Spinal cord syndromes
Notes
Overview
Several classic syndromes that have characteristic clinical features based on the area of the spinal cord that is affected.
Neurological signs and symptoms can usually be located to the spinal cord based on the presentation of bilateral motor and sensory signs without head or face involvement.
In some situations, a specific set of clinical features can develop due to the area within the spinal cord that is affected. These are known as the spinal cord syndromes. We discuss some of the more common ones below.
Anatomy
The spinal cord is part of the central nervous system (CNS) and forms the main communication between the brain and peripheral nerves.
The spinal cord originates at the base of the medulla oblongata, exiting the skull through the foramen magnum. It then extends through the spinal canal and ends at the level of the L1/L2 spinal vertebrae.
It is divided into four main regions termed cervical, thoracic, lumbar, and sacral. This is further divided into 31 spinal cord segments. Arising from the 31 spinal cord segments are the paired ventral and dorsal spinal nerve roots, which join to form the 31 paired spinal nerves.
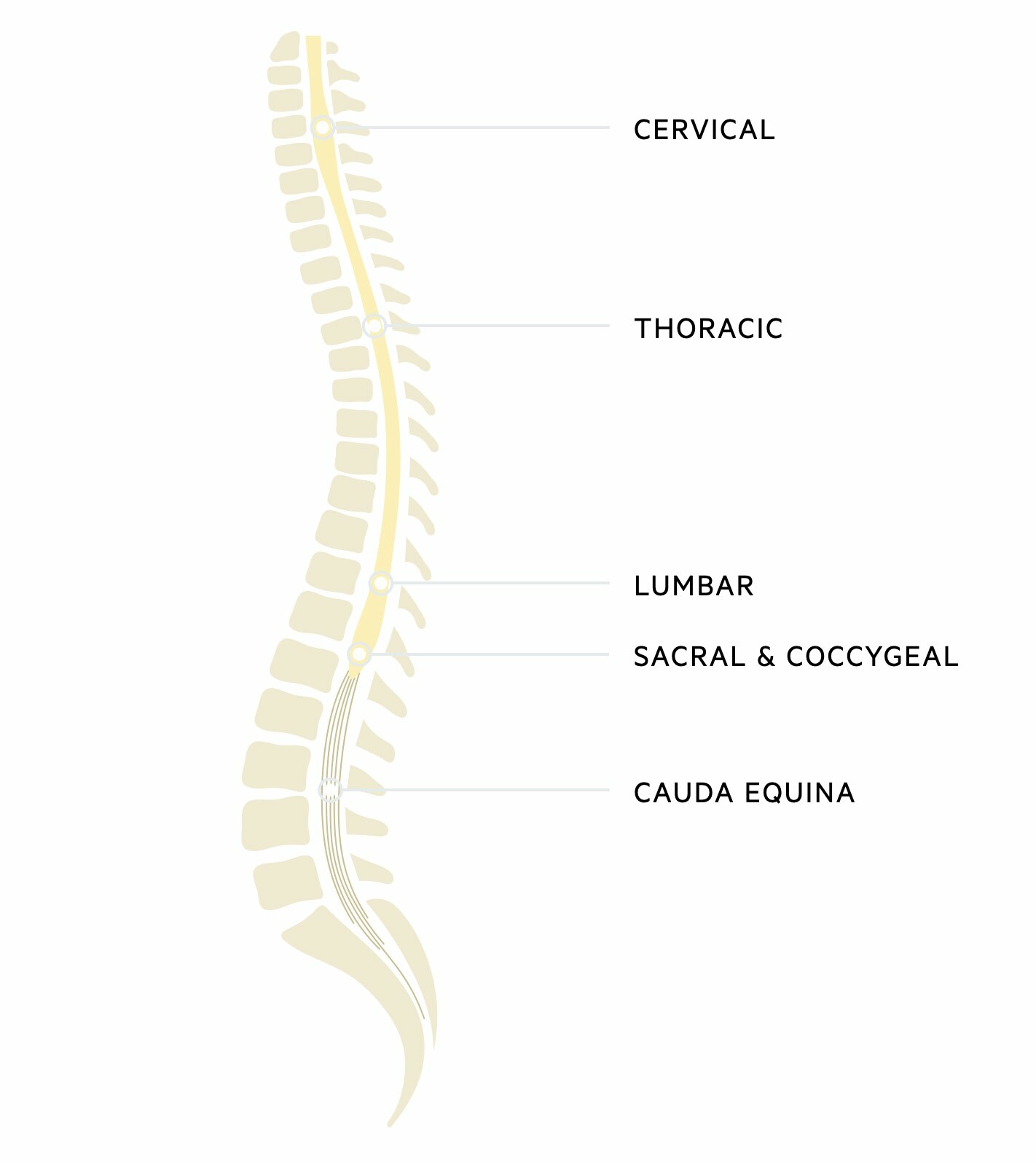
Cauda equina
The terminal end of the spinal cord is termed the conus medullaris. Beyond this is a collection of spinal nerves composed of lumbar, sacral, and coccygeal nerves. Together these make up the cauda equina. These nerves have important innervation for lower extremity motor function, perianal sensation, and parasympathetic sensation to the bladder and bowel including the sphincters.
