies are the main diagnostic method and usually appear around 3 days after the start of the rash.
- Viral PCR: this involves taking a sample (e.g. blood, nasopharyngeal, throat) and then amplifying any viral RNA that may be present specific to measles. Viral RNA is usually present 3 days after the rash onset.
Advice on the diagnosis of measles is usually guided by the health protection team (HPT).
Management
The management of measles is largely conservative with analgesia, antipyretics, and infective control measures.
Measles is largely a self-limiting condition that improves over a week. Adults and children should be advised to rest, drink plenty of fluid, use analgesia and antipyretics as needed, and avoid school or work for at least 4 days after the development of the initial rash.
All cases, confirmed or suspected, should be referred to the health protection team (HPT) as measles is a notifiable disease and they will help with diagnosis, case-control, contact tracing, and advice for at-risk groups.
Some patient groups are at increased risk and may require planned admission including:
- Patients who are immunosuppressed
- Patients who are pregnant
- Children < 1-year-old
- Patients with measles-associated complications (e.g. pneumonia, encephalitis)
Vaccination
Children in the UK are offered the measles vaccination as part of the national vaccination programme. This is a combined vaccine alongside mumps and rubella known as the ‘MMR’ vaccine (measles, mumps, and rubella). This should be given at 1 and 3 years. It is a live attenuated vaccine and may contain egg protein as it is grown in chick embryo fibroblast cell cultures. Patients with anaphylaxis to eggs should be referred to an immunologist before administration.
As MMR is a live attenuated vaccine it cannot be given to certain groups (e.g. pregnant people, those severely immunosuppressed).
Contact tracing
Patients with significant contact (same room for > 15 minutes) and no previous measles vaccination or confirmed laboratory status should be considered for immediate MMR vaccination unless contraindicated.
Complications
Measles is associated with a number of widespread complications due to the dissemination of the virus.
Measles is associated with complications in almost one-third of cases. Patients who are pregnant or those who are immunosuppressed are at increased risk of complications.
Complications include:
- Diarrhoea
- Mesenteric lymphadenitis
- Secondary infections (e.g. otitis media, gastroenteritis, pneumonia)
- Keratitis
- Myocarditis
- Neurological (e.g. encephalitis, acute disseminated encephalomyelitis, subacute sclerosis panencephalitis)
NOTE: Acute disseminated encephalomyelitis is a demyelinating condition due to a post-infectious autoimmune response. Usually occurs within two weeks of the rash and causes a whole variety of neurological features. Subacute sclerosing panencephalitis is a fatal, progressive disease that develops many years after a measles infection. Characterised by marked neurological deterioration but the pathophysiology is unknown.
Last updated: July 2022
Have comments about these notes? Leave us feedback
