Thyroid anatomy
Notes
Overview
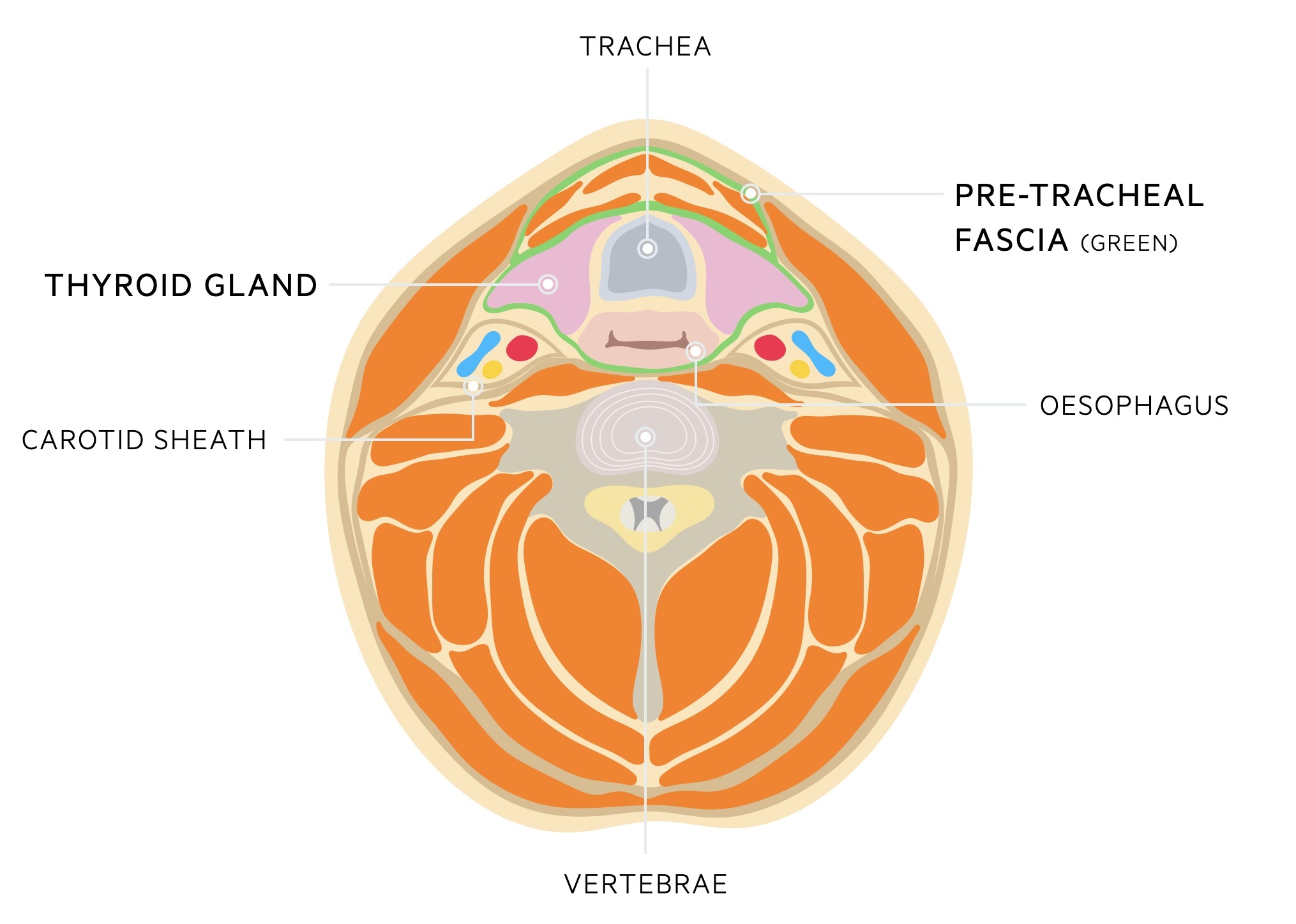
The thyroid is located in the mid-line of the neck, anterior to the trachea and inferior to the larynx.
