Anterior abdominal wall
Notes
Introduction
The abdominal wall refers to the layers of anterolateral structures including skin, muscles, nerves, vessels and connective tissues between the thorax and pelvis.
The muscles of the abdominal wall have multiple functions. They act to protect and contain the abdominal viscera. They are able to contract, increasing intra-abdominal pressure, aiding expiration, coughing and vomiting. Together they help with truncal movements, particularly against resistance.
They are organised into layers with the rectus abdominis found centrally and the (from superficial to deep) external oblique, internal oblique and transversus abdominis found anterolaterally.
Surface anatomy
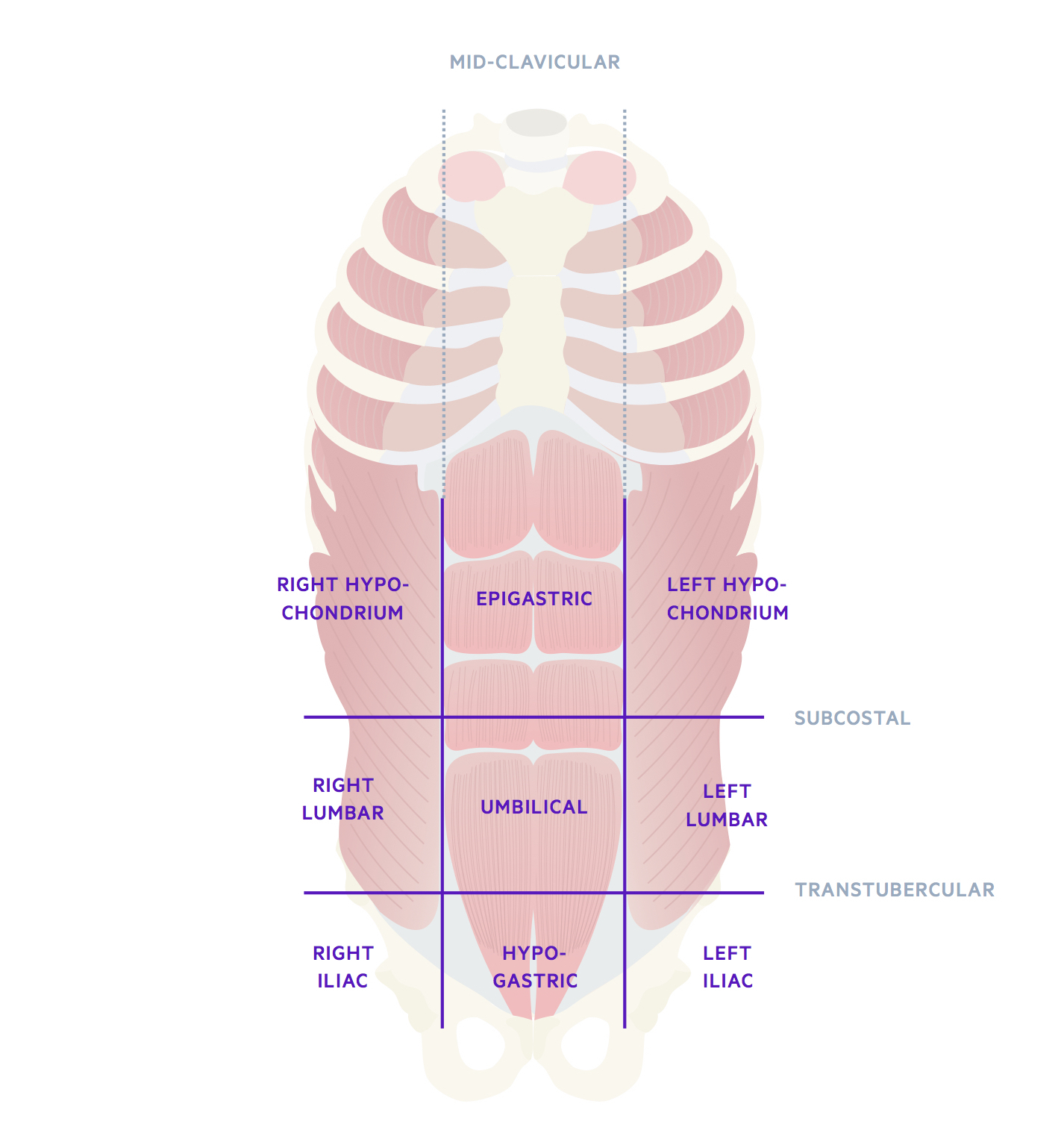
The anterior abdominal wall may be divided into nine regions.
The nine regions of the abdomen are created by four imaginary intersecting lines:
- 2 x mid-clavicular lines: vertical lines that pass down from the mid-point of the clavicle to the mid-inguinal point.
- The subcostal plane: a transverse line that passes across the abdomen at the level of the inferior aspect of the 10th costal cartilage. This line bisects the 3rd lumbar vertebrae.
- The transtubercular plane: a transverse line that passes across the iliac tubercles. These are located approximately 5 cm posterior to the anterior superior iliac spine (ASIS). The line bisects the 5th lumbar vertebrae.
Another commonly discussed plane is the ‘Transpyloric plane of Addison' or more simply the transpyloric plane. It is located halfway between the suprasternal notch and the top of the pubic symphysis. It is approximately a hands breath below the xiphoid process.