Blood supply
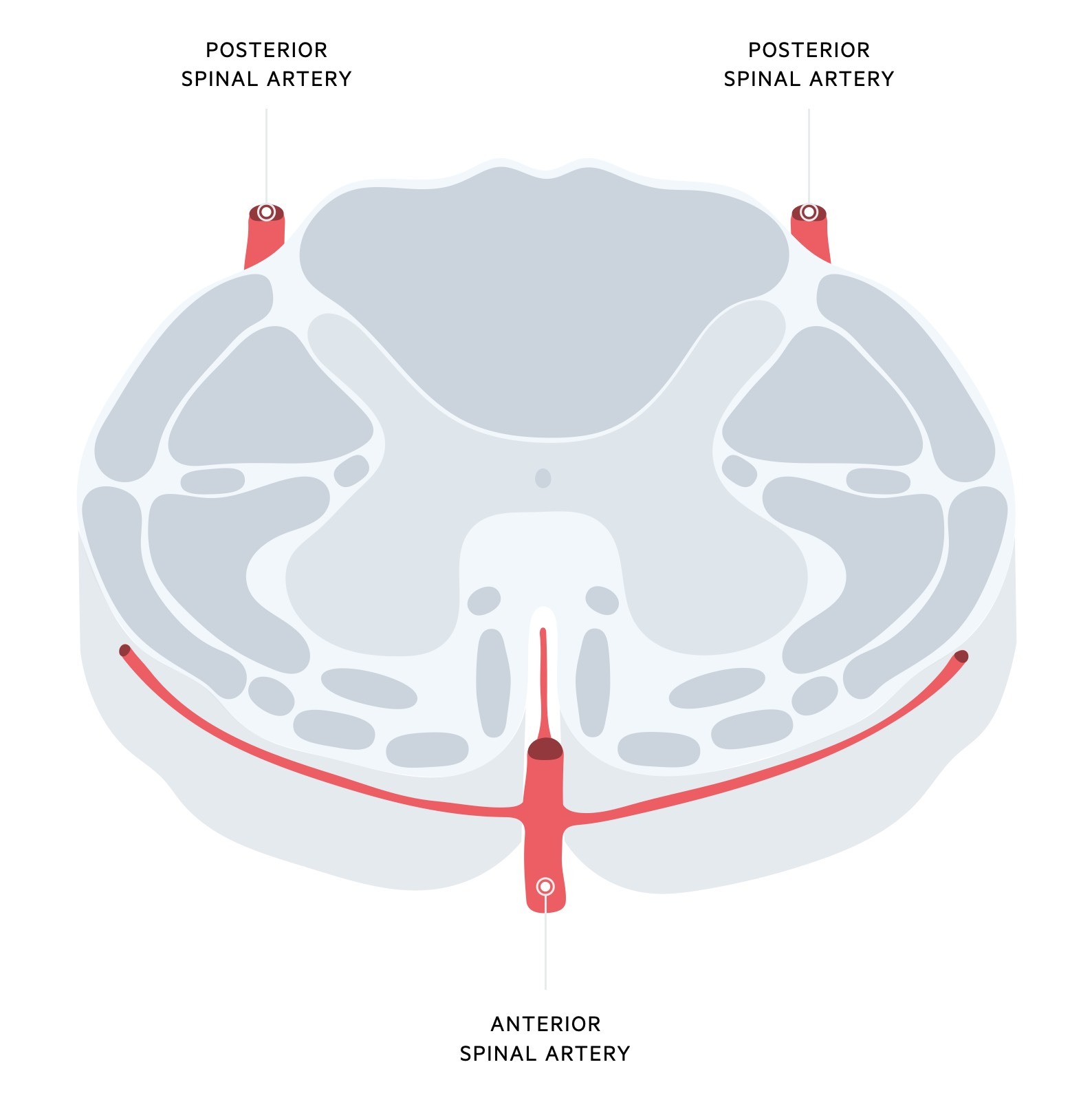
The spinal cord is supplied by three longitudinal arteries
- Anterior spinal artery (single): arises from the vertebral arteries near the brainstem. Supplies the anterior two-thirds of the spinal cord.
- Posterior spinal artery (dual): arises from the posterior inferior cerebellar artery or vertebral arteries. Supplies the posterior one-third of the spinal cord.
As the arteries course down the cord, many arteries including the cervical, intercostal and lumbar provide contributions that reinforce the arterial supply. A major contribution to the anterior spinal artery within the thoracolumbar region is a vessel known as the spinal artery of Adamkiewicz. This may become affected in aortic disease leading to neurological symptoms (e.g. thoracic aortic dissection).
Physiology
The spinal cord has many bundles of nerves called tracts that transmit information from the brain to peripheral tissue.
Within the spinal cord are many ascending and descending spinal tracts. These are pathways that carry information up and down the spinal cord to communicate between the brain and body.
- Ascending tracts: carry sensory information to the brain (e.g. pain, temperature)
- Common tracts: Spinothalamic tracts, dorsal columns
- Descending tracts: carry motor information to the body (e.g. to move your leg)
- Common tracts: Corticospinal tracts
The ascending and descending tracts are organised into discrete structures that are essentially bundles of myelinated nerve axons within the white matter of the cord that contain similar information. Each tract is named according to its anatomical location within the white matter of the spinal cord.
