Specific phobia
Notes
Introduction
In phobias, the fear response is excessive, irrational, and can have debilitating consequences for individuals.
Fear is an uncomfortable emotion that occurs in response to threatening situations. The purpose of fear is to motivate an individual to protect themselves and avoid harm. Fear is therefore a rational reaction to a real threat or danger.
In phobias, the fear response is excessive, irrational, and can have debilitating consequences for the individual. There is an exaggerated or unrealistic sense of danger about the phobic situation or object, which persists despite evidence to the contrary. In some cases, even thinking about the phobic object can cause anticipatory anxiety. Negative reactions to phobic stimuli include feelings of disgust or revulsion and panic-like physical symptoms including lightheadedness, fainting, tremor, shortness of breath, palpitations, sweating, and nausea. The phobic object or situation is actively avoided or else endured with intense fear or anxiety.
Phobias can be divided into specific/simple phobias and complex phobias:
- Specific or simple phobia: fear of a specific object or situation. Common examples include animals (e.g. spider, insects, dogs), natural environment (e.g. heights, storms, water), blood-injection-injury (e.g. needles, invasive medical procedures), and situational (e.g. aeroplanes, elevators, enclosed places).
- Complex phobia: these tend to have a more disruptive impact on an individual’s life. The most common complex phobias are agoraphobia and social phobia.
Epidemiology
Specific phobias usually begin in childhood and can persist throughout an individual’s life.
The lifetime prevalence of specific phobias ranges from 3 to 15%. The most commonly reported specific phobias are those of heights and animals. Although specific phobias have a high prevalence, a low proportion of those affected seek treatment.
Aetiology & risk factors
The aetiology of most anxiety disorders is thought to be a complex interaction between environmental factors, genetic factors, and psychological traits of an individual.
Phobias have a boundary with normality, as some fears can be a normal part of development (for example, fear of the dark in children) that lessen with time.
Anxiety disorders tend to run in families, but it isn’t clear how much of this is related to genetics versus learned behaviour. Phobias may be learned from having observed a parent or caregiver react with disproportionate and irrational fear to the phobic object.
The individual may have had a previous direct negative experience with the phobic object that led to the development of excessive fear. For example, a dog may act aggressively toward a child, which leads the child to associate all dogs with danger and experience a disproportionate overwhelming fear response to all dogs.
Clinical features & diagnosis
Both DSM-V and ICD-11 can be used as frameworks to aid the clinical diagnosis of specific phobias.
Below we outline the diagnostic criteria for specific phobia using the DSM-V:
Specific phobia is characterised by a marked fear or anxiety of a specific object or situation.
The fear or anxiety is:
- Almost always provoked by the phobic object or situation.
- Disproportionate to the actual threat posed by phobic object or situation.
The phobic object or situation is:
- Actively avoided OR,
- Endured with intense fear or anxiety.
The fear, anxiety, or avoidance behaviours are:
- Persistent, lasting for >6 months.
- Cause the individual significant distress or functional impairment (social, occupational, or other important aspects of functioning).
- Not better explained by another mental disorder (see differential diagnoses below).
The DSM-V includes specifiers for the phobic stimulus which include:
- Animal (e.g. spider, insects, dogs)
- Natural environment (e.g. heights, storms, water)
- Blood-injection-injury (e.g. needles, invasive medical procedures)
- Situational (e.g. aeroplanes, elevators, enclosed places)
Differential diagnosis
The main differential diagnosis of a specific phobia is a more generalised, or complex, anxiety disorder.
- Generalised anxiety disorder: excessive anxiety about several events and activities, not limited to specific phobic objects or situations.
- Social anxiety disorder: this is a complex phobia with fear and avoidance of social situations.
- Agoraphobia: this is a complex phobia with fear and avoidance of more than one situation where escape might be difficult or help unavailable.
- Panic disorder: Exposure to a specific phobia may produce panic-like symptoms. In panic disorder, panic attacks are unexpected with no clear trigger.
- Obsessive-compulsive disorder (OCD): in OCD, the disproportionate anxiety and avoidance behaviours are related to obsessions and associated compulsions rather than fear of a specific object or situation.
Management
One of the main management strategies for a specific phobia is cognitive behavioural therapy (CBT).
Cognitive Behavioural Therapy (CBT) focuses on the link between our thoughts, behaviours, and emotions. Challenging negative thoughts and changing unhelpful behaviours can have a positive impact on how a person feels.
The cognitive component of CBT for specific phobias might involve challenging negative automatic thoughts, beliefs or expectations related to the phobic object or situation. For example, when considering a spider phobia, an individual may have the negative thought that “the spider will bite me.” This negative thought can be challenged by thinking of evidence to disprove it and therefore rationalise the fear somewhat.
The behavioural component of CBT for a specific phobia involves exposure therapy – the individual is supported to gradually expose themselves to the phobic object or situation that is feared and usually avoided. This is called systematic desensitisation which is a commonly used CBT method for the treatment of phobias. It involves working with a therapist to construct an anxiety “hierarchy” that ranks situations that cause anxiety from the least to the most anxiety-inducing.