It is found within the pre-tracheal fascia, one of the fascial compartments of the neck. It is a thin fascia in the anterior part of the neck and is composed of two parts:
- Muscular part: contains the infrahyoid muscles
- Visceral part: contains the thyroid, trachea and oesophagus
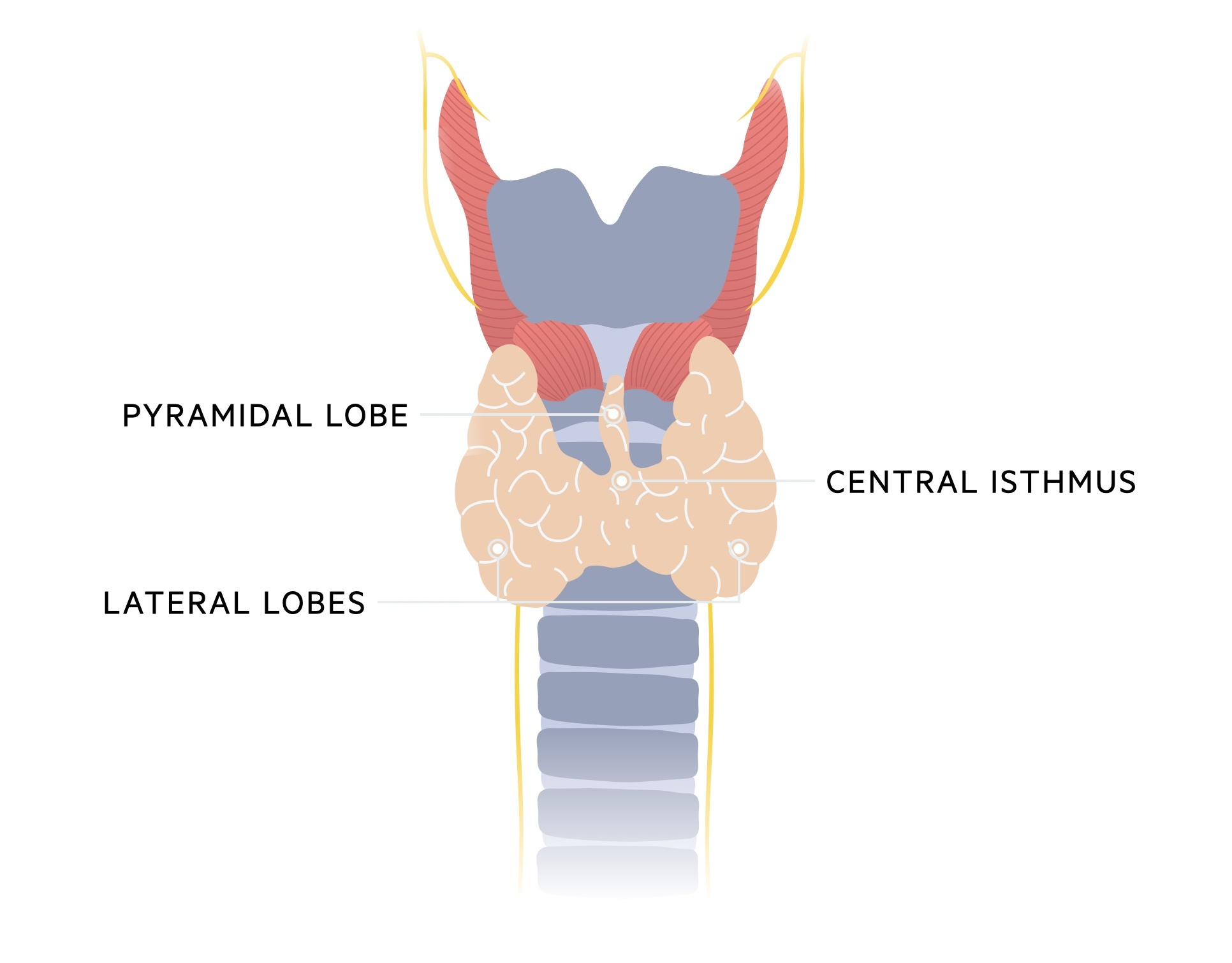
The thyroid gland is comprised of two lateral lobes connected by a central isthmus. It is surrounded by a fibrous capsule and located at the level of vertebrae C5-T1.