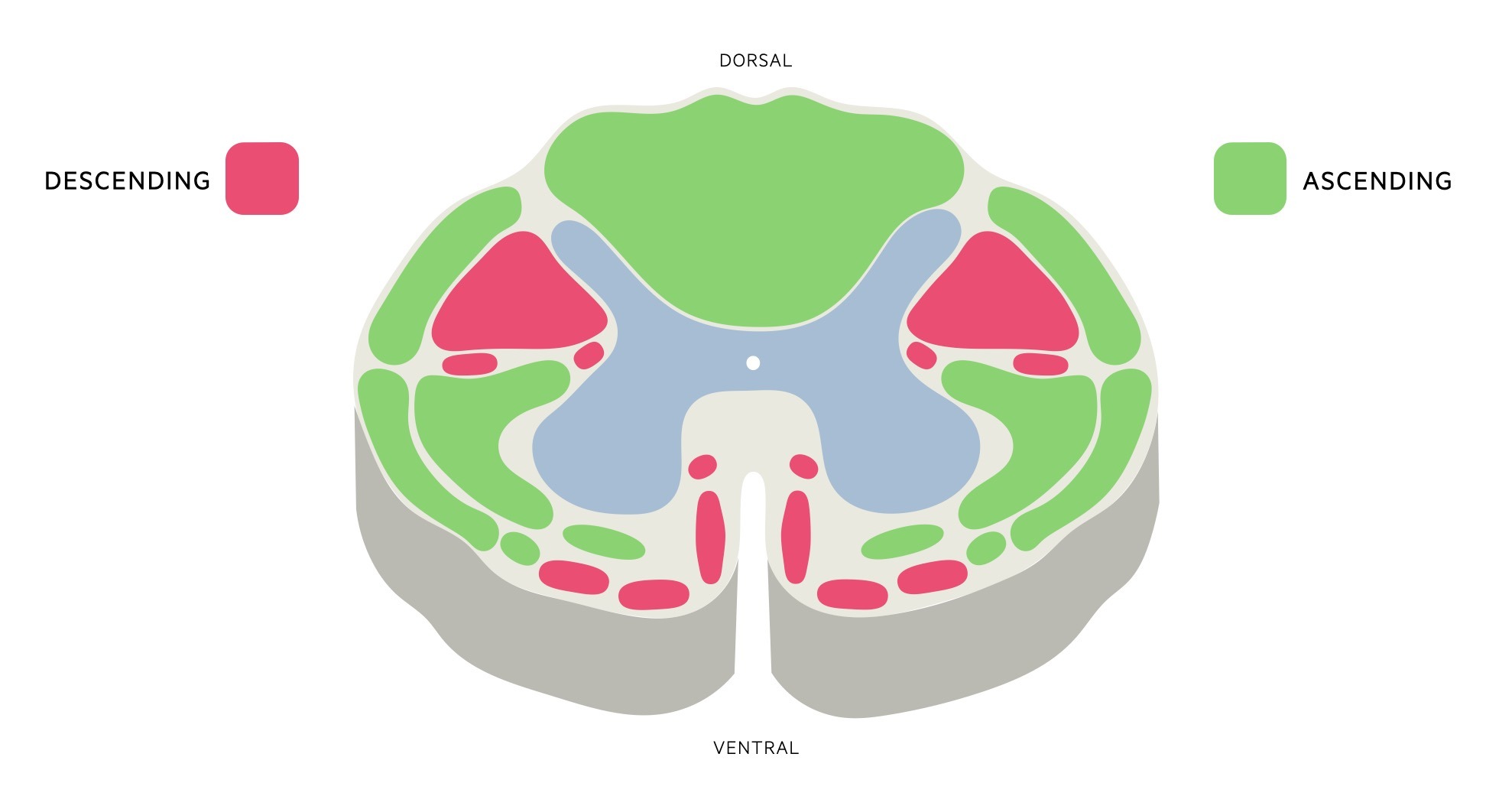
Each tract is bilaterally paired. Importantly, many of these tracts cross from left to right or right to left at different points along the spinal cord or in the brain stem. This crossing is known as ‘decussation’ and means that information from the right hemisphere of the brain is transmitted to the left side of the body and vice versa.
We discuss some of the more common tracts to help us understand the spinal cord syndromes.
Spinothalamic tracts
These are ascending tracts that carry information about pain, temperature, and crude touch from our skin to the thalamus in the brain. It is composed of two major pathways:
- Anterior spinothalamic tract: carries crude touch information
- Lateral spinothalamic tract: carries pain and temperature information
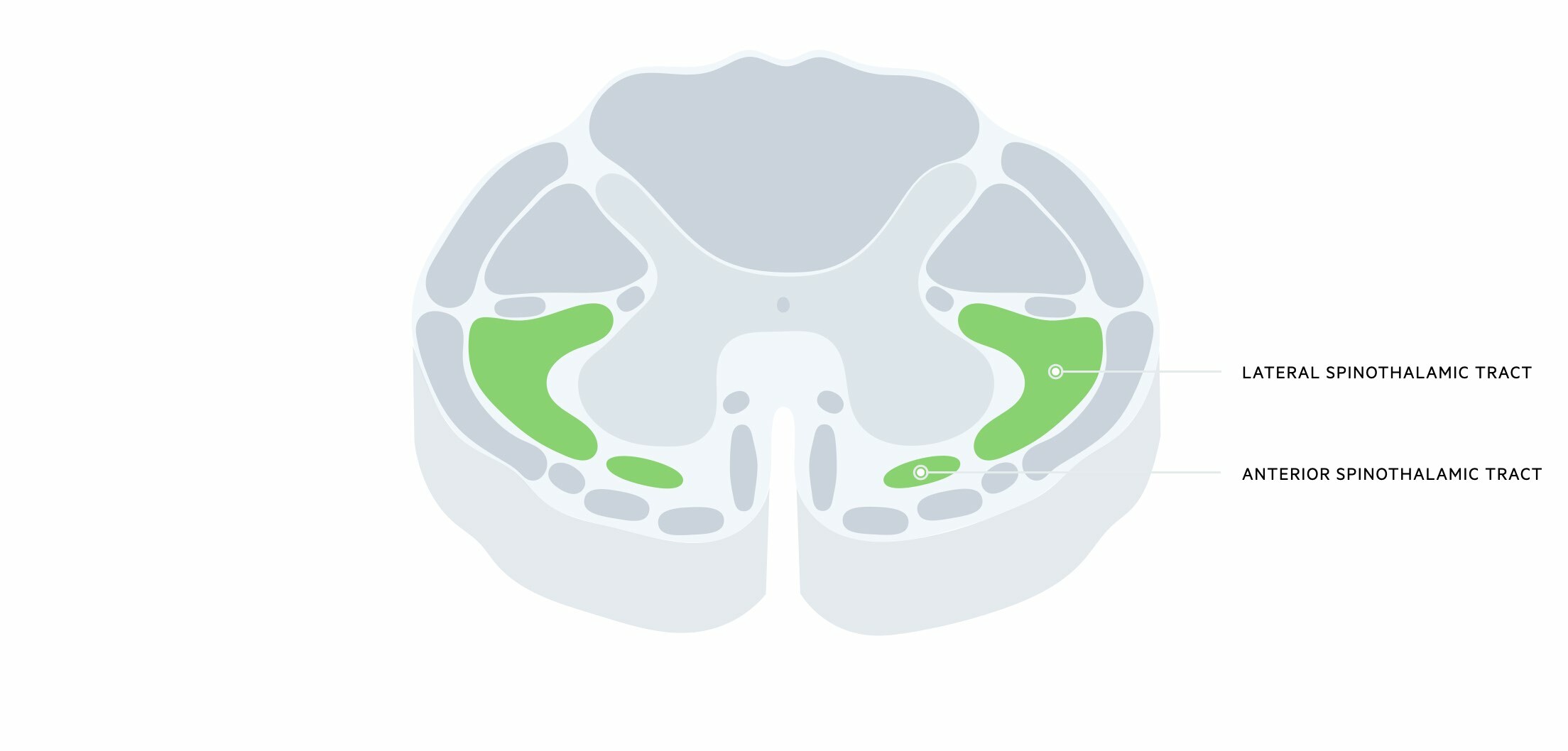
Sensory receptors pass information to the dorsal root ganglia. Located in the dorsal root ganglia is a pseudounipolar (first-order) neuron with a distal axon that extends to the site of sensory receptors and a central neuron that enters the spinal cord. This central neuron synapses with second-order neurons in the gray matter. This second-order neuron then crosses to the opposite side and travels up the spinal cord in the spinothalamic tract. They synapse with third-order neurons in the thalamus.
