Tricuspid regurgitation
Notes
Overview
Tricuspid regurgitation (TR) is the most common right-sided heart valve disease.
In general, right-sided valvular disease is rare. Among the four valvular disorders, tricuspid regurgitation (TR) is the most common.
The underlying problem is backflow of blood from the right ventricle into the right atrium during systole. Although TR can be due to a problem with the tricuspid valve itself, it is most commonly caused by a problem elsewhere in the cardiovascular system, which has a knock-on effect on tricuspid valve function.
Management of patients with symptomatic TR usually involves treating the underlying cause +/- other medical treatments, with surgical intervention only being performed if a patient is undergoing cardiothoracic surgery for another reason.
Classification
Tricuspid regurgitation can be classified by underlying cause or severity.
Classification by Underlying Cause
Tricuspid regurgitation can be primary or secondary:
- Primary (problem with the tricuspid valve itself)
- Can be a problem with the valve leaflets or the valve cords.
- The result is that the valves do not close properly during systole.
- Primary TR is rarer, accounting for ~10% of cases.
- Secondary (problem elsewhere in the cardiac system)
- This other problem will have a knock-on effect on the tricuspid valve, preventing it from closing properly during systole.
- Secondary TR is more common, representing ~90% of cases.
We will look at specific examples of primary and secondary TR in ‘Aetiology and Pathophysiology’ below.
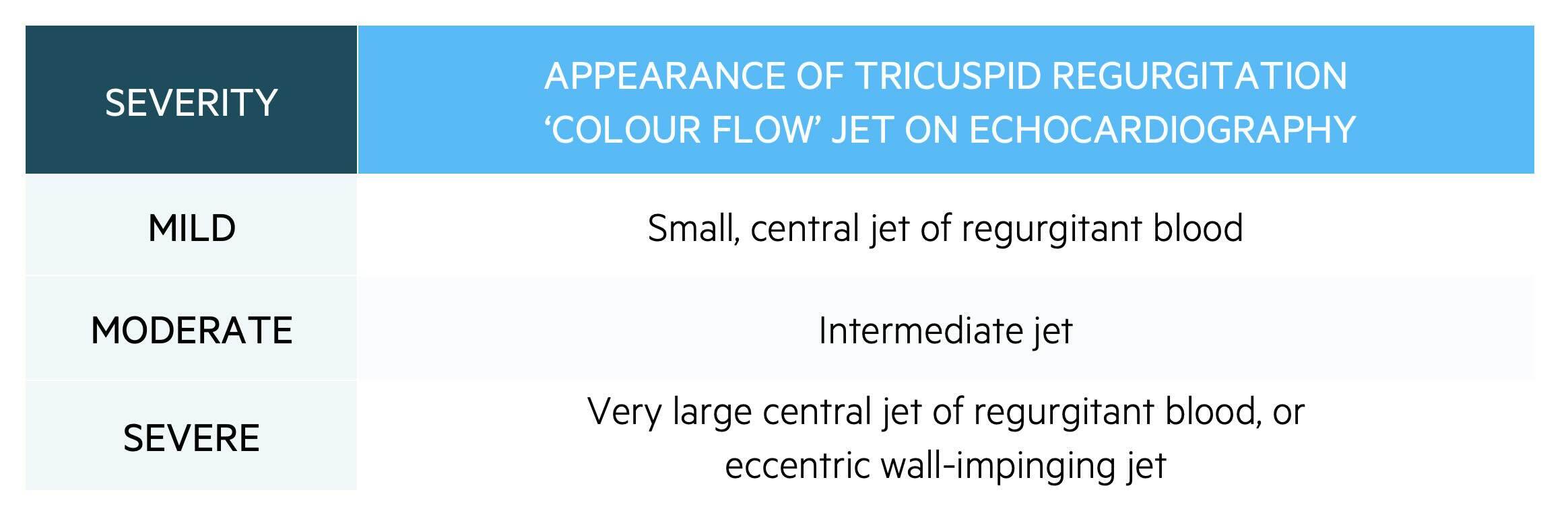
Classification by Severity
Tricuspid regurgitation can be graded as mild, moderate, or severe. The grading process uses multiple qualitative and quantitative measurements and is beyond the scope of a non-specialist. However, to give you a feel for grading severity, we have included one qualitative measurement of severity:
Epidemiology
Mild tricuspid regurgitation affects ~80% of healthy adults.
