Pharyngeal pouch
Notes
Overview
A pharyngeal pouch, also known as Zenker’s diverticulum, is a sac-like out-pouching that occurs within the hypopharynx.
A Zenker diverticulum (ZD), more commonly known as a pharyngeal pouch, is a herniation of the posterior pharyngeal wall that occurs at an area of weakness within the inferior pharyngeal constrictor. It typically occurs in older adults and can lead to symptoms of dysphagia, regurgitation, and more seriously, aspiration pneumonia.
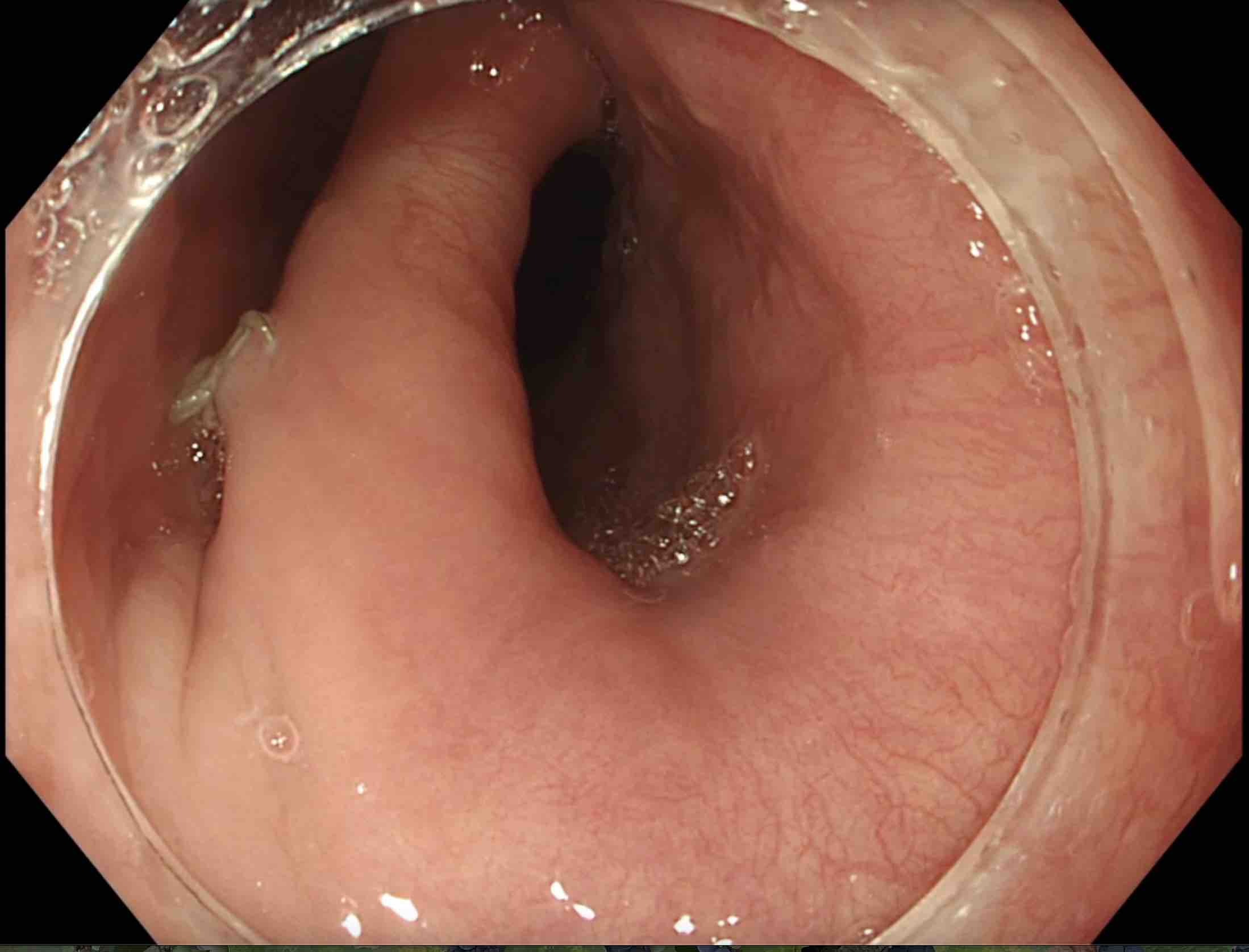
Pharyngeal pouch seen at endoscopy with a transparent distal attachment.
Evidence of previous endoscopic stapling
Epidemiology
A pharyngeal pouch is rare before the age of 40.
A pharyngeal pouch is a relatively rare condition that predominantly occurs in older adults. However, the actual prevalence is thought to be underestimated because many patients may be asymptomatic. There is a reported slight male predominance.