Thus, fibres cross at the spinal cord level.
Dorsal columns
These are ascending tracts that carry information about fine (i.e. light) touch, vibration, and proprioception (i.e. spatial location of body parts). It is located in the dorsal part of the spinal cord, hence the name. The dorsal columns are divided into two components:
- Fasciculus gracilis: carries sensory information from lower extremities. Located throughout the length of the cord and lies medially.
- Fasciculus cuneatus: carries sensory information from upper extremities. Located from T6 upwards and lies laterally.
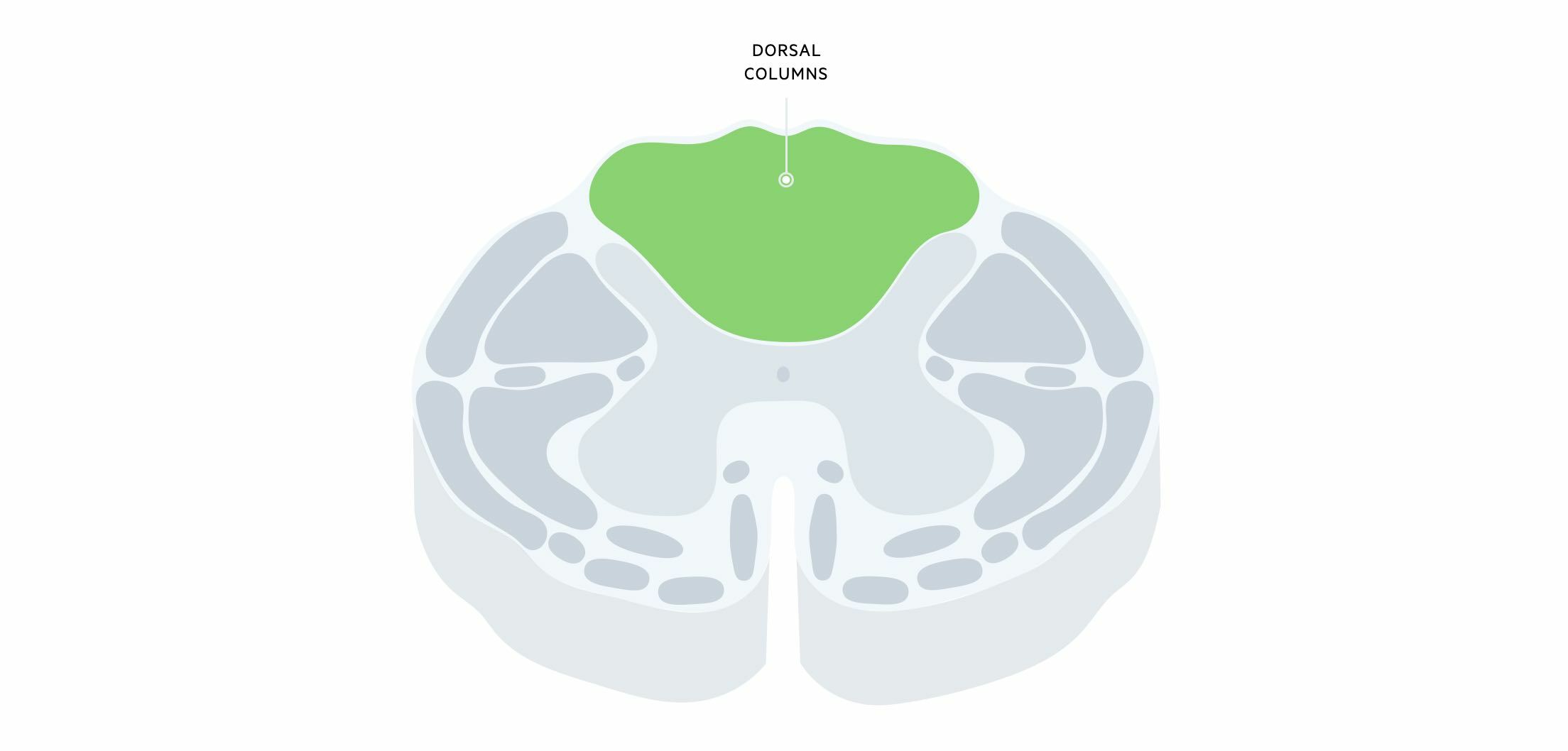
Sensory receptors from the skin and joints send information to the dorsal root ganglia via the distal axon of the pseudouniploar (first-order) neuron. Here, the central axon of these neurons enter the spinal cord and the majority enter the dorsal columns and ascend (without synapsing) to reach the medulla oblongata. They synapse with nuclei of second-order neurons within the caudal aspect of the medulla, which then crosses the midline (decussate). Fibres then travel through the brainstem via the medial lemniscus pathway that synapses with third-order neurons in the thalamus.
