Abdominal aortic aneurysm
Notes
Definition
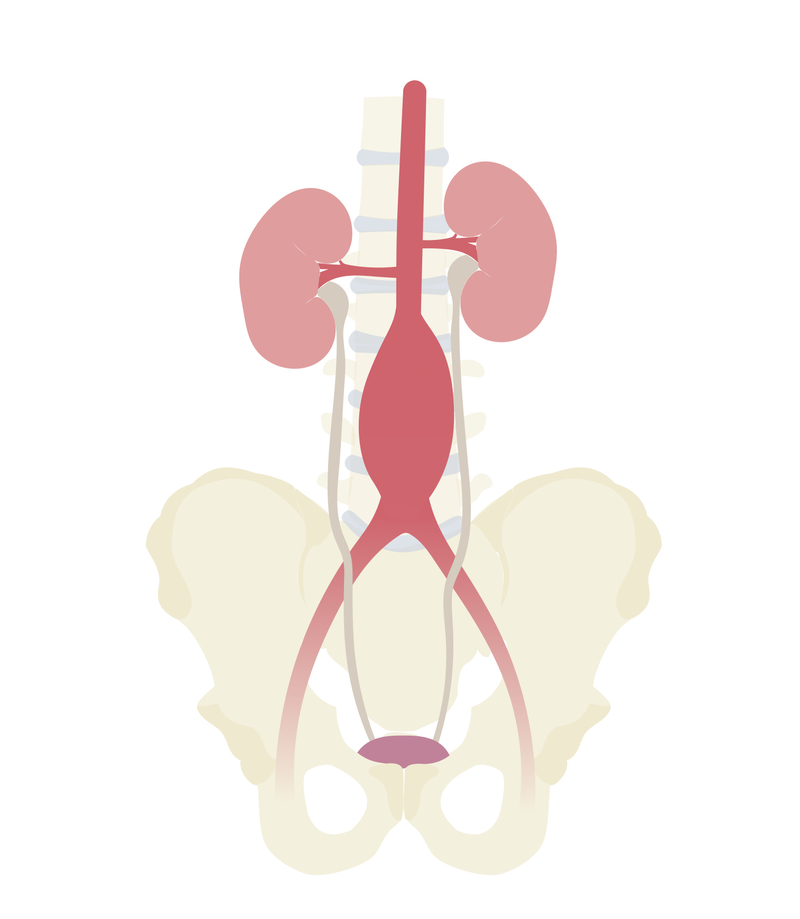
Abdominal aortic aneurysm (AAA) is defined as an abnormal dilatation of the abdominal aorta with a diameter greater than 3 cm.
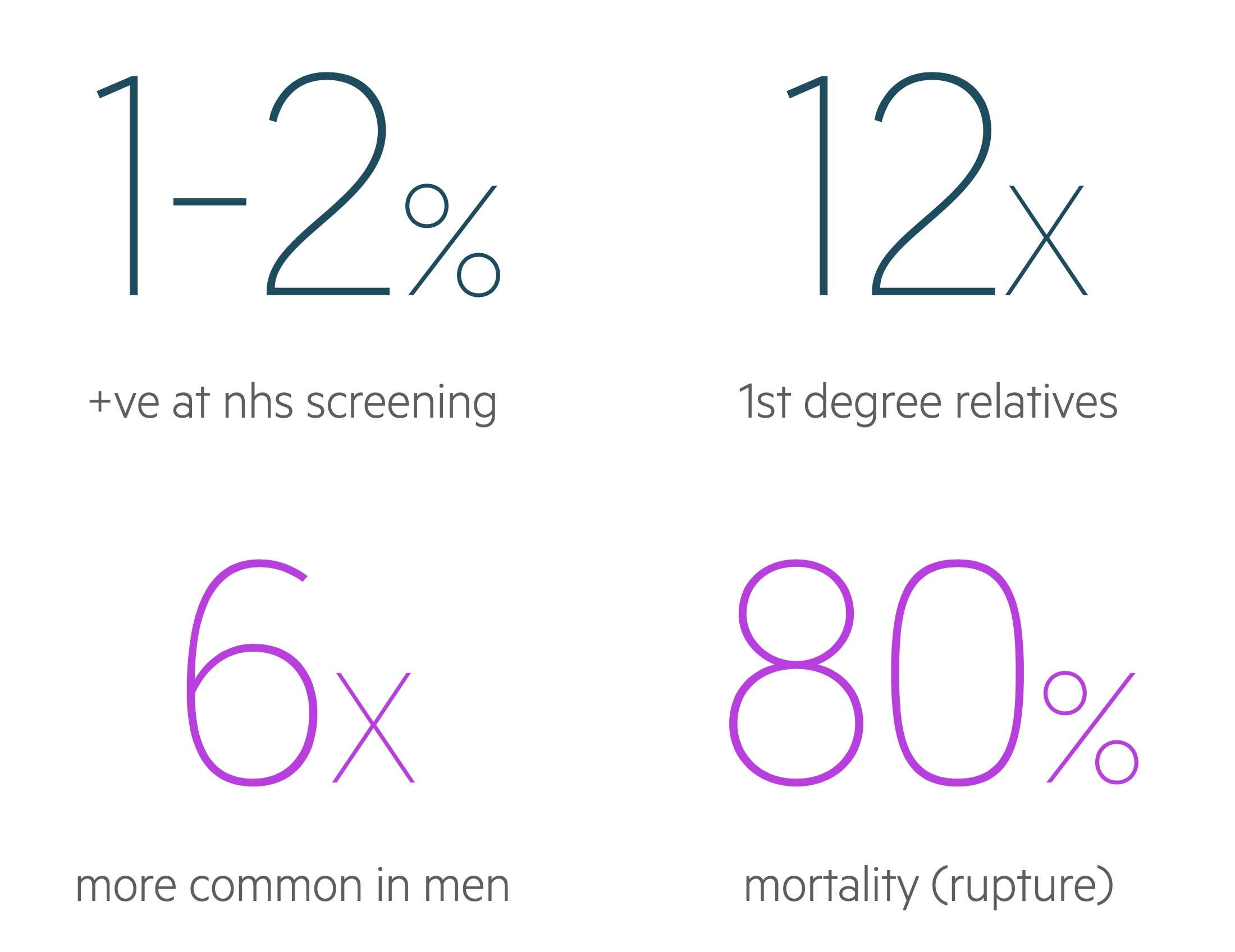
It is a relatively common aortic pathology that results in significant amounts of morbidity and mortality. Between 1-2% of men undergoing NHS screening (over the age of 65) will be found to have a AAA. The vast majority are infrarenal (i.e below the origin of the renal arteries).
Risk factors
AAA may be considered a degenerative condition of the aorta though its aetiology is not fully understood.
A number of risk factors have been shown to be associated with AAA:
- Age
- Male gender
- Atherosclerotic disease
- Family history
- Smoking
- Hypertension
- Connective tissue disorders
Uncommonly an aneurysm may be secondary to infection, inflammatory diseases or trauma.
Clinical features
AAA’s are frequently asymptomatic, the presence of symptoms often indicates rupture or impending rupture.
Unruptured AAA’s tend to be asymptomatic. Local mass effect may result in back pain or ureteric obstruction. AAA may be found incidentally on imaging or clinical examination. It may also present due to complications such as distal embolisation.
Ruptured AAA's frequently present with pain, the patient may also exhibit signs of haemodynamic compromise.
Symptoms
- Abdominal pain
- Back/loin pain
Signs
- Hypotension
- Tachycardia
- Collapse
- Pulsatile abdominal mass
Screening
The NHS has introduced screening for AAA for men aged 65 and over in England. It consists of an abdominal USS.