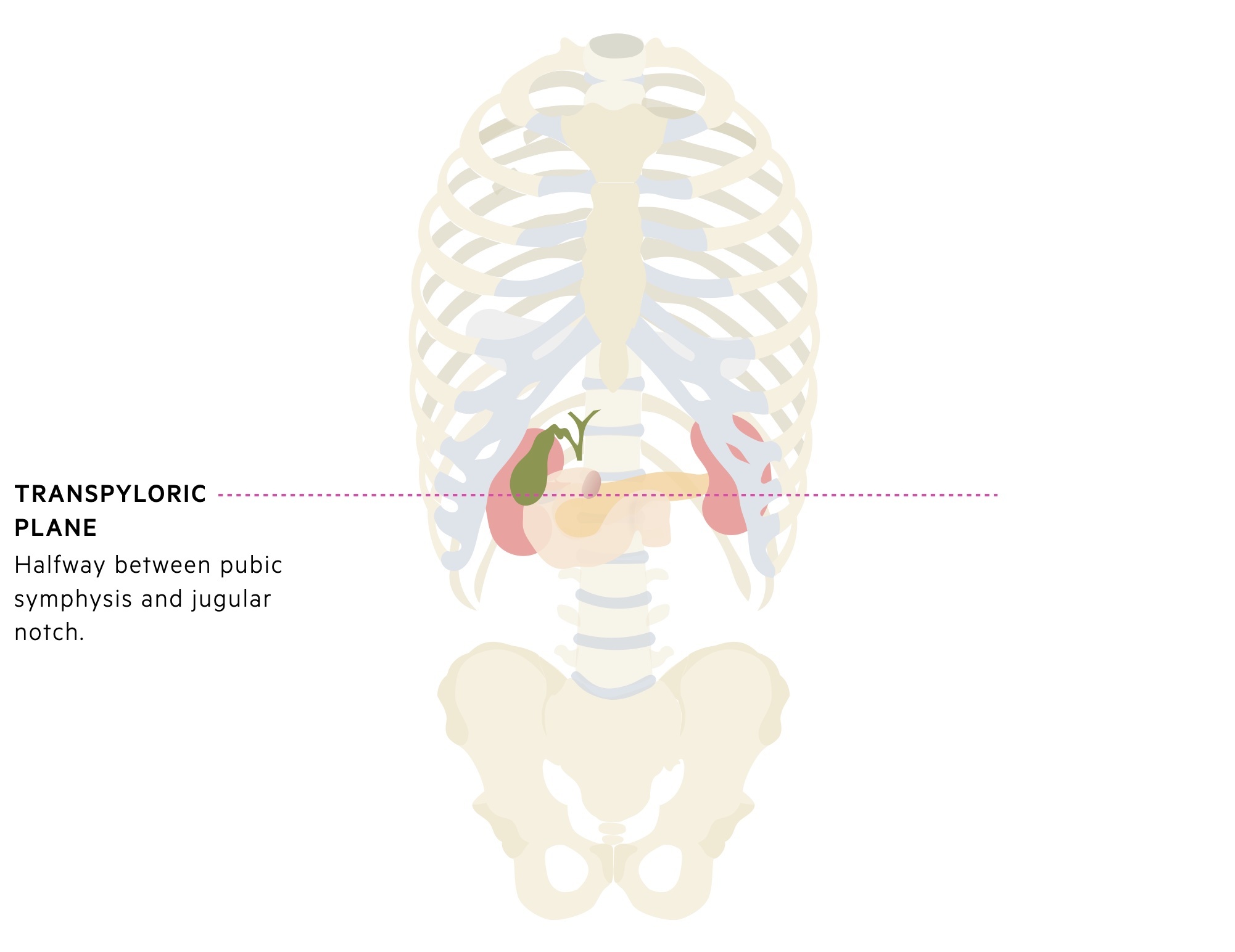
A number of key structures lie on the transpyloric plane:
- L1 vertebrae
- Pancreatic neck
- Pylorus of the stomach
- First part of the duodenum
- Duodenojejunal flexure
- Fundus of the gallbladder
- Renal hila
Skin and soft tissues
The anterolateral abdominal wall is covered by skin, deep to which lies superficial fascia.
Skin
The anterolateral abdominal wall is covered in a non-specialised skin layer. In the postpubertal state, there is a variable degree of extension of the pubic hair on the lower abdominal skin seen particularly in males.
Superficial fascia
Between the skin and muscles of the abdominal wall lies the superficial fascia.
This is divided into:
- Camper's fascia - a superficial fatty layer, which is continuous with the superficial fascia of the thigh and extends into the external genitalia.
- Scarpa's fascia - a deep membranous layer of variable thickness. In the upper abdomen it becomes thinner and less defined. It is continuous with the superficial fascia of the trunk superiorly and extends into the genitalia where, in males, it is continuous with Colles' fascia.
- A third fatty layer is described, which is situated deep to Scarpa's. This layer is seen most clearly in children.
Muscles
The anterolateral abdominal wall is made up of five muscles; rectus abdominis, external oblique, internal oblique, transversus abdominis and pyramidalis.
The muscles of the abdominal wall have multiple functions. They act to protect and contain the abdominal viscera. They are able to contract, increasing intra-abdominal pressure, aiding expiration, coughing and vomiting. Together they help with truncal movements, particularly against resistance.
External oblique
The external oblique is the largest and outermost muscle of the anterolateral abdominal wall.
Origin: external surface of the 5-12th ribs.
Insertion: linea alba, pubic tubercle and anterior half of iliac crest.
Actions: lateral flexion, increase intra-abdominal pressure, maintain abdominal tone.
Vascular supply: intercostal, subcostal and deep circumflex iliac arteries.
Innervation: thoracoabdominal and subcostal nerves.
