Fibroadenoma
Notes
Introduction
Fibroadenomas are the most common benign tumour of the breast.
Traditionally referred to as ‘breast mice’, these discrete, mobile lumps often occur in younger women. It is important to distinguish and exclude breast cancer, as such patients should be referred for a triple assessment in line with NICE guidance.
As a general rule, 50% regress spontaneously, 25% will remain unchanged and 25% will get bigger.
Epidemiology
Fibroadenomas most commonly occur in women aged 14 to 35.
These benign tumours are typically seen in younger patients and often regress after menopause. There is up to a 10% lifetime incidence of fibroadenomas in women.
Types
Fibroadenoma may be split into a number of sub-types.
These include:
- Simple fibroadenomas: These are small (1-3cm) lumps with classical features of a firm, mobile and painless lump.
- Complex fibroadenomas: Complex appearance on histopathology. These have been associated with a slight increase in the risk of breast cancer.
- Giant fibroadenomas: Large fibroadenomas growing to a size of greater than 5cm. Difficult to distinguish from a phyllodes tumour.
Pathophysiology
Fibroadenomas are fibroepithelial tumours arising from stromal and epithelial tissue.
There is clear evidence of a hormonal link. They tend to develop after menarche and regress after menopause. They may be triggered or increase in size during pregnancy or when taking hormone replacement therapy (HRT).
A genetic basis has also been identified with a mutation to MED12 found in around 60% of tumours. MED12 has been implicated in many other conditions including uterine fibroids.
Clinical features
Fibroadenomas present with a breast lump which is typically painless.
They classically occur on the outer, upper quadrant of the breast. In general, the breast lump can be described as:
- Painless
- Firm
- Mobile
In up to 20% of cases, there are multiple fibroadenomas affecting one or both breasts.
Referral
NICE have set out criteria to guide referral for patients with symptoms suggestive of breast cancer.
Patients should be referred on a two-week wait suspected cancer pathway if:
- 30 and over and have an unexplained breast lump with or without pain or
- 50 and over with any of the following symptoms in one nipple only:
- Discharge
- Retraction
- Other changes of concern
NICE also recommend clinicians consider a two-week wait suspected cancer pathway for people:
- With skin changes that suggest breast cancer or
- Aged 30 and over with an unexplained lump in the axilla
Consider non-urgent referral in people aged under 30 with an unexplained breast lump with or without pain.
Local services may have their own urgent referral guidelines, additional reasons for which a clinician may urgently refer include 'women with unilateral non-cyclical breast pain persisting beyond one menstrual cycle'. Clinicians judgement should be used - if concerns exist they should discuss with the local specialist service.
Triple assessment
Unexplained breast lumps should undergo specialist assessment.
The one-stop breast clinic incorporates a triple assessment in one appointment. It requires localities to have access to appropriate specialists and diagnostic equipment but offers patients a convenient and efficient service.
The majority of patients can be reassured that they do not have evidence of breast cancer following a single visit. Some may need to await further tests (e.g. core biopsy results) whilst others may be given a likely diagnosis.
In young patients (< 25 years) with a low-risk history; examination and imaging findings - these alone may be sufficient to make a diagnosis of fibroadenoma. In older patients or those with indeterminate (or concerning) examination or imaging, a biopsy must be considered.
