Third nerve palsy
Notes
Introduction
A third nerve palsy refers to damage to the oculomotor cranial nerve.
The oculomotor nerve is the third cranial nerve that has predominant motor function to the pupil, eyelid and extraocular muscles. Paralysis or ‘palsy’ to the oculomotor nerve can occur anywhere along its course from nucleus in the midbrain to orbital apex.
Anatomy & physiology
The third nerve nucleus originates in the midbrain of the brainstem.
Nerve course
The third nerve nucleus is comprised of several subnuclei that innervate important visual structures.
Fibres from these nuclei pass from the midbrain into the subarachnoid space and then into the lateral wall of the cavernous sinus. It then enters the superior orbital fissure and divides into superior and inferior branches.
- Superior branch: innervates levator palpebrae and superior rectus
- Inferior branch: Innervates medial and inferior rectus muscles, inferior oblique, and pupillary sphincter
Function
The third cranial nerve has a small number of sensory fibres, but is predominantly a motor nerve that innervates ocular structures.
- Pupil: parasympathetic fibres run superficially within the nerve to cause pupil constriction
- Eyelid: innervates the levator palpebrae superioris that elevates the eyelid
- Extraocular muscles: innervates all the extraocular muscles except the superior oblique and lateral rectus muscle
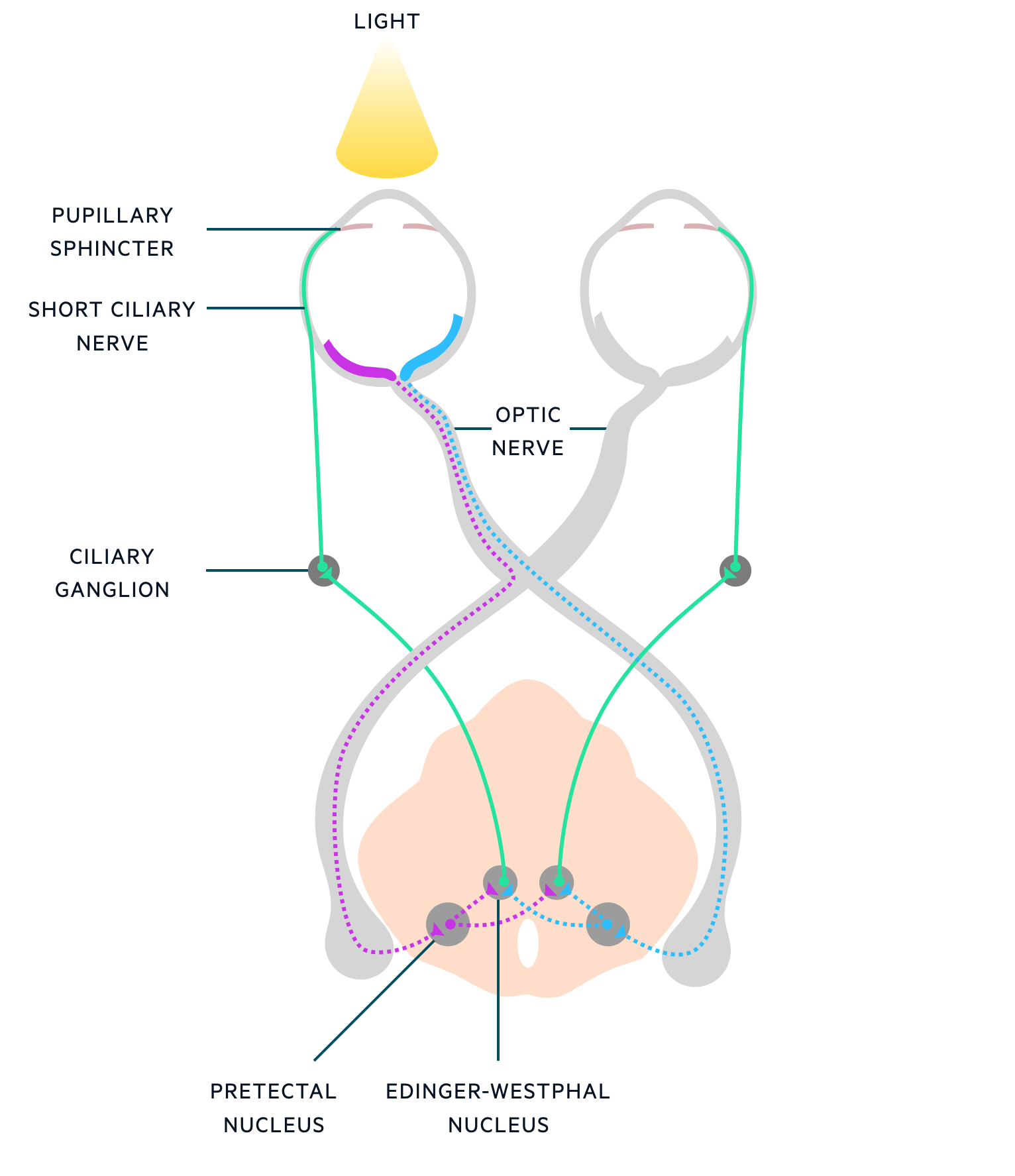
Pupillary light reflex
The third nerve has an important role in the pupillary light reflex.