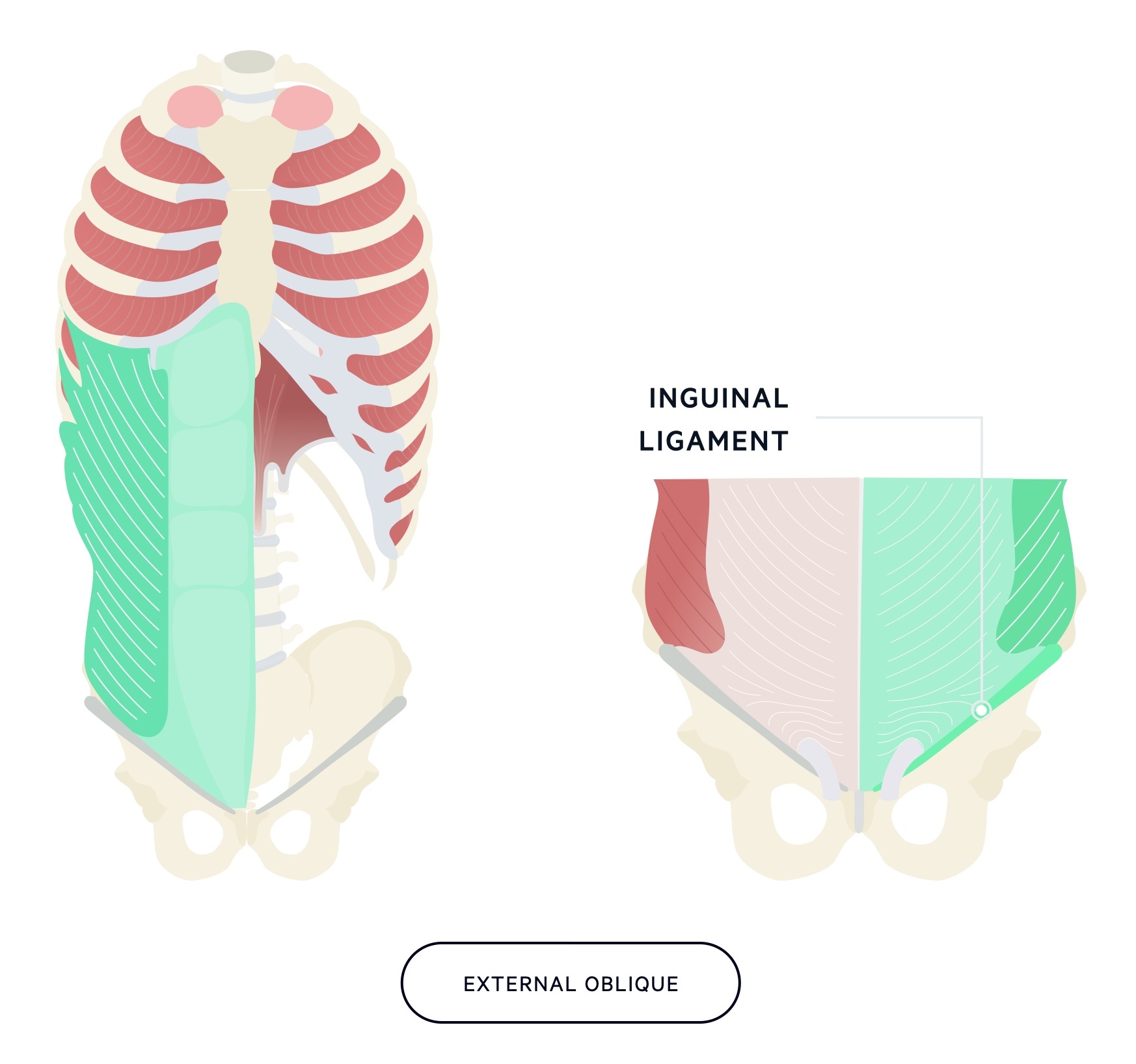
The fibres of the external oblique run inferomedially. As it approaches the midline, the muscle forms an aponeurosis (a broad, flat, tendon) inserting at the linea alba ('white line' formed by the fusion of aponeuroses).
The inferior margin of the aponeurosis of the external oblique muscle is thickened between the ASIS of the iliac crest and the pubic tubercle. This thickened structure is known as the inguinal ligament or “poupart’s ligament”.
Rectus abdominis
The rectus abdominis is a paired, vertical structure running each side of the linea alba and contained within the rectus sheath.
Origin: pubic symphysis & pubic crest.
Insertion: xiphoid process & 5-7th costal cartilage.
Action: flexion of the trunk, maintain abdominal tone.
Vascular supply: superior and inferior epigastric arteries.
Innervation: T6-T11 intercostals, subcostal and ilioinguinal nerves.
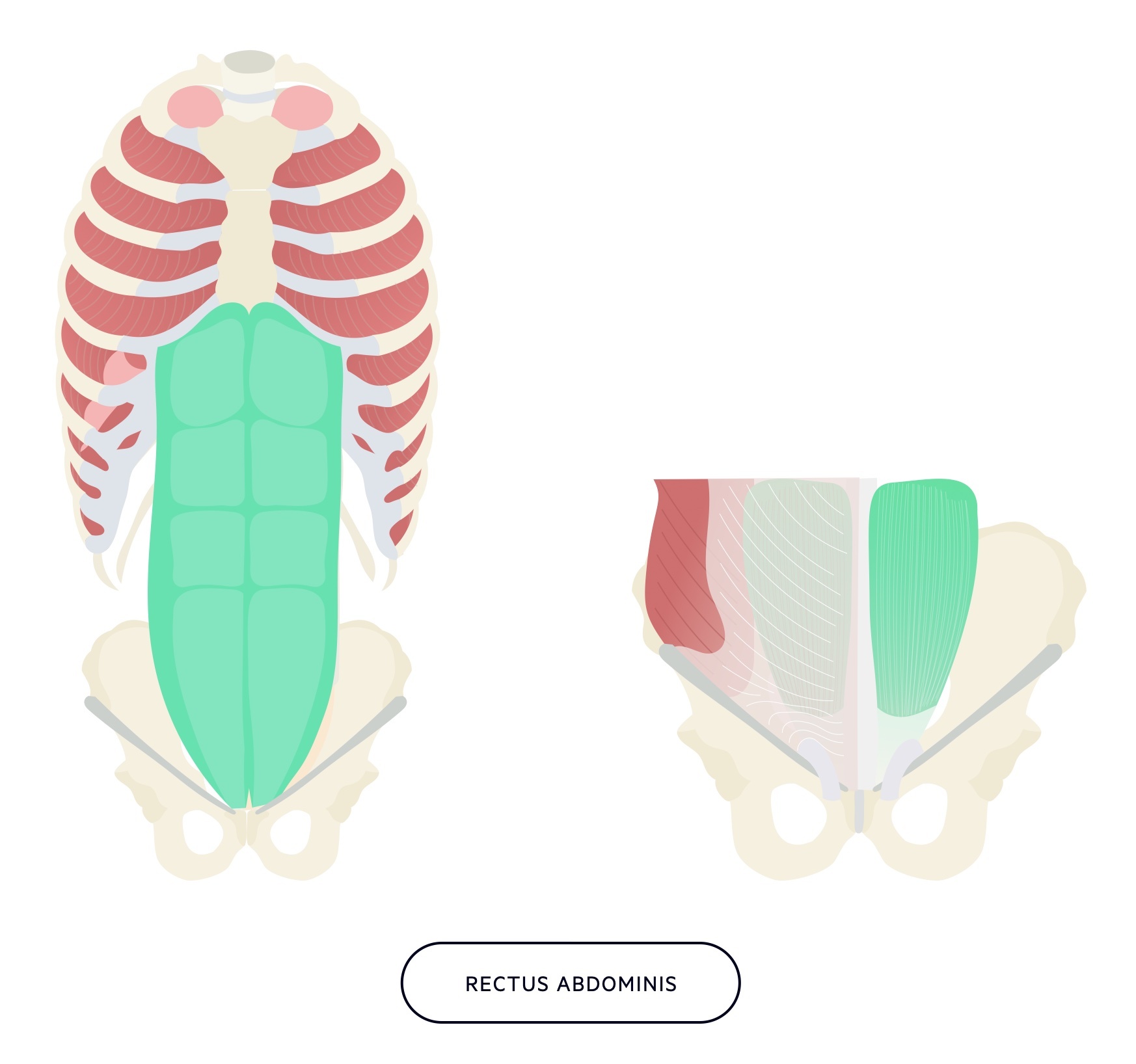
The rectus sheath is formed by the aponeurotic layers of the anterolateral abdominal wall muscles. For more on the rectus sheath please look at our 'Aponeuroses & fascias' chapter.
