Quinsy
Notes
Overview
Quinsy, also termed peritonsillar abscess, is a collection of pus in the peritonsillar space.
There are two types of infection that affect the peritonsillar regions:
- Peritonsillar cellulitis: refers to infection of the peritonsillar tissue in the absence of a discrete collection of pus (abscess).
- Peritonsillar abscess (quinsy): refers to a discrete collection of pus in the peritonsillar region.
Quinsy occurs most commonly as a complication of bacterial tonsillitis. Unlike simple tonsillitis, it mandates surgical intervention to drain the collection. Group A beta-haemolytic streptococcus and haemophilus influenzae are commonly implicated.
Severe complications are rare but can include sepsis, the spread of the infection through the deep spaces of the neck and airway obstruction.
Note: In patients presenting with any of a severe sore throat, drooling, stridor or trismus – epiglottitis – a rare but potentially life-threatening condition should be considered.
Clinical features
Patients present with sore throat, fevers and may complain of trismus or altered voice.
The sore throat may be unilateral or affect one side more than the other. The voice can become altered, classically described as a 'hot potato' voice. Trismus refers to restriction in a person's ability to open their mouth. The diagnosis of quinsy can be made following a suggestive history and examination.
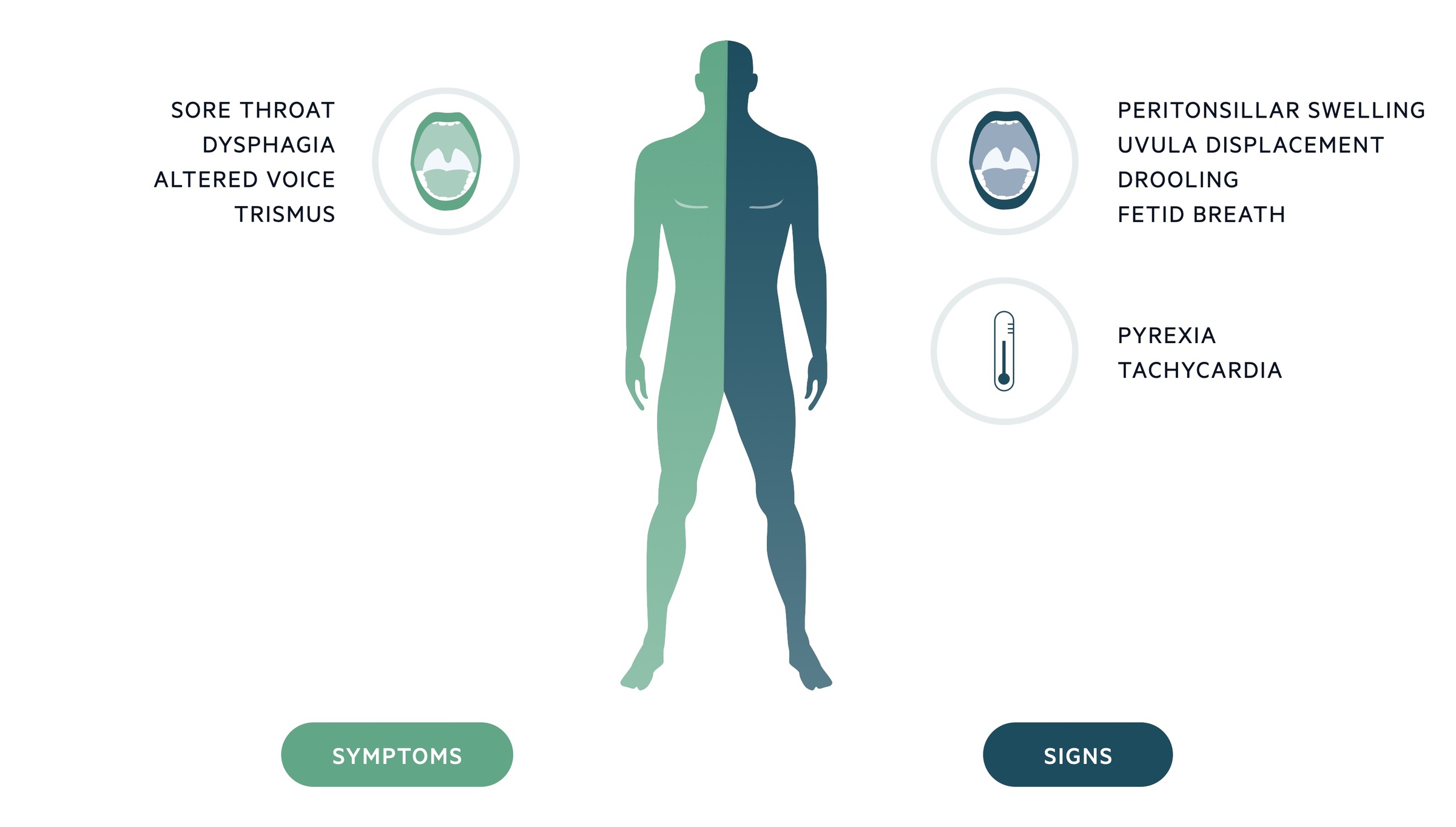
Symptoms
- Sore throat
- Fever
- Trismus
- Dysphagia
- Altered voice
Signs
- Peritonsillar swelling
- Exudate
- Drooling
- Stertor (sound caused by upper airway obstruction)
- Displacement of uvula (away from the side of abscess)
- Fetid breath
Note: If there is clinical evidence of spreading of infection through the deep spaces of the neck, a senior ENT and anaesthetic review should be arranged.
Investigations
Quinsy tends to be a clinical diagnosis, intraoral ultrasound may be used to confirm it.
Bedside
- Observations
Bloods
- FBC
- U&Es
- CRP
- LFTs
- EBV IgM antibody (if infectious mononucleosis is suspected)
Imaging
- Intraoral ultrasound: rarely used but offers reasonable sensitivity and specificity for peritonsillar abscess.
- CT/MRI: axial imaging is required if there is suspicion the infection has spread beyond the peritonsillar space.
Special tests
- Pus cultures: may be sent but rarely impact management
Management
Patients with quinsy should be referred for urgent ENT review.
1. Medical
IV access should be obtained and routine blood tests sent. Patients have frequently had reduced oral intake and benefit from IV fluids. Adequate analgesia, topical where possible, should be administered.
Most will commence IV antibiotics (e.g. penicillin and metronidazole) and some give a dose of IV steroids (6.6mg IV dexamethasone).
2. Surgical
Quinsy requires surgical intervention. An ENT surgeon will normally either aspirate the abscess or complete an incision and drainage.
Patients should complete a course of antibiotics (follow local guidelines) following their surgical intervention. In some centres an ENT surgeon will carry out a tonsillectomy acutely to treat quinsy (quinsy tonsillectomy).
Following initial management, patients should be observed for a period. In those who feel well, are able to maintain their oral hydration (swallow well) and are clinically stable, discharge can be considered. They should be given a course of antibiotics to complete and appropriate safety netting.
Note: Recurrent quinsy is an indication for elective tonsillectomy.
Last updated: March 2021
Have comments about these notes? Leave us feedback