Thus, fibres cross at the level of the brainstem.
Corticospinal tracts
These are descending tracts that carry important information for voluntary motor control. They are also known as the ‘pyramidal tracts’ due to the large pyramidal decussation within the medulla oblongata. This tract is divided into two components:
- Lateral corticospinal tract: contains the 75-90% of fibres that cross at the medulla. Hence, contain information from the contralateral hemisphere (e.g. left lateral corticospinal tract has information from the right hemisphere of the brain).
- Anterior corticospinal tract: contains the 10-15% of fibres that do not cross at the medulla. These only regulate thoracic and cervical segments.
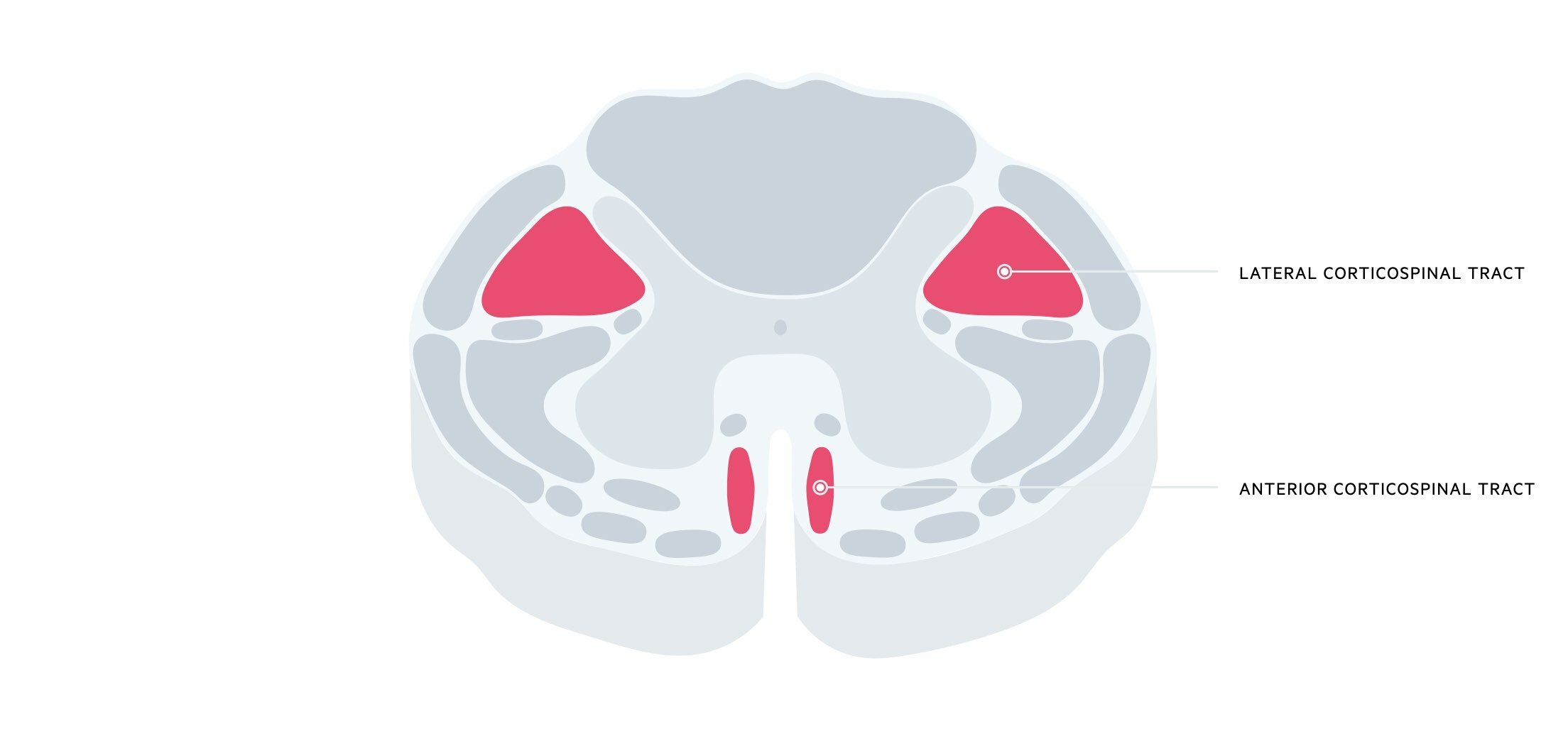
Motor information from the primary motor cortex travels in neuron bundles via the internal capsule to the cerebral peduncles. These bundles of neurons become more compact as they travel through the brainstem. At the Medulla, 75-90% of fibres decussate to the contralateral side and travel through the spinal cord in the lateral corticospinal tract, and 10-15% do not decussate and travel through the spinal cord in the anterior corticospinal tract.