Internal oblique
The internal oblique is a relatively thin sheet of muscle that forms the intermediate layer of the anterolateral abdominal wall.
Origin: thoracolumbar fascia, iliac crest, iliopectineal arch.
Insertion: 9-12th ribs (aponeurosis as high as 7th costal cartilage), linea alba, pubic crest.
Action: lateral flexion, increase intra-abdominal pressure, maintain abdominal tone.
Vascular supply: intercostal, subcostal, inferior epigastric and deep circumflex iliac artery.
Innervation: T8-T11 intercostals, subcostal, ilioinguinal and iliohypogastric nerves.
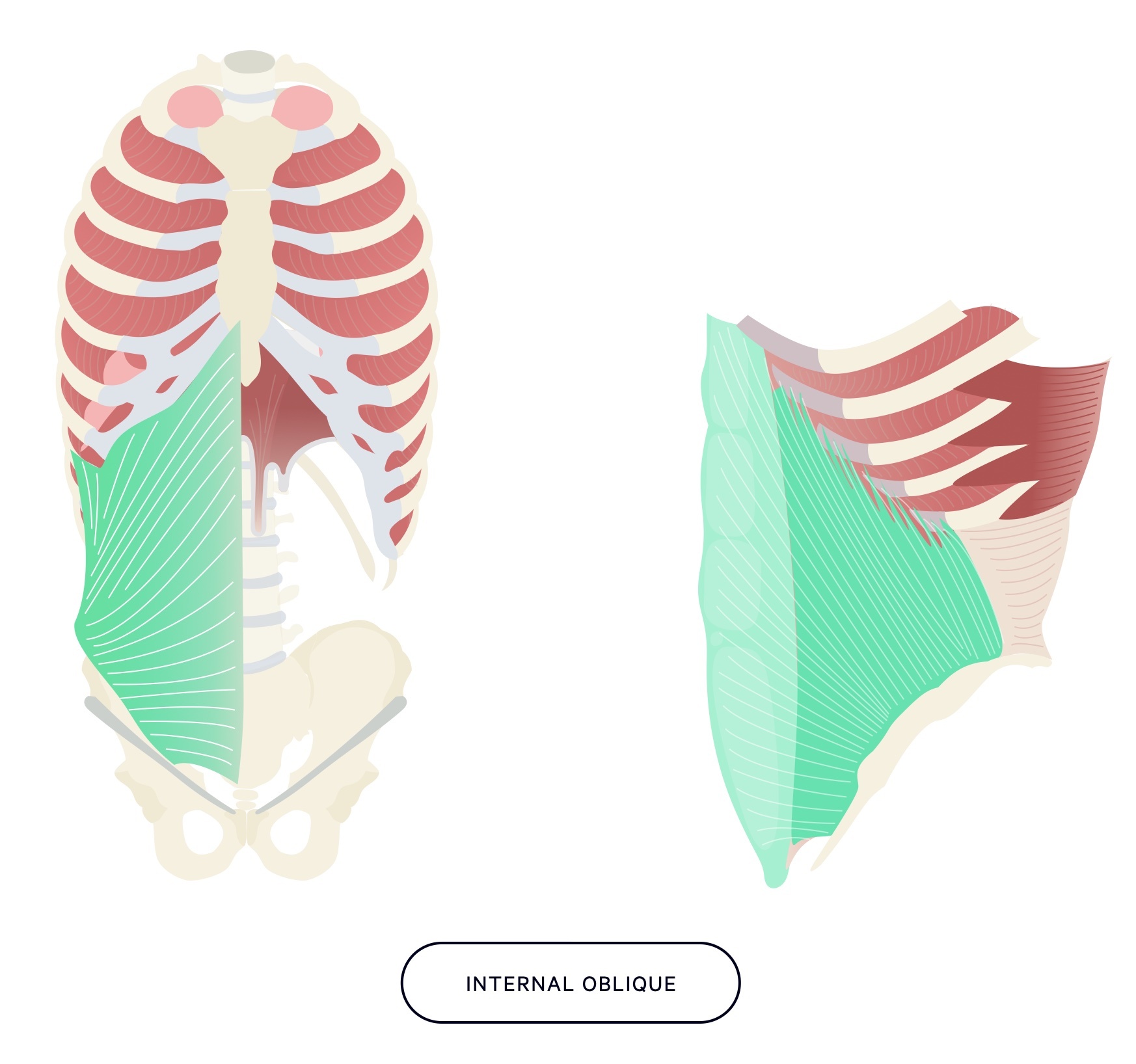
The fibres of the internal oblique run superomedially. As it approaches the midline the muscle forms an aponeurosis (a broad, flat, tendon) inserting at the linea alba.