USS is a relatively cheap, non-invasive test with a high sensitivity for detecting AAA. Further management is dependent on the USS findings:
- < 3cm: No further follow-up required
- 3cm - 4.4cm: Found in just over 1%, advise yearly screening with USS, give lifestyle advice. Refer to vascular service, to be seen within 12 weeks.
- 4.5cm - 5.4cm: Found in around 0.5%, advise 3 monthly screening with USS, give lifestyle advice. Refer to vascular service, to be seen within 12 weeks.
- > 5.4cm: Found in around 0.1%, requires urgent two-week wait referral to vascular surgery to discuss management.
Screening is also indicated outside these groups if the patient is at greater risk of a AAA than the general population (e.g. family history). In the latest NICE guidance they advise considering USS in women over 70 (who have not already had abdominal imaging) with any one of; COPD, vascular disease, family history, hyperlipidaemia, hypertension, smoker/ex-smoker.
Investigations
AAA may be diagnosed with an abdominal USS or axial imaging.
Bedside
- Observations/Monitoring
- ECG
- Urine dip
Bloods
- FBC
- UE
- LFT
- Clotting screen
- ABG/VBG
- Group and Save / Crossmatch
Imaging
- AXR: Though not a sensitive test an AXR may be ordered in the work-up of a patient presenting with abdominal pain. May reveal a dilated aorta if aortic wall calcification is seen.
- Abdominal USS: A simple non-invasive test, standard modality readily available in emergency departments.
- MRI/CT: Used for pre-operatively in the elective setting to allow for surgical planning. May be used in the acute setting in suitably stable patients.
Elective management
Management of AAA depends on the patients presentation, co-morbidities and anatomical considerations.
Conservative
Patients with stable AAA not requiring surgical input should be advised to follow a healthy lifestyle and diet. They should be evaluated for hyperlipidaemia and hypertension and treated if necessary. Help with smoking cessation should be offered.
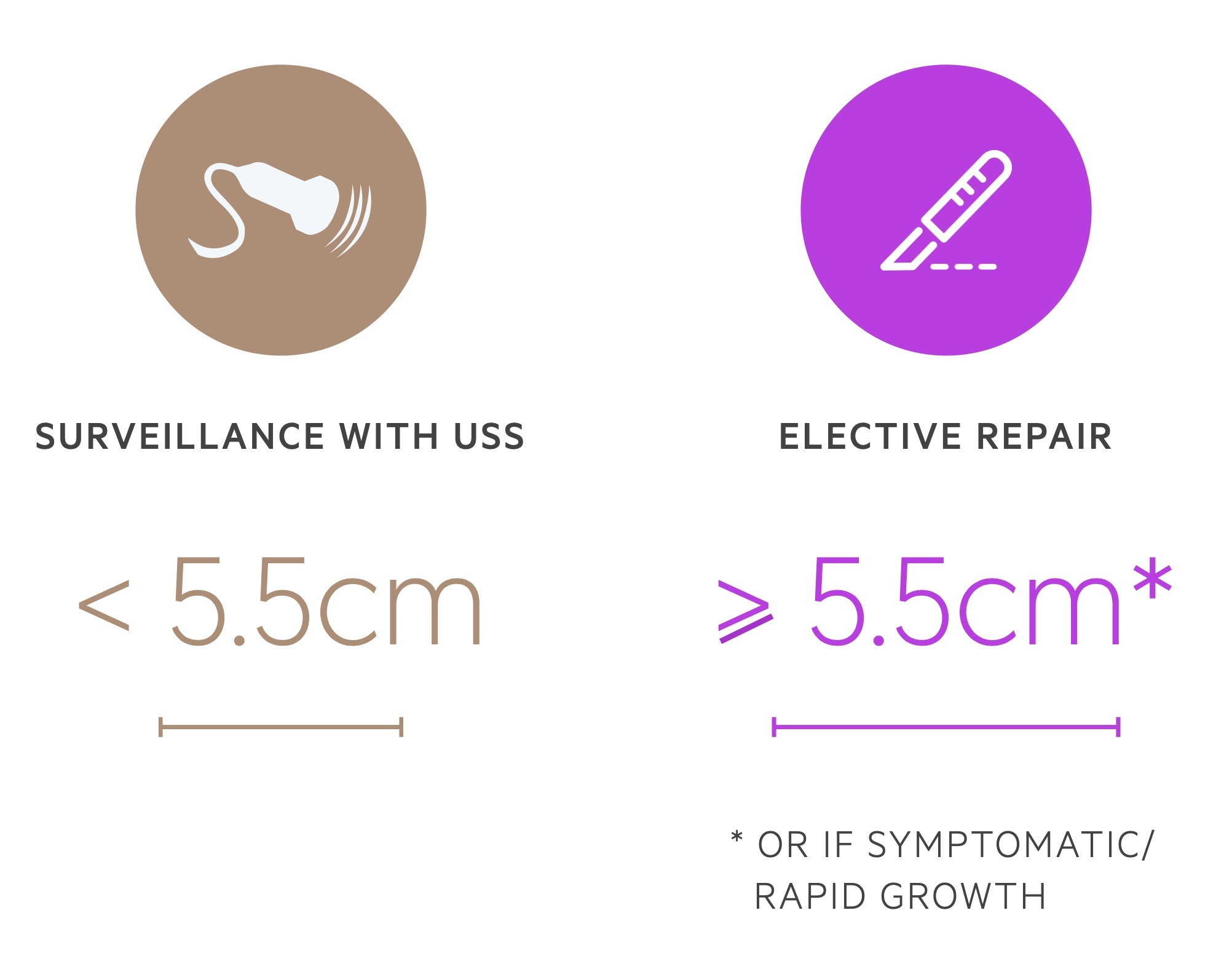
Their AAA should be monitored based on its diameter (see screening chapter above).