The pyramidal lobe, an embryological remnant from the descent of the thyroid, typically projects upwards from the isthmus, however, there is a wide degree of variation between individuals.
The primary function of the thyroid gland is to produce thyroid hormones (T3 and T4) following stimulation by thyroid-stimulating hormone (TSH).
Surrounding structures
The thyroid gland is surrounded by a number of important structures.
Thyroid cartilage
The thyroid cartilage is one of the three unpaired laryngeal cartilages (the others being the cricoid cartilage and epiglottis). It is formed by hyaline cartilage and is found above the thyroid gland, sitting at the level of vertebrae C4-5.
It forms a median projection, more prominent in males, termed the Adam's apple. Superior to this projection is the superior thyroid notch. The cartilage has both superior and inferior horns.
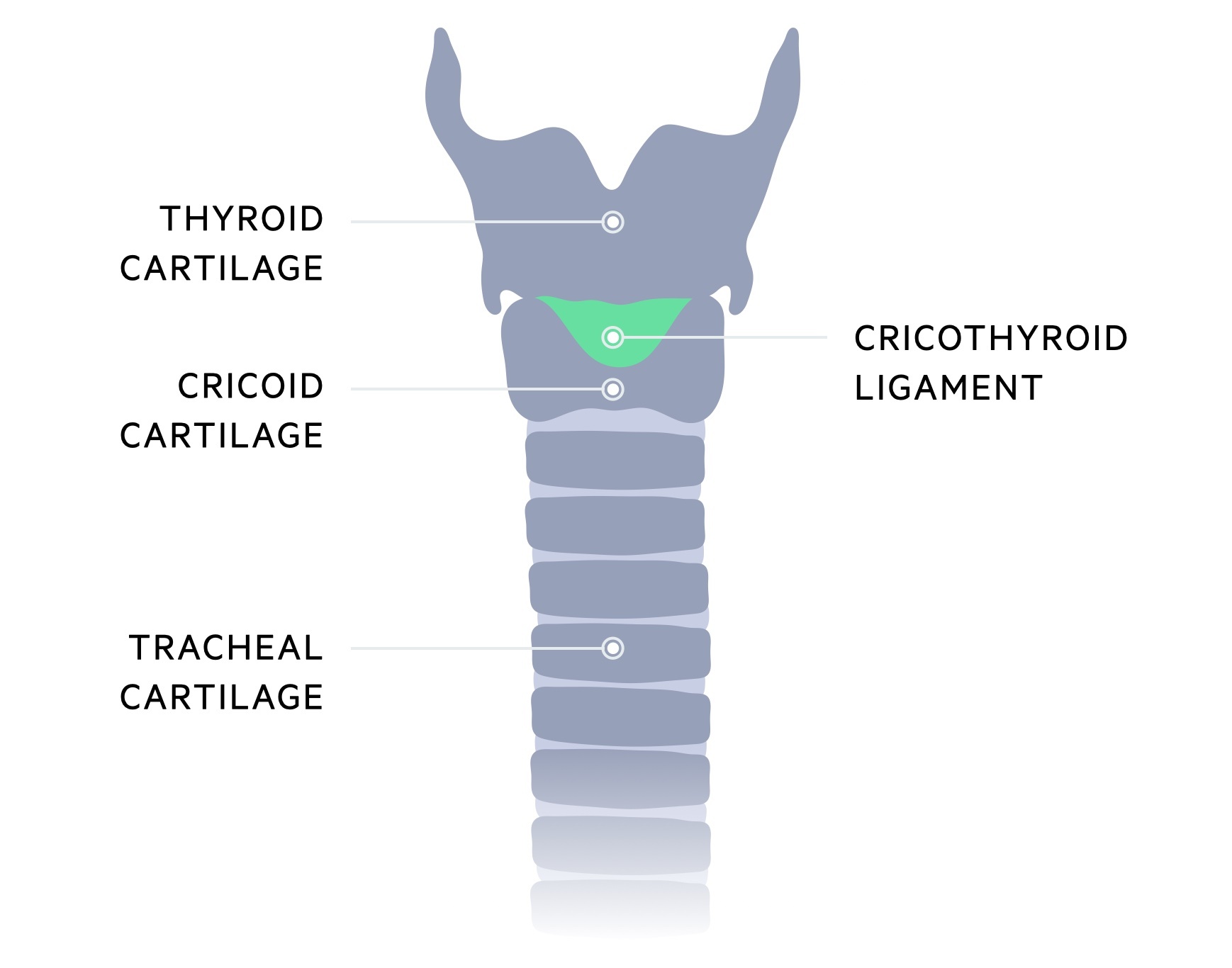
Cricoid cartilage
The cricoid cartilage sits at the level of vertebrae C6. It is the only complete ring of cartilage in the trachea. It is composed of a posterior component termed the lamina and an anterior component termed the arch. It is attached to the first tracheal ring by the cricotracheal ligament.
Medium cricothyroid ligament
This ligament connects the inferior border of the thyroid cartilage with the superior border of the cricoid cartilage. An incision is made through the medium cricothyroid ligament to establish an emergency airway - a cricothyroidotomy.
Parathyroid glands
The parathyroid glands (typically four) are located posterior to the thyroid gland. It is important to note there is a great deal of variety in both the location and number of glands.