Aetiology & pathophysiology
A pharyngeal pouch is a ‘false’ diverticulum because it only contains mucosal and submucosal layers.
The pharynx is a cone-shaped passageway that runs between the mouth and nasal cavity to the top of the oesophagus and trachea. It forms part of the aerodigestive tract and is divided into three sections:
- Nasopharynx
- Oropharynx
- Hypopharynx (also known as the laryngopharynx)
The pharynx is involved in the movement of air from the nasal and oral cavities to the larynx, as well as the movement of food to the oesophagus. The pharynx contains three major constrictor muscles (superior, middle, inferior) that are involved in swallowing and speaking.
The inferior pharyngeal constrictor is composed of the thyropharyngeus muscle superiorly and the cricopharyngeal muscle inferiorly. The orientation of these muscle fibres creates a triangular gap (or weakness), known as Killian’s triangle, that is prone to the formation of a diverticulum (i.e. herniation of the pharyngeal mucosa and submucosa through this gap in the muscular arrangement). The actual cause of the diverticulum is unclear, although several factors have been proposed such as abnormal motility and increased pressure during bolus transfer of food to the oesophagus.
Clinical features
The principal symptom of a pharyngeal pouch is dysphagia (i.e. difficulty swallowing).
The cardinal features of a pharyngeal pouch are dysphagia and regurgitation of food, often hours after ingestion. This is because food and liquid can become trapped within the pouch including medications if the pouch becomes large. Other patients may be asymptomatic and the pouch identified when performing investigations for other reasons.
Symptoms
- Dysphagia (solids and liquids): usually described as oropharyngeal because there is difficulty with the initial aspects of swallowing in the mouth
- Regurgitation
- Halitosis (bad breath)
- Weight loss
- Globus (sensation of having a lump in the throat)
- Hoarseness
- Chronic cough
Signs
- Gurgling in the throat
- Mass in the neck (if the pouch is very large)
- Malnourishment (e.g. sarcopenia, low BMI)
Diagnosis & investigations
The gold-standard diagnosis for a pharyngeal pouch is a barium swallow.
A pharyngeal pouch is best diagnosed on a barium swallow that involves continuous fluoroscopic assessment of swallowing after drinking barium contrast solution. This enables assessment of the swallowing mechanism and any passage of contrast into a pouch.

Contrast is seen to pool in a pharyngeal pouch on barium swallow.
Image courtesy of Bernd Brägelmann, Wikimedia commons.
Many patients will undergo an upper gastrointestinal (GI) endoscopy, but this is not required for the diagnosis. This is because the cardinal feature is dysphagia, which is a red flag feature for malignancy in the upper GI tract, so many patients will be referred for this investigation. A small pharyngeal pouch may be missed at endoscopy, but a large pouch is usually seen as a ‘second lumen’ when trying to pass the endoscope into the oesophagus.
Management
Patients with small, asymptomatic pouches do not require any treatment.
Patients who are asymptomatic or have small pouches (i.e. < 1cm) do not require any specific treatment. For patients with symptomatic or larger pharyngeal pouches, there are a variety of treatment options that can include surgery or endoscopy.
The aim of treatment for a pharyngeal pouch is to dissect the septum of the cricopharyngeal muscle that is maintaining the integrity of the pouch by performing a myotomy (i.e. cutting muscle). This creates a common cavity between the pouch and the oesophageal lumen that improves symptoms. There are currently three methods for performing myotomy with variable success:
- Open surgery (e.g. transcervical diverticulectomy)
- Rigid endoscopy (e.g. endoscopic stapling)
- Flexible endoscopy (e.g. flexible endoscopic septum division)
Each technique is associated with its own risks and benefits. In general, surgery has a high success rate (80-100%), but recurrence may be high (up to 19%) and it is associated with significant morbidity and mortality compared to endoscopic techniques. Flexible techniques have become routine, which are associated with a clinical success rate of 91%, adverse event rate of 11.3%, and recurrence of 10.3%. Newer techniques are now being used to treat pharyngeal pouches including Zenker-peroral endoscopic myotomy (Z-POEM) that involves third-space endoscopy.
Complications
Aspiration of partially digested food or liquid may occur from the pouch into the lungs.
A pharyngeal pouch may be associated with several complications, some of which can be life-threatening, especially in patients who are older and frailer. Complications can include:
- Aspiration pneumonia
- Malnutrition
- Medication ineffectiveness (tablets become trapped in the pouch and regurgitated)
- Fistula formation
- Ulceration
- Squamous cell carcinoma within the pouch (rare)
Last updated: February 2023
Have comments about these notes? Leave us feedback