Surgical
Open surgical repair has long been the main-stay of management of patients with AAA. Elective surgery is indicated in:
- Diameter > 5.4cm
- Symptomatic aneurysms
- Asymptomatic, > 4cm and grown by more that one cm in a year.
Endovascular Aneurysm Repair
EVAR is a minimally invasive technique that utilises endovascular iliofemoral access to deploy an aortic graft. It may be used either in the elective or emergency setting.
The latest NICE guidance outlines when to consider EVAR - it is quite complex(!) and well worth a read if you are interested. We will summarise a number of the key points.
- Standard EVAR: EVAR may be considered in unruptured aneurysms who meet the same above criteria and abdominal copathology, anaesthetic risks or comorbidities that make open surgical repair less desirable. EVAR should only be used after a detailed explanation about the risks and uncertainties regarding EVARs outcomes.
- Complex EVAR: If open surgery and complex EVAR are both suitable, EVAR should only be used after a detailed explanation about the risks and uncertainties regarding EVARs outcomes.
NOTE: A standard EVAR is one that uses a standard infrarenal device, follows manufacturers guidance without any adjunctive procedures. Anything else is considered complex.
Emergency management
Acute rupture represents a medical emergency.
Fluid resuscitation / blood transfusion (BP targets vary, many advocate 100-120 systolic) and analgesia are key. Emergency surgery or EVAR may be indicated in suitable patients in acute rupture.
The management of a ruptured AAA is complex and dependent on numerous factors, we will broadly outline some of the options and considerations advised by NICE.
- Ruptured infrarenal AAA: EVAR appears to be the best option in women and men over the age of 70. Evidence indicates overall open repair may be better for men under 70.
- Standard EVAR unsuitable: Open surgical repair should be considered if standard EVAR is not possible.
- Complex EVAR: Should not be offered if open surgical repair suitable outside of trials.
Have comments about these notes? Leave us feedback