They are responsible for the release of parathyroid hormone, a key part of the calcium homeostasis pathways. Due to their location, they are frequently removed, injured or devascularised during a total thyroidectomy, typically resulting in a transient hypocalcaemia.
Arterial supply
A rich blood supply is received from the external carotid artery and the thyrocervical trunk.
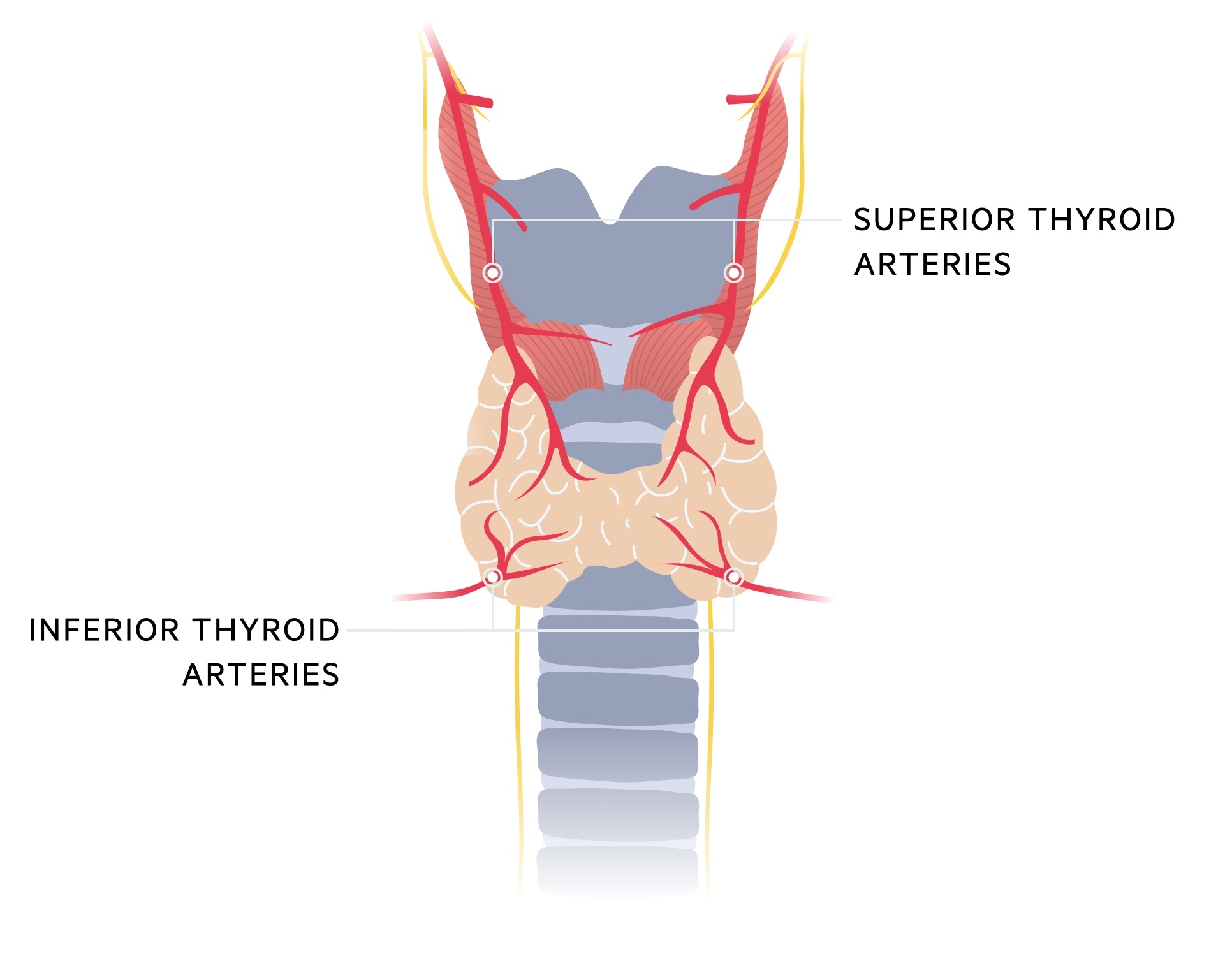
Superior thyroid arteries
- Supplies: anterosuperior aspect of the thyroid gland.
- Source: it is the first branch of the external carotid artery.
- Branches:
- Hyoid artery
- Sternocleidomastoid branches
- Superior laryngeal artery
- Cricothyroid branch
Inferior thyroid arteries
- Supplies: posteroinferior aspect of the thyroid gland.
- Source: thyrocervical trunk (third branch of the subclavian artery).
- Branches:
- Inferior laryngeal
- Oesophageal
- Tracheal
- Ascending cervical
- Pharyngeal
Venous drainage
The thyroid gland is drained by three pairs of veins.