Neurons within these tracts then synapse with neurons in the anterior horn of the gray matter. Fibres in the anterior corticospinal tract decussate at their target level within the spinal cord. The cell body of the neuron within the gray matter is known as an anterior horn cell and projects axons to innervate skeletal muscle.
Thus, fibres predominantly cross at the level of the brainstem.
Complete versus incomplete
Injuries to the spinal cord may be complete or incomplete.
A complete cord syndrome is characterised by a complete loss of function (motor/sensory) below the level of the lesion.
An incomplete cord syndrome is characterised by variable neurological function below the level of the injury depending on the area of the cord that is affected.
Posterior cord syndrome
A clinical syndrome due to damage to the posterior aspect of the spinal cord.
Posterior cord syndrome, also known as dorsal cord syndrome, is a rare syndrome due to injury of the posterior aspect of the spinal cord. This area is predominantly housed by the dorsal columns that are ascending tracts carrying information on light touch, proprioception, and vibration.
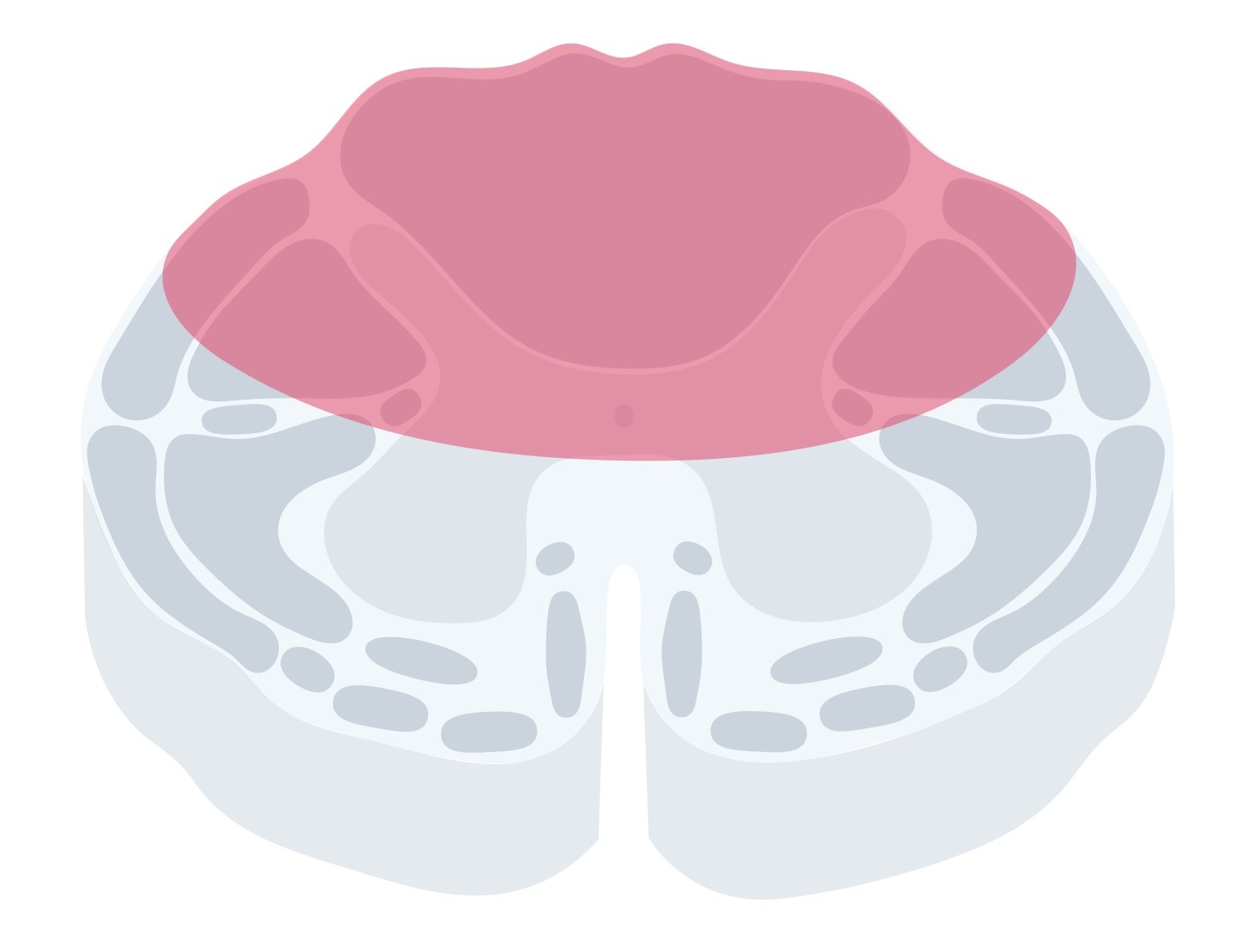
Clinical features
The syndrome is characterised by gait ataxia (abnormal, uncoordinated gait with a wide base and irregular foot placement), abnormal vibration sense, and paraesthesia below the level of the injury.
In large lesions, it may involve the lateral corticospinal tracts leading to weakness.
Aetiology
Many conditions can cause posterior cord syndrome. Some may cause an acute injury, whereas others are slowly progressive.
- Inflammatory (e.g. multiple sclerosis)
- Syphilis
- Ischaemia (e.g. posterior spinal artery syndrome)
- Malignancy
- Metabolic (e.g. subacute degeneration of the cord due to vitamin B12 deficiency)
- Hereditary (e.g. Friedreich ataxia)
Anterior cord syndrome
A clinical syndrome due to damage to the anterior two-thirds of the spinal cord.
Anterior cord syndrome, also known as ventral cord syndrome, refers to damage to the anterior two-thirds of the spinal cord irrespective of aetiology. This area contains many important tracts leading to a wide range of symptoms including the corticospinal tracts, spinothalamic tracts and autonomic tracts important for bladder control.