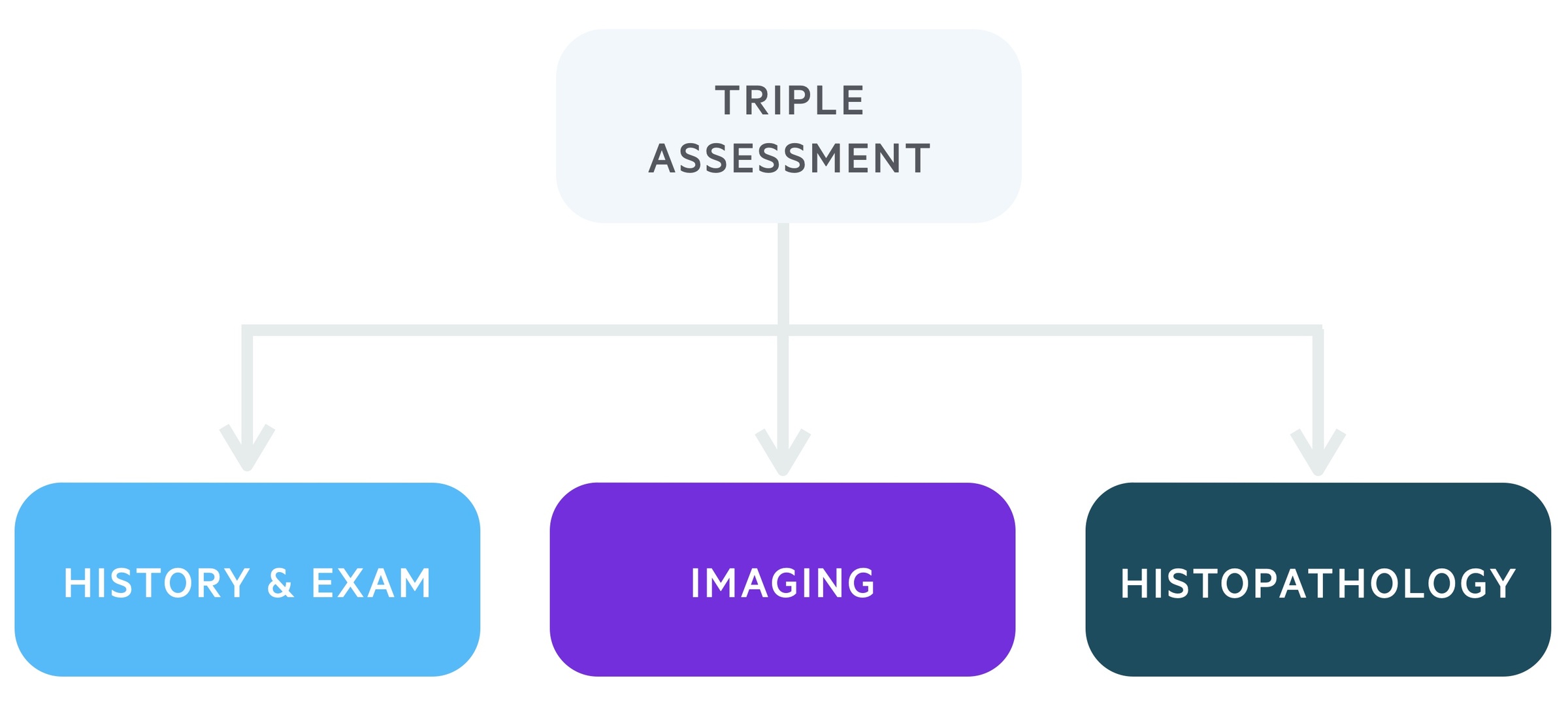
1. Clinical history and examination
Each patient referred to the two-week wait one-stop clinic will be reviewed by a specialist. This will involve a detailed history including family history. Following this, the patient will be carefully examined.
2. Imaging
This will depend in part on the history and examination and the patient's age. Clinics are set up to conduct both breast ultrasound scans (USS) and mammograms.
- Mammogram: A mammogram utilises x-rays to image breast tissue. Finding suggestive of cancer include soft tissue masses and microcalcifications.
- USS: Breast USS is the modality of choice in women under the age of 40. It is also used in older women, particularly when mammogram and clinical findings do not align. High-resolution scanners meeting NHSBSP standards are used.
3. Histopathology
Depending on what is found in the first two steps a tissue/cellular sample may be taken. This may be in the form of fine-needle aspiration (provisional same-day results) or core biopsy (often provisional same-day results, sometimes may have to wait a few days).
Management
The majority of fibroadenomas can be managed conservatively.
Conservative
Simple, small and asymptomatic, biopsy-proven fibroadenomas do not need further treatment. If appearances are classical in young patients (e.g. under 25 years) biopsy may be avoided and interval imaging considered.
Patients should be advised to re-present if the mass changes in size, if they develop pain or any other features that may indicate breast cancer (e.g. skin and nipple changes).
Intervention
In certain circumstances excision may be discussed, this includes:
- Cellular fibroepithelial lesion (difficult to differentiate from phyllodes tumour)
- Rapidly growing fibroadenoma
- Persistent pain or discomfort (NB - no guarantee surgical excision will improve symptoms)
The main options are surgical excision and ultrasound-guided vacuum-assisted mammotome. Open surgical excision is recommended for cellular fibroepithelial lesions.
Other treatment options include High-Intensity Focused Ultrasound (HIFU) and cryoablation.
Further reading
- Association of Breast surgery summary statement: Management of fibroadenomas
Last updated: March 2021
Have comments about these notes? Leave us feedback