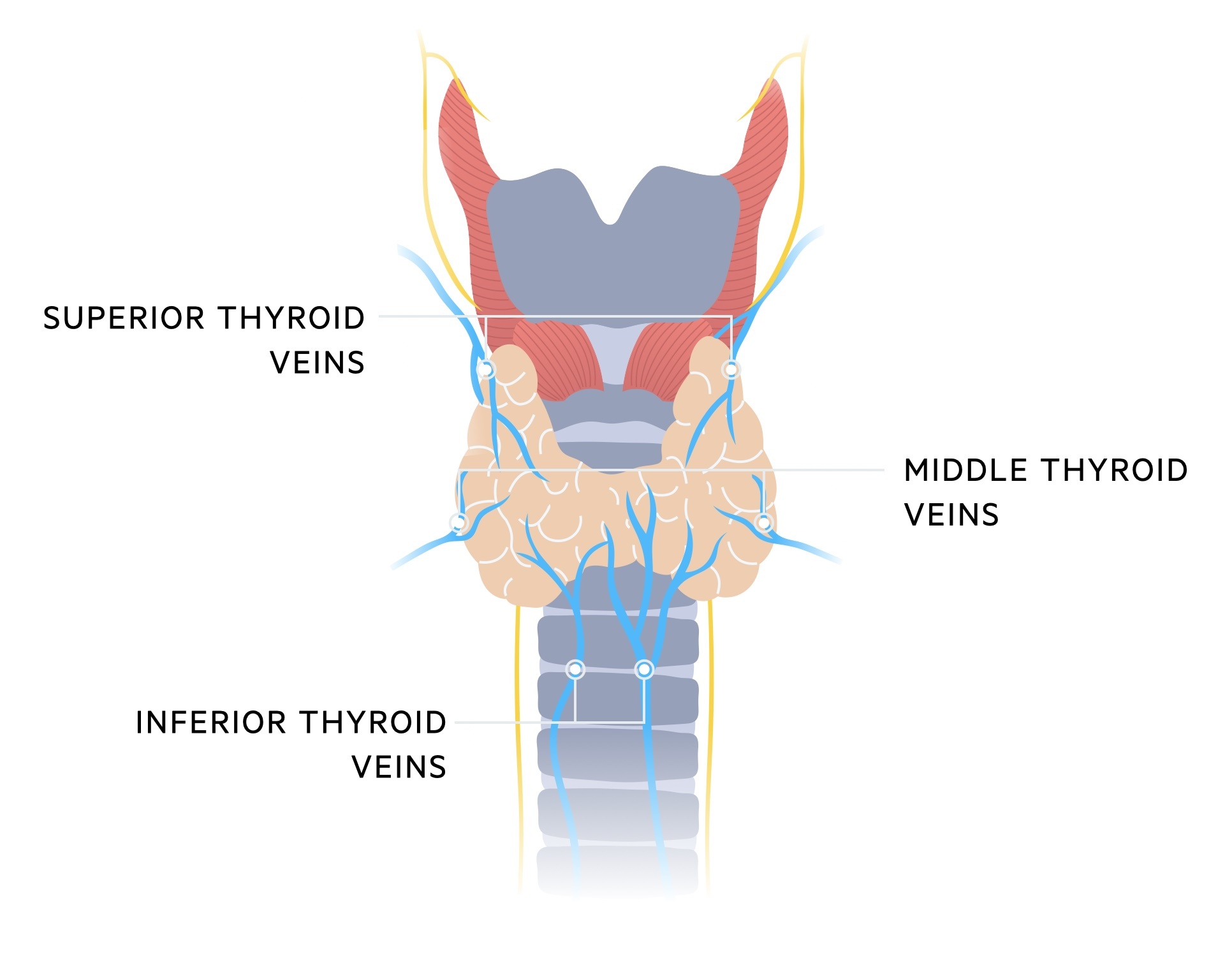
Superior thyroid veins
- Drains from: superior poles of the thyroid gland
- Drains to: internal jugular vein
Middle thyroid veins
- Drains from: middle poles of the thyroid gland
- Drains to: internal jugular vein
Inferior thyroid veins
- Drains from: lower poles of the thyroid gland
- Drains to: brachiocephalic vein
Recurrent laryngeal nerve
The recurrent laryngeal nerve is a branch of the vagus nerve (cranial nerve X).
The right and left recurrent laryngeal nerves branch off the left and right vagus nerves at different levels. The right side branches of at the level of the subclavian artery whilst the left side branches at the level of the arch of the aorta.