The pupillary light reflex controls the diameter of the pupil in response to light. It is mediated by the parasympathetic nervous system and involves the optic and oculomotor cranial nerves.
The basic principle of the parasympathetic pathway is that as light is shone onto one eye there is corresponding equal and symmetrical pupillary constriction. This occurs by contraction of circular fibres of the iris (i.e. pupillary sphincter).
Pupillary light reflex stages
- Light source: Light is shone onto the retina and detected by photoreceptors
- Transmitted via optic nerve: Retinal fibres transmit this signal via the optic nerve. Nasal retinal fibres cross at the optic chiasm and enter the contralateral pretectal nucleus. Temporal retinal fibres do not cross and enter the ipsilateral pretectal nucleus.
- Pre-tectal nucleus to Edinger-Westphal nuclei: Input from the pretectal nucleus is transmitted the Edinger-Westphal (EW) nuclei (a subnuclei of the oculomotor nerve). The ipsilateral pretectal nucleus transmits information to both the ipsilateral and contralateral EW nuclei.
- Transmitted to ciliary ganglion: Effector neurons pass from both EW nuclei to the ipsilateral ciliary ganglion. From here, fibres pass via the short ciliary nerve to the ipsilateral pupillary sphincter.
- Pupillary constriction: once activated, each pupillary sphincter contracts leading to symmetrical pupillary constriction
Aetiology & pathophysiology
A lesion at any point during the course of the third nerve can cause palsy.
A variety of pathologies can lead to a third nerve palsy. These are generally divided according to location. Each location has several possible causes and associated clinical manifestations.
Locations:
- Midbrain
- Subarachnoid space
- Cavernous sinus
- Orbital apex
Midbrain
The oculomotor nucleus is situated in the brainstem. It is at risk of damage from a tumour, haemorrhage or ischaemia (i.e. stroke). Midbrain lesions are usually associated with other neurological feature and may be part of a wider ‘brainstem syndrome’. For example, Weber’s syndrome is characterised by ipsilateral third nerve palsy and contralateral hemiparesis.
Subarachnoid space
Damage to the oculomotor nerve in the subarachnoid space typically causes an isolated third nerve palsy (absence of other neurological features). A variety of conditions can cause a third nerve palsy in this location:
- Inflammation/infection (e.g. meningitis)
- Malignancy (e.g. meningeal metastasis, also known as meningeal carcinomatosis)
- Ischaemia (e.g. diabetes mellitus, giant cell arteritis): thought to be a microvascular event.
- Aneurysm
- Trauma
The major concern of a new-onset third nerve palsy is a rapidly enlarging cerebral aneurysm leading to compression. These aneurysms are thought to have an imminent risk of rupture. Commonly due to a posterior community artery aneurysm.