Transversus abdominis
The two transversus abdominis muscles form the innermost layer of muscle of the anterolateral abdominal wall.
Origin: 7-12th ribs, thoracolumbar fascia, iliac crest, inguinal ligament.
Insertion: linea alba, pubic crest, pectineal line.
Action: increase intra-abdominal pressure, maintain abdominal tone.
Vascular supply: intercostal, subcostal, superior/inferior epigastric, superficial/deep circumflex iliac and posterior lumbar arteries.
Innervation: T7-11 intercostals, subcostal, ilioinguinal and iliohypogastric nerves.
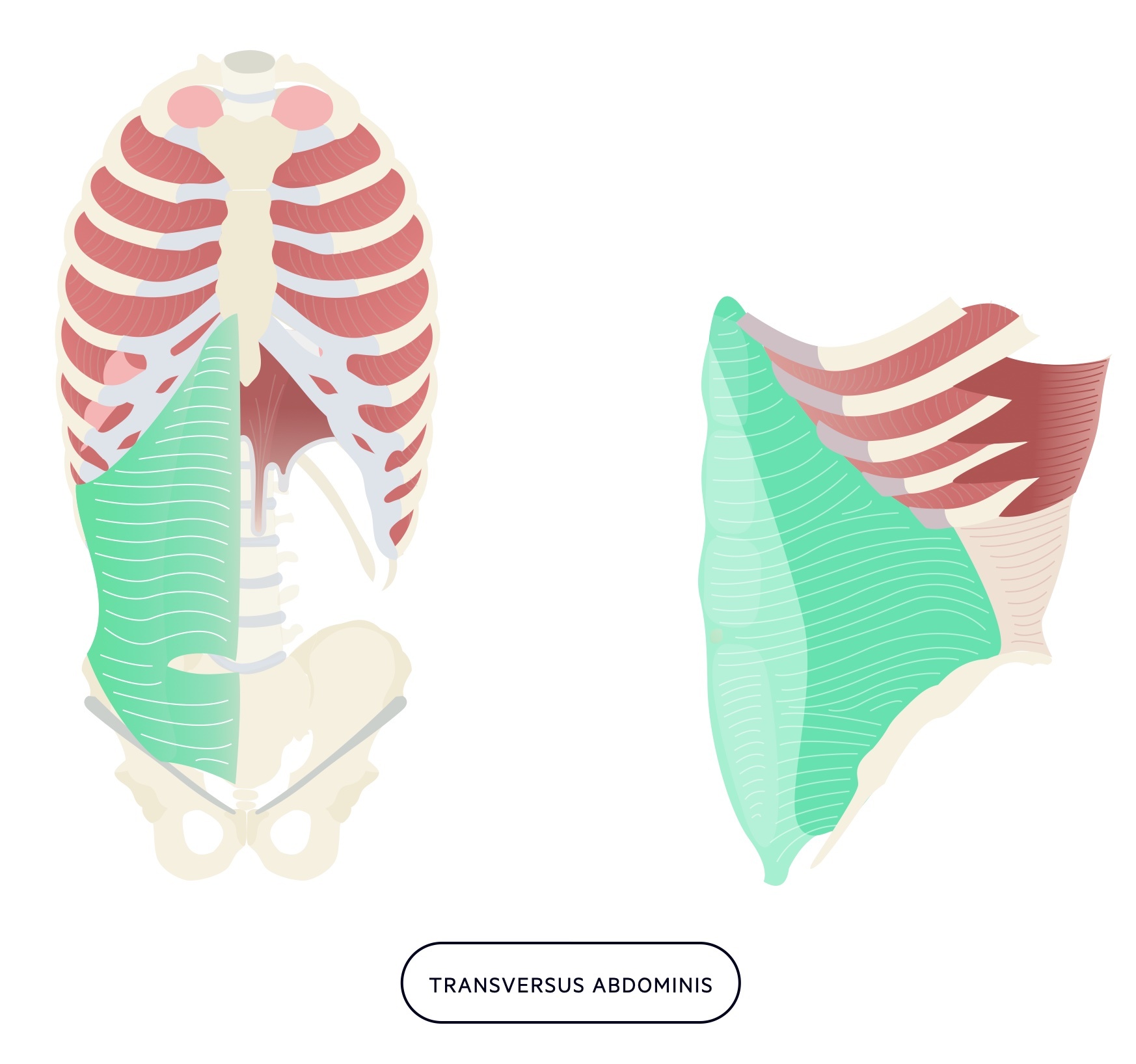
The fibres of the transversus abdominis run transversely. As it approaches the midline the muscle forms an aponeurosis (a broad, flat, tendon) inserting at the linea alba.
Pyramidalis
The pyramidalis is small triangular muscle that is located anterior to the inferior part of the rectus abdominis.
Origin: pubic symphysis and pubic crest.
Insertion: linea alba.
Action: tenses the linea alba.
Vascular supply: inferior epigastric artery.
Innervation: subcostal nerve.
The pyramidalis sits in the rectus sheath anterior to the lower rectus abdominis. It is thought to have little clinical significance and is absent in 20% of people.
Aponeuroses & fascias
The bilaminar aponeuorses of the external oblique, internal oblique and transversus abdominis form a sheath around the rectus abdominis.
Aponeuroses
Three flat muscles make up the anterolateral abdominal wall, the external oblique, internal oblique and transversus abdominis. Sitting most anteriorly are the rectus abdominis muscles, more colloquially known as ‘abs’.
The three flat muscles of the anterolateral abdominal wall form bilaminar aponeuroses (flat, broad tendons) as they approach the midline, fusing at the linea alba. Together they form a sheath around the rectus abdominis muscles known as the rectus sheath.