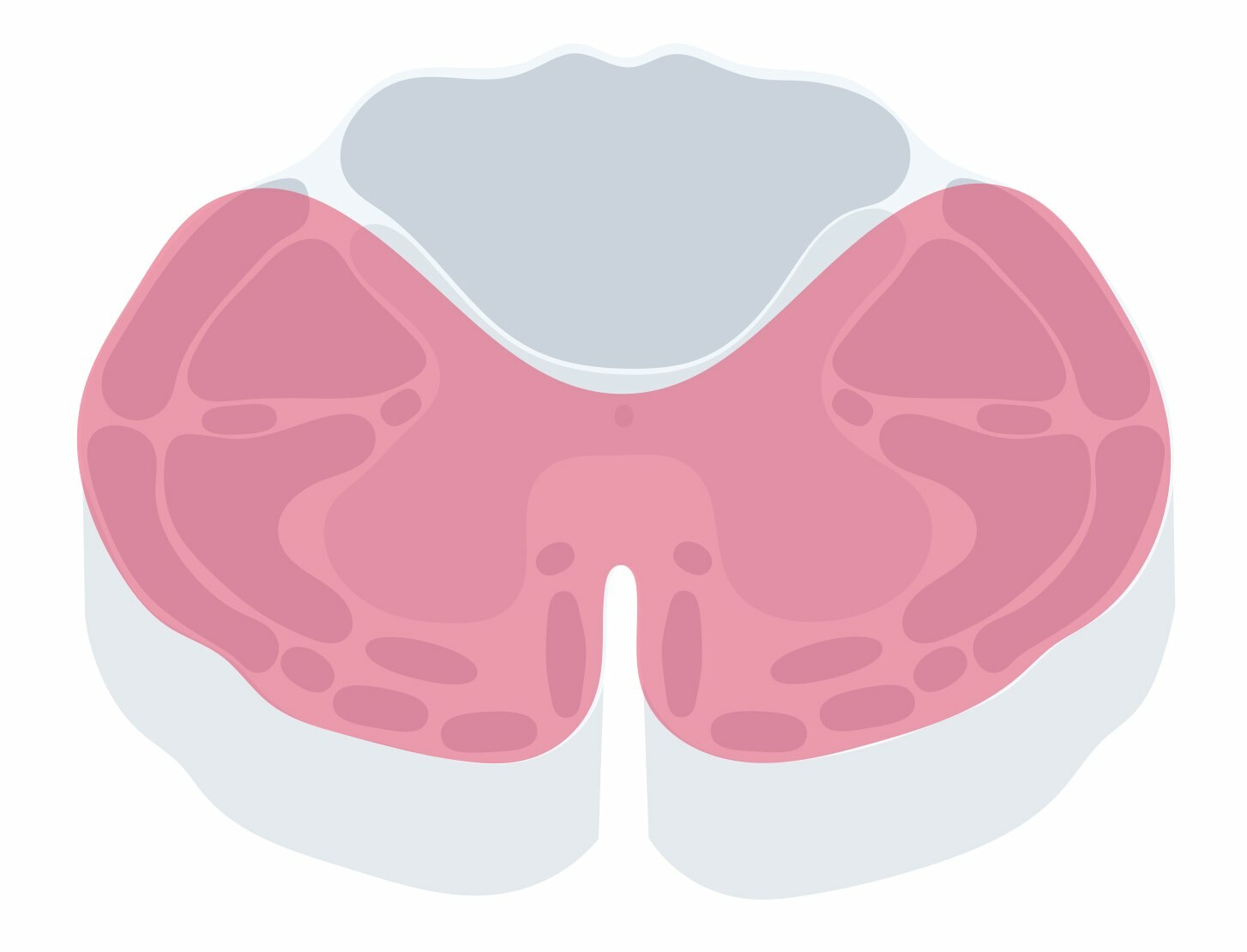
Clinical features
The syndrome is characterised by a broad range of clinical features:
- Bilateral weakness (paraplegia or quadriplegia): depends on the level of the lesion
- Bilateral loss of pain and temperature
- Autonomic dysfunction: abnormal blood pressure
- Bladder dysfunction: Urinary incontinence
Aetiology
Anterior cord syndrome is commonly due to ischaemia of the anterior spinal artery, which results in an acute presentation. Anything that limits flow through the anterior spinal artery is known as anterior spinal artery syndrome and this gives rise to the cord syndrome:
- Thromboembolism
- Trauma
- Hypotension
- Aortic disease (e.g. aortic aneurysm, thrombosis, dissection): damage the arteries that contribute to the anterior spinal artery
Alternatively, any pathology that damages the anterior spinal cord can lead to the syndrome:
- Disc herniation
- Tumour
- Trauma
- Epidural collection
Brown-Sequard syndrome
A clinical syndrome due to hemisection of the cord.
Brown-Sequard syndrome, also known as hemisection of the cord, is a classic cord syndrome that results in ipsilateral (same side as the lesion) weakness and proprioception/vibration loss, and contralateral (opposite side to the lesion) pain/temperature loss. It is typically due to damage to one-half of the cervical or thoracic spinal cord.

Clinical features
Brown-Sequard is a rare cord syndrome that presents with symptoms affecting different sides of the body due to the decussation (i.e. crossing) of tracts at different levels.
- Ipsilateral weakness: the corticospinal tracts cross at the brainstem. Upper motor neuron signs below the lesion (i.e. high tone, hyperreflexia, weakness). There is usually flaccid paralysis (i.e. lower motor neuron weakness) at the level of the lesion
- Ipsilateral proprioception/vibration loss: the dorsal columns cross at the medulla
- Contralateral pain/temperature loss: cross at the level of the spinal cord
- Horner’s syndrome (Triad: miosis, ptosis, anhidrosis): if the lesion is above T1, hemisection of the cord affects the first order sympathetic neuron
Aetiology
Brown-Sequard syndrome is commonly due to trauma.