Mild TR is extremely common, affecting approximately 80% of healthy adults. It is so common that it can be considered normal. However, moderate-to-severe TR is less common, affecting 1 in 200 adult patients.
TR tends to affect older patients: 1 in 25 patients over the age of 75 has moderate or severe TR.
Aetiology
The aetiology of tricuspid regurgitation may be primary or secondary.
Primary causes of TR include:
- Congenital abnormality of valve leaflets (e.g. Ebstein abnormality).
- Infective endocarditis (intravenous drug users are at particular risk of TR secondary to endocarditis).
- Iatrogenic valve damage (e.g. caused by pacemaker leads).
Secondary causes of TR include:
- Right atrial dilation: this leads to dilation of the tricuspid valvular annulus and therefore interferes with valve closure.
- Right ventricular dilation (e.g. cardiomyopathy, ischaemic heart disease, pulmonary hypertension)
- Pulmonary hypertension: creates a back pressure against blood flow from the right ventricle into the pulmonary artery, therefore encouraging blood to regurgitate into the right atrium)
- Atrial fibrillation: can lead to tricuspid annular remodelling, independently of LV changes
Pathophysiology
The main underlying problem in tricuspid regurgitation is the backflow of blood from the right ventricle into the right atrium during systole.
There are three key pathological changes in TR:
- Rise in right atrial pressure: Initially, a small degree of TR doesn’t cause many problems. This is because the right atrium is relatively compliant (‘stretchy’), and so can cope with the increase in volume. However, as TR progresses, and more blood regurgitates with each heartbeat, right atrial pressure will start to rise.
- Back pressure in the vena cava: Increased right atrial pressure leads to back pressure into the SVC and IVC. This pressure causes the signs and symptoms of right-sided heart failure (e.g. raised JVP, peripheral oedema, ascites, liver impairment)
- Right ventricular dilatation: As TR becomes more severe, the right ventricle has to work harder. This is because it has to continue to pump blood into the pulmonary artery, whilst also pumping a significant volume of blood into the right atrium. Initially, the right ventricle copes with this by undergoing hypertrophy. However, eventually the right ventricle becomes unable to fully compensate for the regurgitation, leading to reduced forward flow into the pulmonary circulation and right ventricular dilatation.
Right ventricular dilatation is particularly problematic since – as we saw in secondary causes of TR above – right ventricular dilatation is also a cause of TR. This can lead to a vicious cycle of ventricular dilatation, valvular annular stretch and improper closing, increased work of the ventricle due to an ineffective tricuspid valve, which subsequently leads to more stretching, overload, and dilatation of the right ventricle.
Clinical features
The murmur of TR will be louder when more blood is crossing the valve.
History
The history is not particularly useful in diagnosing tricuspid regurgitation. This is because there aren’t many features in the history that specifically point to tricuspid regurgitation. In addition, many patients are asymptomatic for a long time and it may be an incidental finding on echocardiography completed for another reason. Finally, even patients with severe disease on echocardiogram may be asymptomatic.
In symptomatic patients, the following features might point to a diagnosis of tricuspid regurgitation:
- The sensation of pulsation in the neck (due to a raised JVP; see ‘examination’ below)
- Fatigue
- Dyspnoea
- Ankle swelling
- Painful hepatomegaly and/or splenomegaly
Examination
The examination is much more useful than the history for diagnosing tricuspid regurgitation and many subtle signs can be detected, particularly in severe disease with right heart failure.
- Raised JVP (may be prominent 'v' waves or giant 'cv' waves): reflecting transmission of ventricular contractions into the superior vena cava due to the incompetent tricuspid valve
- Parasternal heave: A heave is a palpable prolonged “lifting” of the chest wall with each heartbeat, which is commonly due to right ventricular hypertrophy
- Palpable thrill: A thrill is a palpable buzzing sensation caused by turbulent blood flow.