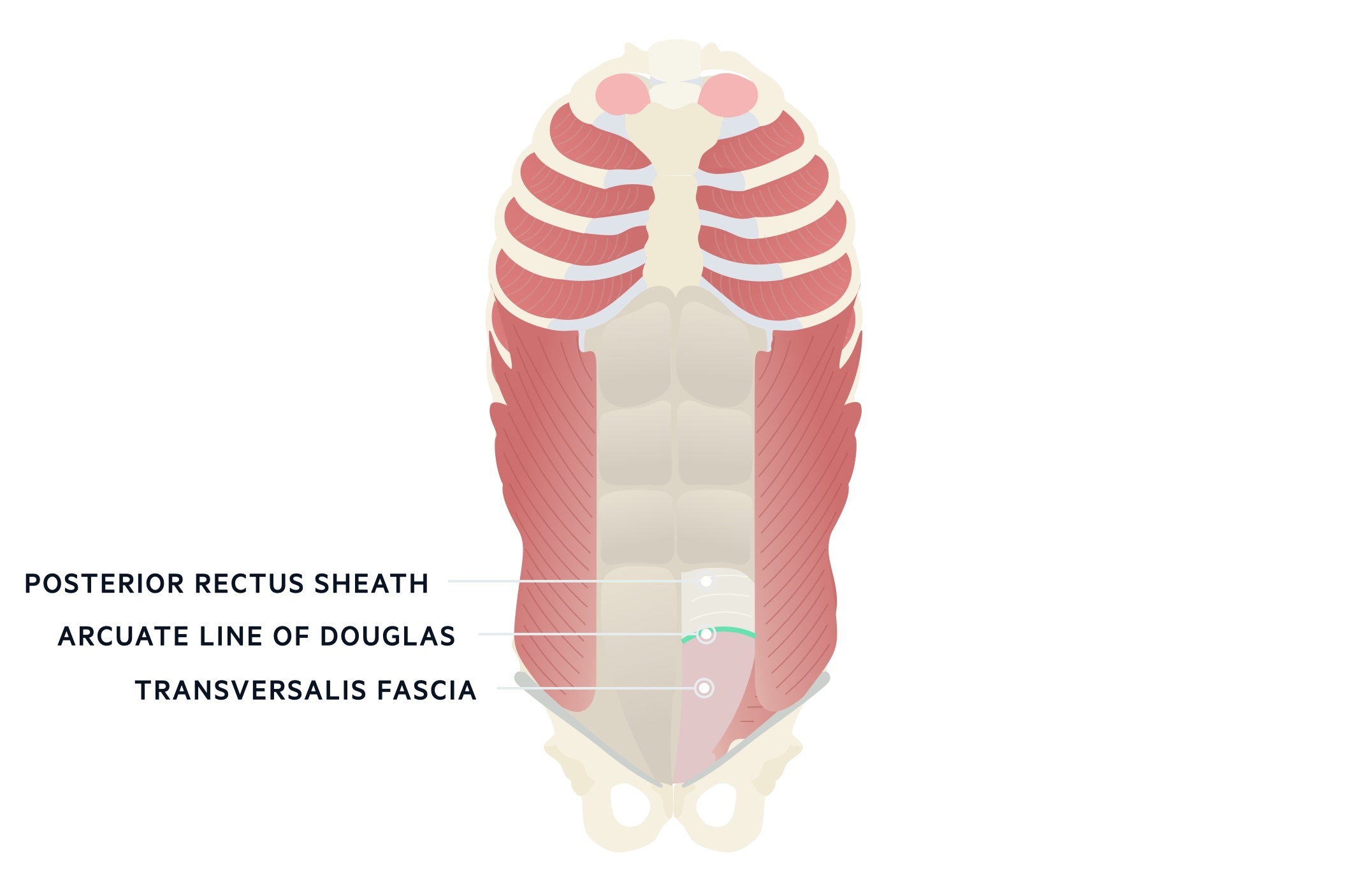
Rectus sheath
The rectus sheath is a fibrous structure that envelops the rectus abdominis muscles. The anterior component of the rectus sheath is continuous along the entire length of the rectus abdominis muscle. Above the costal margin only the external oblique contributes to the anterior rectus sheath. At this level the posterior rectus sheath is deficient.
Between the costal margin and the arcuate line (arcuate line of Douglas, linea semicircularis) both the anterior and posterior rectus sheath receive contributions from each of the aponeuroses of the anterolateral muscles. Below the arcuate line all the fibres of the aponeuroses pass anteriorly leaving the rectus abdominis sitting directly on the transversalis fascia below. The arcuate line is created by the lower border of the posterior rectus sheath.