- Gun-shot wound
- Stabbings
- Road-traffic collision
Numerous non-traumatic causes may lead to Brown-Sequard syndrome such as disc disease, multiple sclerosis, or tumours.
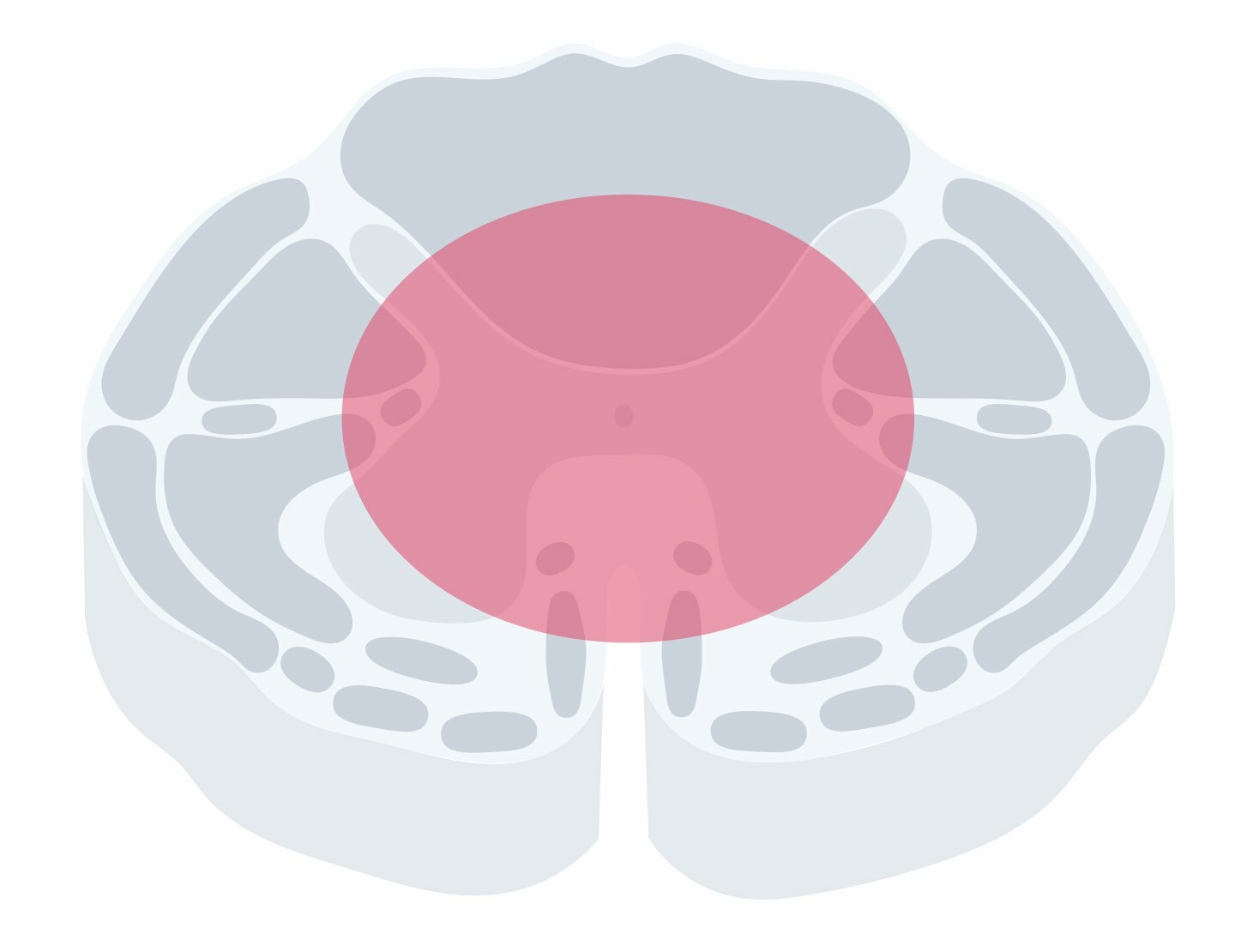
Central cord syndrome
A clinical syndrome commonly due to a hyperextension injury of the neck.
Central cord syndrome is a common spinal cord syndrome that is often the result of a traumatic hyperextension injury within the cervical spine. Weakness and sensory changes occur because it affects the medial aspect of the corticospinal tract and the crossing fibres of the spinothalamic tracts (crude touch, pain, temperature).
Clinical features
The syndrome is commonly due to pathologies within the cervical spine. It leads to a very classic set of clinical features.
- Weakness: upper extremity weakness > lower extremity weakness. Neurons to the upper extremities are more densely represented within the medial part of the lateral corticospinal tract
- Pain and temperature loss: usually located at the level of the lesion in a ‘cape-like’ distribution affecting the upper back and upper extremities. This is known as a ‘suspended sensory level’.
- Neck pain: commonly due to the mechanism of injury (hyperextension injury in trauma).
- Normal vibration and proprioception (dorsal columns unaffected)
- Urinary retention may occur
Aetiology
The most common cause is a hyperextension injury of the neck due to trauma. Hyperextension of the neck usually follows a fall in the elderly with simultaneous compression of the anterior and posterior cord (often in the context of coexistent cervical spine disease). This was originally thought to cause central haemorrhage and adjacent white matter compression but may instead be due to disruption of white matter axons.
Other classic causes of this syndrome include:
- Intramedullary tumor (i.e. tumours arising within the spinal cord)
- Syringomyelia: fluid-filled cyst within the spinal cord
Last updated: June 2022
Have comments about these notes? Leave us feedback