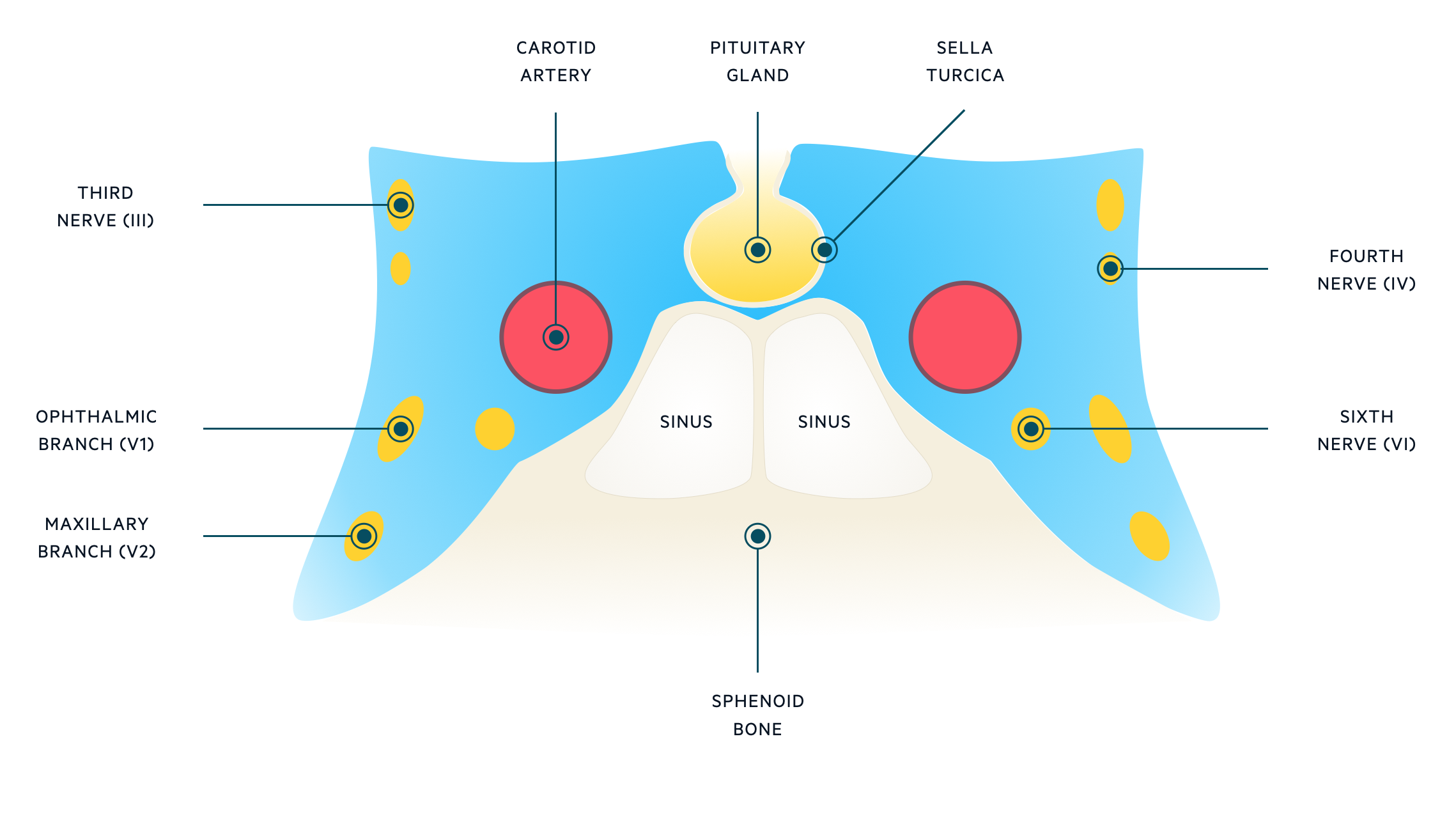
Cavernous sinus
The cavernous sinus is one of the dural venous sinuses within the head. It is essentially a cavity bordered by the temporal bone, sphenoid bone and sella turcica, which contains the pituitary gland.
Several important structures run through or adjacent to the cavernous sinus including cranial nerves III, IV, VI, V1, V2 and the carotid artery. Therefore, a third nerve palsy secondary to a cavernous sinus lesion is usually associated with other nerve palsies. Typical causes at this location include thrombosis, tumour or carotid artery aneurysm.