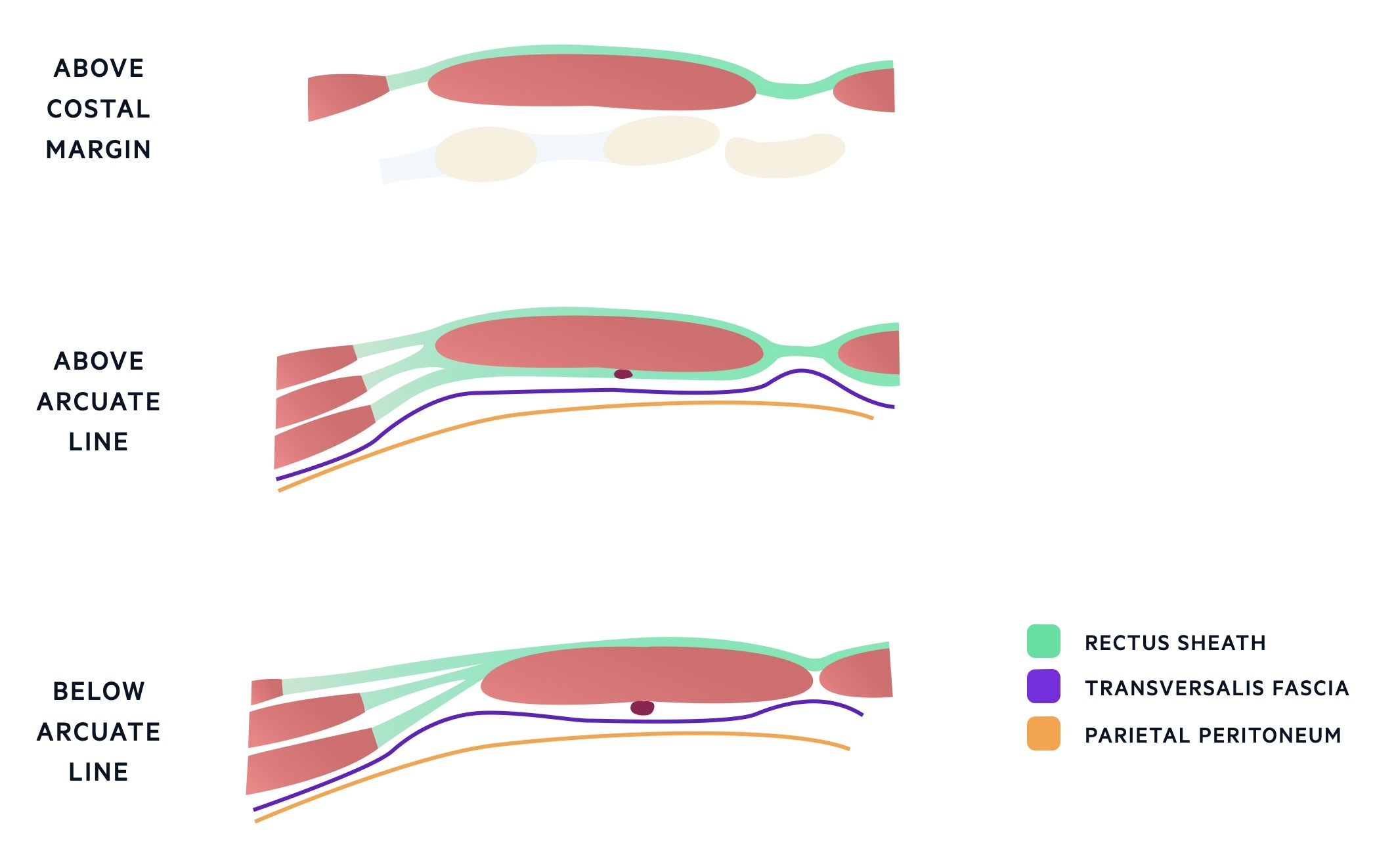
Fascia, fat & peritoneum
The transversalis fascia is a layer of connective tissue found deep to the transversus abdominis. The fascia is continuous with the thoracolumbar fascia posteriorly, a fascia of the diaphragm superiorly and the iliac and pelvic fascia inferiorly.
Two inferior thickenings of the transversalis fascia form the iliopubic tract and interfoveolar ligament that run alongside and below the inguinal ligament respectively. The fascia is continuous with that of the internal spermatic fascia.
Between the transversalis fascia and parietal peritoneum lies a layer of extraperitoneal fat of variable thickness. Immediately deep to this lies the parietal peritoneum.
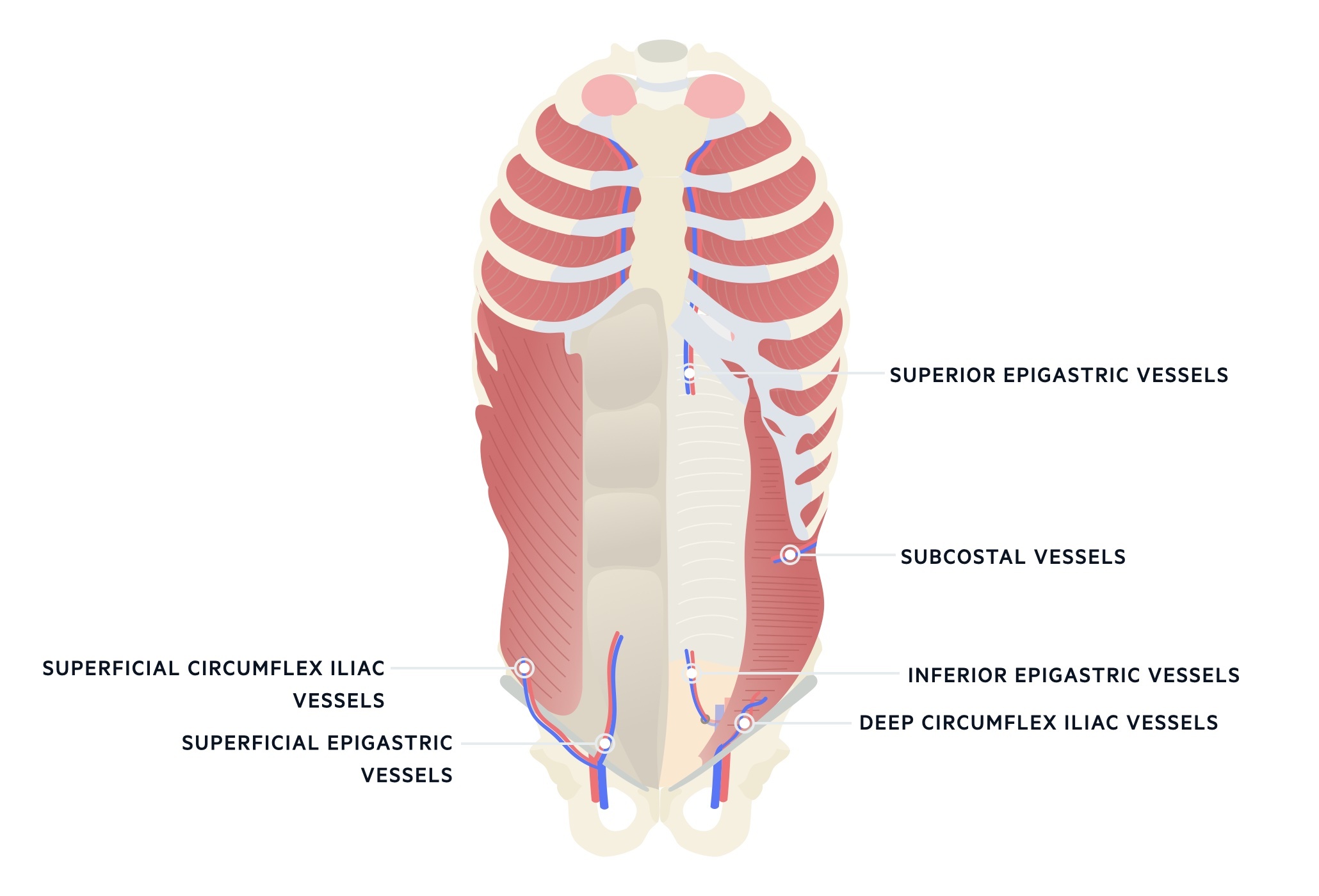
Vasculature
The abdominal wall receives a complex blood supply from a number of contribuiting arteries.
