Acute otitis externa
Notes
Overview
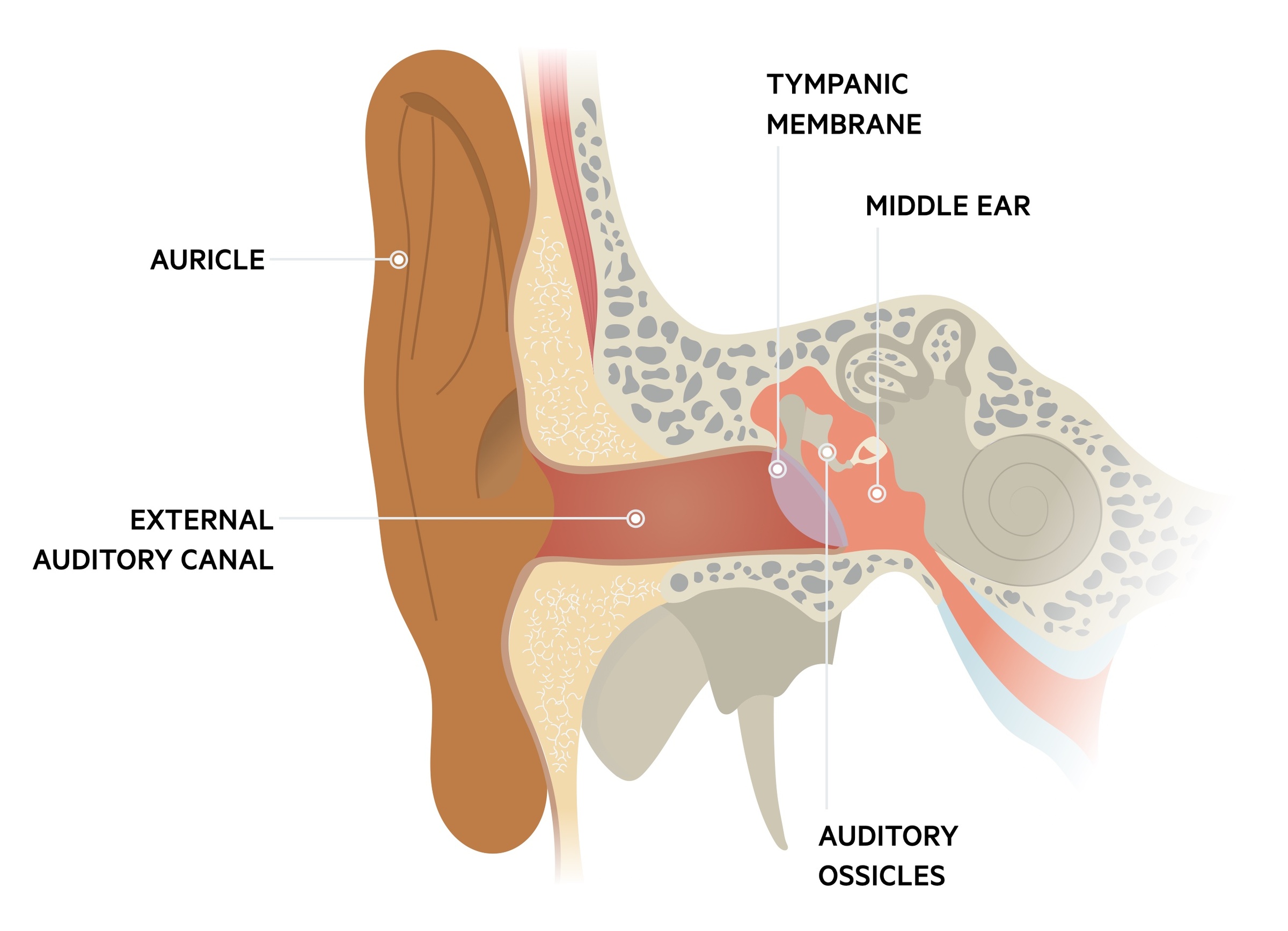
Otitis externa refers to inflammation of the external auditory canal.
Though the inflammation can have many causes (e.g. allergic, dermatologic), infection, in particular by bacteria, is the most common cause.
Broadly, otitis externa may be defined as:
- Acute: ≤ 3 weeks of symptoms and signs of ear canal inflammation, usually with rapid onset (generally within 48 hours)
- Chronic: ≥3 months of symptoms and signs of chronic inflammation of the middle ear and mastoid cavity (e.g. persistent on recurrent ear discharge).
Malignant otitis externa (MOE) is a rare life-threatening condition where the infection spreads to the surrounding bone, it is covered here.
Epidemiology
It is estimated that up to 10% of people will experience acute otitis externa in their lifetime.
Though otitis externa (both acute and chronic) can occur at any age, it is more common in children and adolescents, with incidence peaking between the ages of 5-14.
Risk factors
Acute otitis externa is sometimes called swimmers ear because of its increased incidence in swimmers.
- Swimming
- Humid air
- Young age
- Diabetes
- Trauma
- Narrow external auditory meatus
- Obstructed external auditory meatus
- Eczema, psoriasis
- Radiotherapy
Aetiology
Bacterial infection accounts for up to 98% of cases of acute otitis externa.
Infection
Bacterial infection is the most common cause of acute otitis externa. Pseudomonas aeruginosa or Staphylococcus aureus is most frequently implicated.
Fungal pathogens may also result in otitis externa, commonly Candida albicans or Aspergillus species.
Dermatitis
Dermatological conditions can also cause otitis externa, these include:
- Seborrhoeic dermatitis
- Contact dermatitis
Clinical features
Acute otitis externa often presents with ear pain and itchiness.
Patients tend to present with a short history of otalgia (ear pain), frequently associated with discharge. In more severe cases swelling of the external auditory canal and debris may result in hearing loss.
Symptoms
- Itch
- Tenderness
- Hearing loss
- Discharge
Signs
- Inflamed external auditory canal
- Erythema
- Scaly skin
- Pre-auricular lymphadenopathy
Management
Treatment normally takes the form of analgesia and topical therapies.
Investigations
In many cases, no investigations beyond a thorough history and examination are needed. If the presentation is atypical, recurrent or treatment-resistant, an ear swab, sent for MC&S may be of use.
Treatment
Consideration should be given to any underlying cause and how that may be treated. Cleaning of the external canal can be needed. Patients should avoid swimming for a minimum of 7-10 days.
- Analgesia: paracetamol and ibuprofen (if no contraindications).
- Topical therapy: topical antibiotics +/- a topical steroid may be given.
Oral antibiotics are rarely indicated and should prompt discussion with ENT. Any patient who is systemically unwell should be urgently reviewed by ENT.
NOTE: Clinicians should be alert to severe infection and malignant otitis externa. This is seen in particular in the elderly and patients with diabetes or a compromised immune system.
Prevention
The ears should be kept clean and dry whilst trauma must be avoided. Earplugs or a swimming cap can help reduce the incidence.
If a precipitating factor, allergies should be identified and avoided whilst dermatological conditions should be optimally treated.
There are acidifying ear drops that can be used prior to sleeping or before and after swimming that may reduce the incidence of otitis externa.
Last updated: October 2024
Have comments about these notes? Leave us feedback