Please see the example anxiety hierarchy for a specific phobia of a spider:
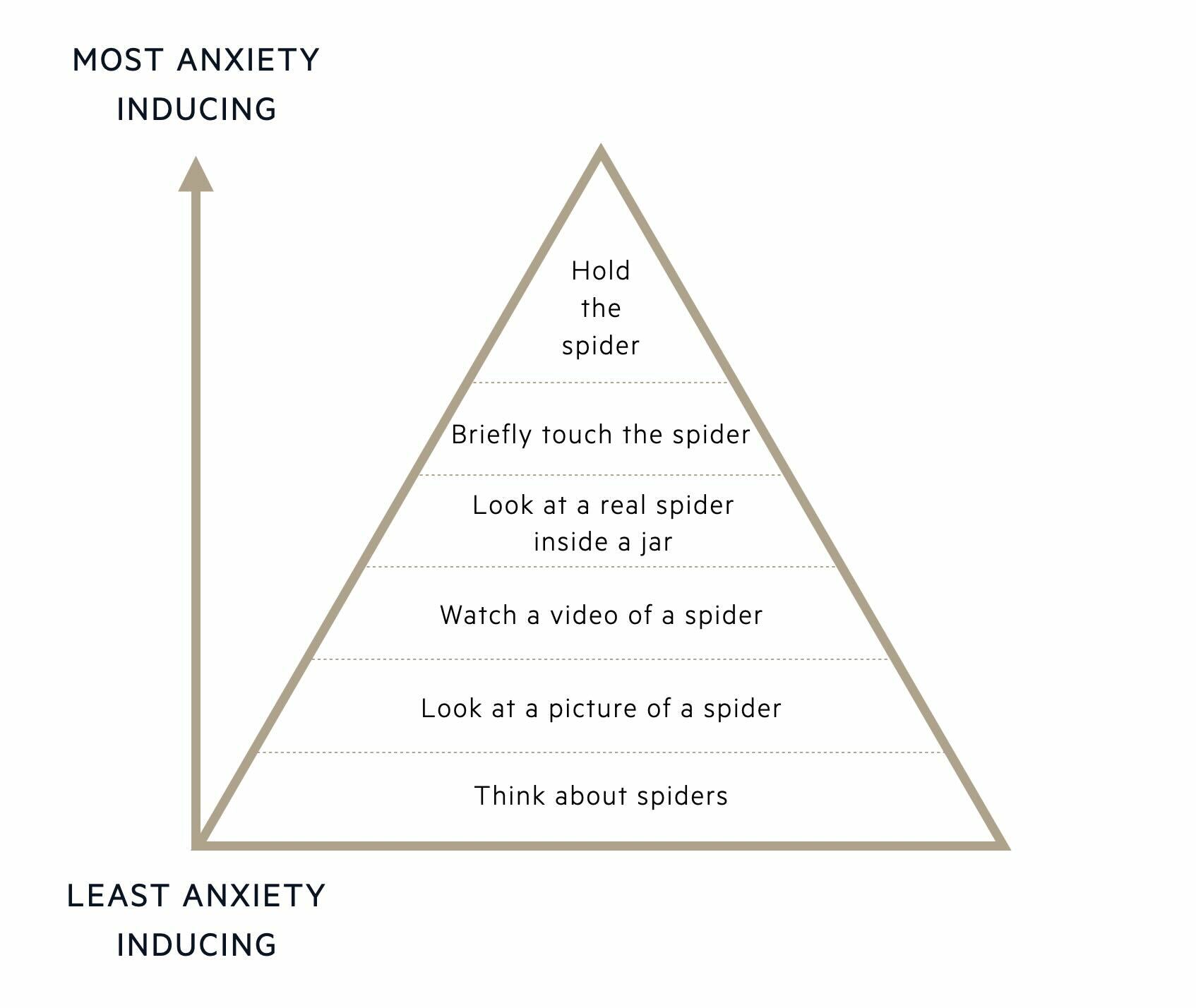
The individual will be supported by the therapist to gradually work their way up the anxiety hierarchy, starting by exposing themselves to objects/situations that cause the least anxiety and finishing with exposure to the most anxiety-inducing object/situation. The therapist also teaches the individual relaxation techniques to help manage anxiety at each stage of the hierarchy. By gradually exposing themselves to more stressful situations, using relaxation techniques and tolerating the anxiety, the fear response should reduce over time. The aim is to reduce the fear response to the phobic object/situation and replace this with a relaxation response.
Applied relaxation
In applied relaxation, the therapist first works with the individual to help them spot the signs of tension. They then teach the individual exercises to relax muscles and relieve tension. These relaxation techniques are usually practiced in the absence of the phobia in low-stress environments before being used to prevent and manage anxiety/panic on exposure to the phobic object/situation.
Last updated: January 2024
References:
DSM-V
Treatment - Phobias - NHS (www.nhs.uk)
NHS England. (2016). Adult Psychiatric Morbidity Survey: Survey of Mental Health and Wellbeing, England.
Have comments about these notes? Leave us feedback