Superior branches
The internal thoracic artery terminates at the level of the sixth costal cartilage into the superior epigastric artery and the musculophrenic artery. The superior epigastric artery runs inferiorly branching and forming an anastomosis with the inferior epigastric artery above the umbilicus.
The musculophrenic artery and the lower anterior intercostal arteries offer contributions to the vascular supply of the abdominal wall though these are less significant than the superior epigastric artery.
Inferior branches
The inferior epigastric artery branches from the external iliac artery. It anastomoses with the superior epigastric vessel around the umbilicus and helps supply the anterior abdominal wall.
The deep circumflex iliac artery arises from the external iliac artery almost opposite the origin of the inferior epigastric artery. It pierces the transversus abdominis to lie behind the internal oblique. The superficial circumflex iliac and superficial epigastric arteries arise from the femoral artery and supply the lower abdominal wall.
Lateral branches
The lateral supply is from the posterior intercostal, subcostal and lumbar arteries arising from the thoracic and abdominal aorta. They supply the musculature that accompanies their course, running in a neurovascular plane deep to the internal oblique.
Innervation
The innervation of the anterolateral abdominal wall follows a segmental pattern from the anterior rami of T6-T12 and L1.
Spinal roots T6-L1 supply the anterolateral abdominal wall. This is in the form of the T6-T11 intercostal nerves, the subcostal nerve (arising from the T12 spinal nerve root) and the iliohypogastric and ilioinguinal nerves (arising from the L1 spinal nerve root).
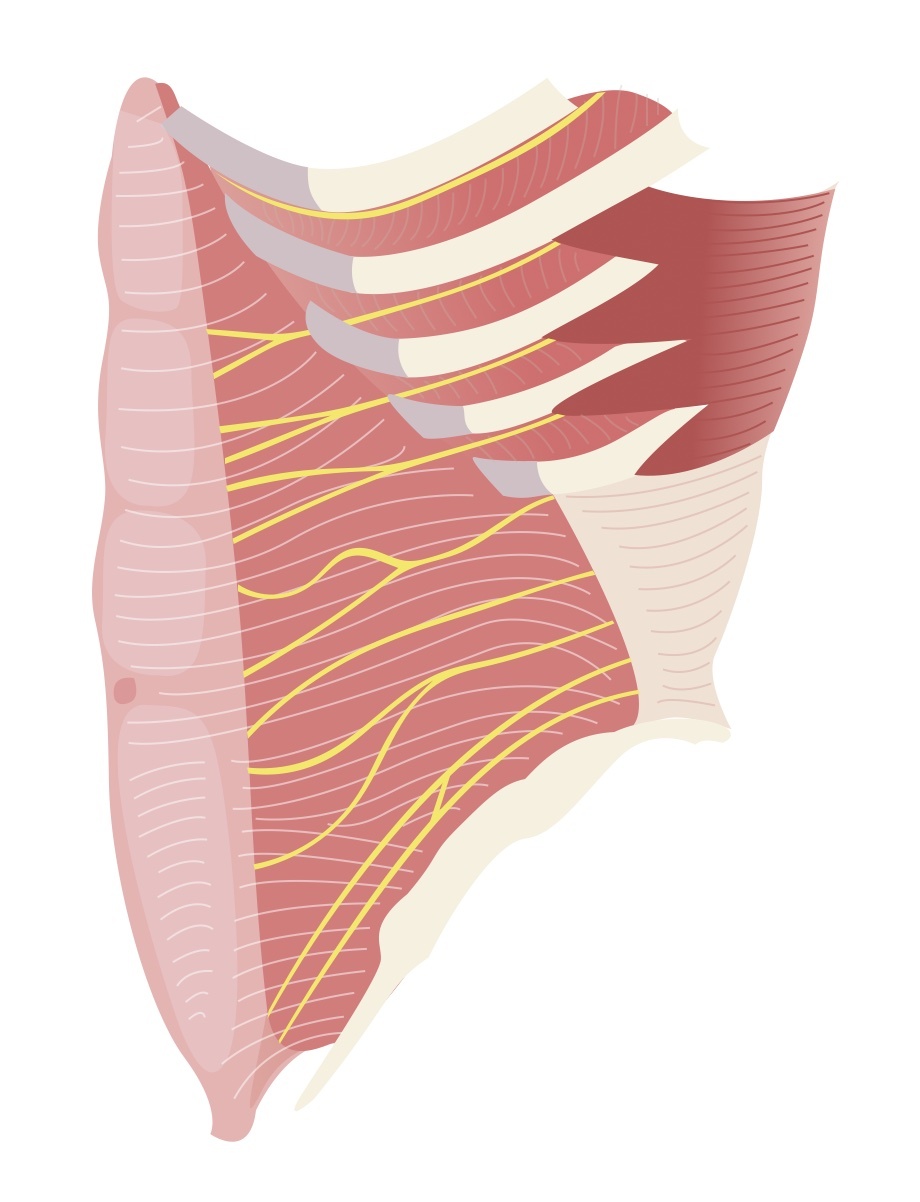
Intercostal & Subcostal
The upper part of the abdomen is innervated by the spinal nerves T6-T11, primarily T7-T11 which are also termed the thoracoabdominal nerves. The T10 nerve root reliably innervates the skin around the umbilicus.
The subcostal nerve arises from the anterior rami of the T12 nerve root. It runs inferior to the 12th rib and to the anterolateral abdominal wall.
Iliohypogastric
The iliohypogastric nerve is the superior terminal branch of the L1 nerve root.
Ilioinguinal
The ilioinguinal nerve is the inferior terminal branch of L1 nerve root.
Last updated: March 2021
Have comments about these notes? Leave us feedback