Orbital apex syndrome
Lesions at the orbital apex are associated with other neurological features (e.g. multiple cranial nerve palsies) and ophthalmic signs including chemosis (swelling of the conjunctiva) and proptosis.
Orbital apex syndrome describes the presence of multiple cranial nerve palsies (III, IV, VI, V1) and optic nerve dysfunction due to various pathologies including head and neck tumours, invasive fungal sinusitis, orbital cellulitis or sarcoidosis among many others. Multiple cranial nerve palsies (III, IV, VI, V1) in the absence of optic nerve dysfunction may suggest superior orbital fissure syndrome (these nerves traverse the superior orbital fissure) or cavernous sinus lesions.
Isolated versus non-isolated
A third nerve palsy may occur in isolation or alongside other neurological features. An isolated third nerve palsy usually locates to the subarachnoid space. A new isolated third nerve palsy is concerning for an enlarging aneurysm with risk of rupture and requires urgent assessment.
Pupil-sparing versus pupil involved
Absence or presence of pupil involvement is used to help determine the possible aetiology. This is because of the anatomical location of the parasympathetic fibres within the oculomotor nerve.
Parasympathetic motor fibres associated with the pupillary light reflex are situated superficially within the oculomotor nerve. Therefore, compressive lesions (e.g. aneurysms) will affect outer fibres leading to pupillary dilatation and loss of the light reflex (i.e. the pupil is fixed and dilated). On the other hand, vascular lesions (e.g. ischaemia, diabetes mellitus) tend to affect the inner fibres preferentially. This 'spares' the superficial parasympathetic fibres leading to pupillary sparing.
Clinical features
A third nerve palsy is characterised by ipsilateral ptosis with a ‘down and out’ eye appearance.
A third nerve palsy usually presents with sudden onset diplopia (double vision) and noticing ptosis (drooping eyelid). Other neurological features are dependent on the underlying aetiology.
Symptoms
- Diplopia
- Ptosis (drooping eyelid)
- Pain
- Severe headache (concerning for aneurysmal subarachnoid haemorrhage)
- Meningism (headache, neck stiffness, photophobia): suggestive of subarachnoid haemorrhage or meningitis
Signs
- Ptosis
- Eye appearance: ‘down and out’
- Pupil dilatation (mydriasis): unless pupillary sparing
- Loss of light reflex: unless pupillary sparing
- Neck stiffness: suggestive of subarachnoid haemorrhage or meningitis
- Focal neurological deficits: particularly if brainstem lesions
- Other cranial nerve palsies (IV, VI, V1): particularly if cavernous sinus or orbital apex lesions
Diagnosis & investigations
A third nerve palsy is a clinical diagnosis.
The diagnosis of a third nerve palsy is made clinically based on characteristic features (e.g. ptosis, ‘down and out’ eye appearance, diplopia). Once identified, it warrants further evaluation for the underlying cause.
Investigations depend in the suspected aetiology with the most concerning being an aneurysmal subarachnoid haemorrhage (or impending haemorrhage). Key investigations including neuroimaging (CT/MRI) and lumbar puncture (if required). Some clinicians and guidelines will recommend neuroimaging for all new third nerve palsies.
Aneurysm suspected
If the patient has presented with a new-onset third nerve palsy and a cerebral aneurysm is suspected, they need an urgent work-up similar to the evaluation of a subarachnoid haemorrhage. This includes a CT head looking for evidence of blood in the subarachnoid space and a CT angiography looking at the intracranial vessels for a possible aneurysm. If a ruptured aneurysm is suspected with a normal CT head, then patients require a lumbar puncture looking for Xanthochromia.
For more information see Subarachnoid haemorrhage notes
Management
The treatment of a third nerve palsy is directed towards the underlying cause.
The majority of third nerve palsies will resolve over weeks to months, particularly if the underlying cause is addressed. Ischaemic third nerve palsies (e.g. secondary to diabetes) usually have favourable outcome with resolution over 3-6 months. Antiplatelet therapy should be considered.
For persistent deficits an eye patch may be required to prevent diplopia short-term. Longer term options can include prisms and strabismus (abnormal eye alignment) surgery. Patients should be referred to an ophthalmologist.
Last updated: July 2021
Have comments about these notes? Leave us feedback