- Murmur: Tricuspid regurgitation causes a pansystolic (also described as a holosystolic) murmur. It is heard loudest in the tricuspid region i.e. 4th intercostal space, left sternal edge.
- Hepatomegaly
- Ascites
- Peripheral oedema
Auscultation manoeuvres
On examination, certain manoeuvres can be performed to accentuate the sound of the murmur and aid the diagnosis. The murmur of TR will be louder when more blood is crossing the valve. We can manipulate this fact using manoeuvres to increase the amount of blood crossing the valve. Manoeuvres increase venous return, which results in more blood crossing the valves on the right side of the heart.
Two manoeuvres are commonly used:
- Ask the patient to take a deep breath in, which expands the thorax and encourages venous return. The 'RILE' mnemonic (Right Inspiration, Left Expiration) can help you remember that right-sided murmurs are louder in inspiration.
- Lie the patient flat and perform a straight leg raise
Investigations and diagnosis
Echocardiography is the main diagnostic tool for tricuspid regurgitation.
Echocardiography is the principal investigation that can be used to both diagnose and grade tricuspid regurgitation. Patients may undergo other tests during their workup, such as chest x-ray and electrocardiogram (ECG). The following results on these tests might point towards TR:
- Chest x-ray (CXR):
- Cardiomegaly
- Right atrial enlargement
- ECG
- Right ventricular hypertrophy
- P pulmonale
Management
Unfortunately, severe TR is associated with a poor prognosis.
Asymptomatic Patients
Asymptomatic patients with moderate and severe disease should be followed up regularly. Follow-up should include:
- Assessment for any signs or symptoms of heart failure or valve disease.
- Echocardiography to look for right-ventricular changes (e.g. hypertrophy).
- Moderate TR: Echocardiogram every 1-2 years.
- Severe TR: Echocardiogram every 6-12 months.
Symptomatic Patients, and Patients with Right-Ventricular Changes
Management of symptomatic tricuspid regurgitation can be considered in three sections:
- Treat the Underlying Cause.
- Medical Treatment for Right-Sided Heart Failure.
- Surgical Treatment.
Treating the underlying cause involves correcting the underlying cause of secondary TR, which will slow or halt the disease. For example, treat pulmonary hypertension or atrial fibrillation. The main stay of treatment for the management of right-heart failure is diuresis with loop diuretics (e.g. furosemide). Finally, surgical treatment in general is not performed for TR. It tends to only be performed if a patient is undergoing cardiac surgery for another reason.
Regarding surgery, the NICE guidelines state:
- Consider surgical tricuspid valve repair at the time of mitral valve surgery when tricuspid regurgitation is moderate or severe.
- Consider surgical tricuspid valve repair at the time of aortic valve surgery when tricuspid regurgitation is severe.
Last updated: September 2024
References:
-
UpToDate. Etiology, clinical features, and evaluation of tricuspid regurgitation.
-
Arsalan, M. et al. Tricuspid regurgitation diagnosis and treatment, European Heart Journal, Volume 38, Issue 9, 1 March 2017, Pages 634–638, https://doi.org/10.1093/eurheartj/ehv487
-
Zaidi, A. et al. Echocardiographic assessment of the tricuspid and pulmonary valves: a practical guideline from the British Society of Echocardiography. Echo Res Pract 7, G95–G122 (2020). https://doi.org/10.1530/ERP-20-0033
-
Adamo, M. et al. Epidemiology, pathophysiology, diagnosis and management of chronic right-sided heart failure and tricuspid regurgitation. A clinical consensus statement of the Heart Failure Association (HFA) and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) of the ESC. Eur J Heart Fail. 2024. 26: 18-33. https://doi.org/10.1002/ejhf.3106
-
NICE guideline [NG208]. Heart valve disease presenting in adults: investigation and management. 17 November 2021.
-
Deranged Physiology; Yartsev, A. Tricuspid Regurgitation.
Have comments about these notes? Leave us feedback