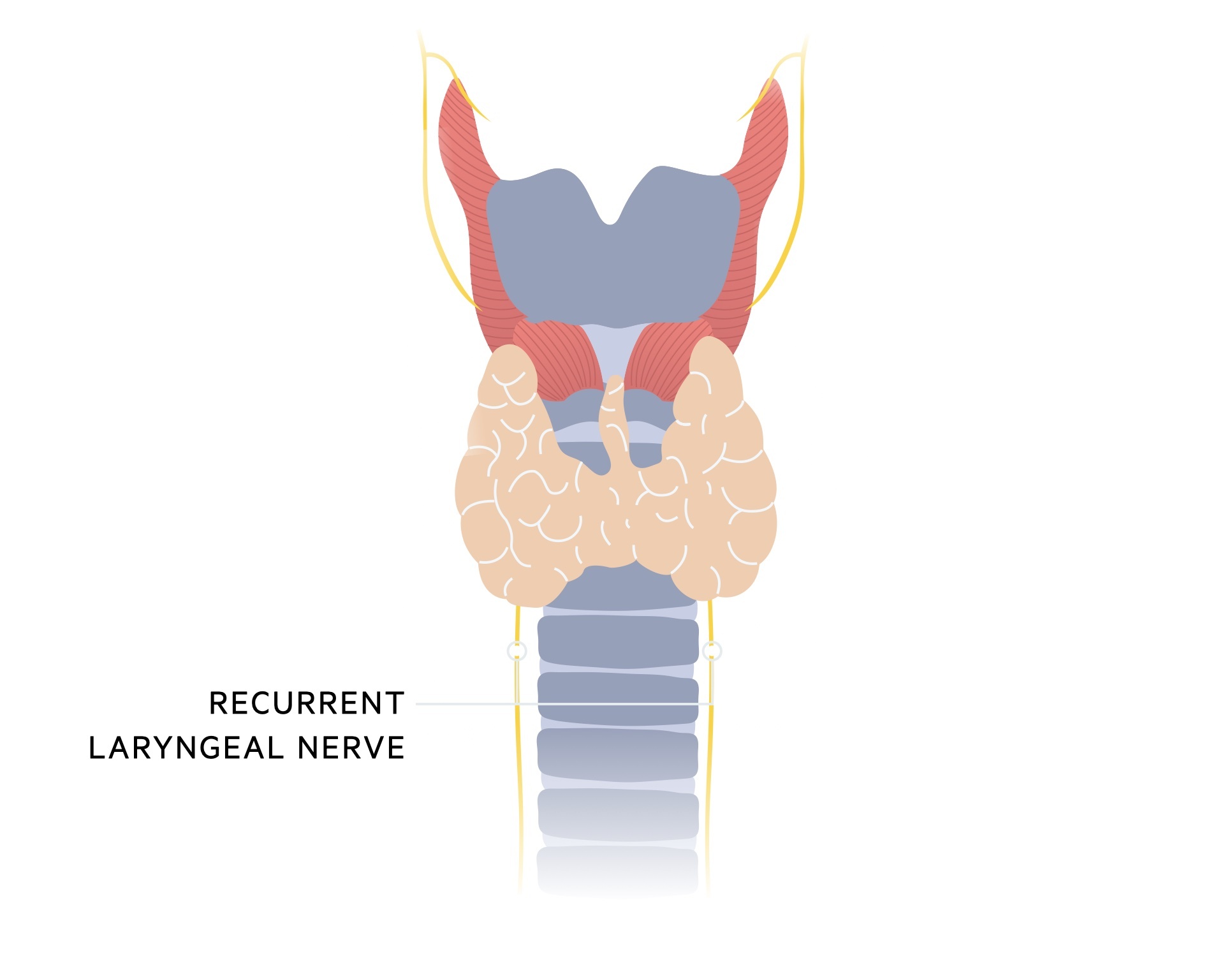
They follow a ‘recurrent’ path returning back upwards through a groove between the trachea and oesophagus. This brings them close to the thyroid gland. The nerve may be damaged during thyroid surgery, typically resulting in vocal cord paralysis on the affected side and a hoarse voice.
The recurrent laryngeal nerve has a number of functions:
- Motor:
- Intrinsic muscles of the larynx (except cricothyroid muscle).
- Sensory and secretomotor:
- Glottis
- Subglottis
- Trachea
Last updated: October 2022
Have comments about these notes? Leave us feedback
