Hip fractures
Notes
Introduction
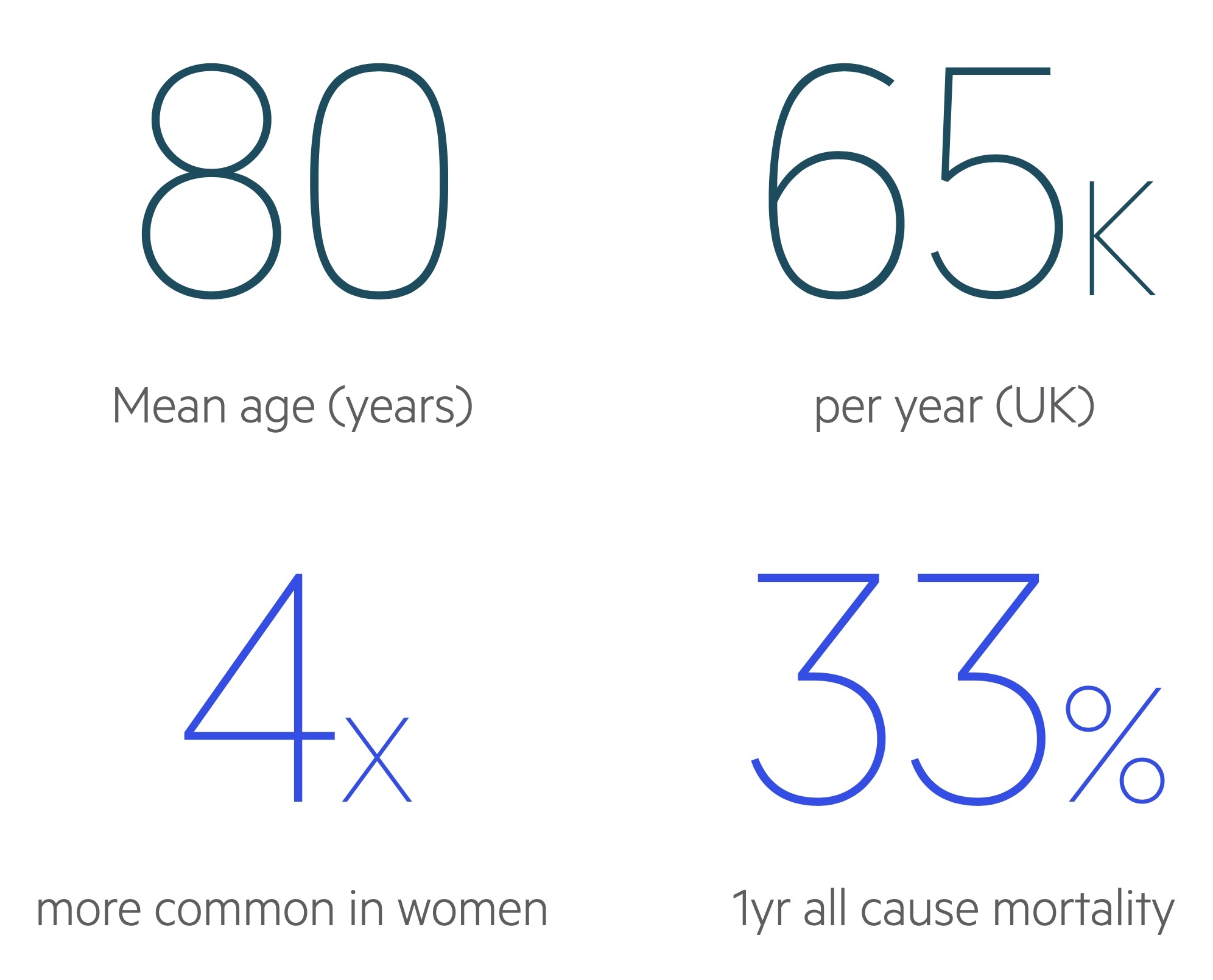
A hip fracture is a bony injury of the proximal femur typically occurring in the elderly.
Older patients are more likely to have gait unsteadiness and reduced bone mineral density, predisposing to fracture.
It is a common serious injury in older people, costing the NHS and social care £1 billion per year.
Basic anatomy
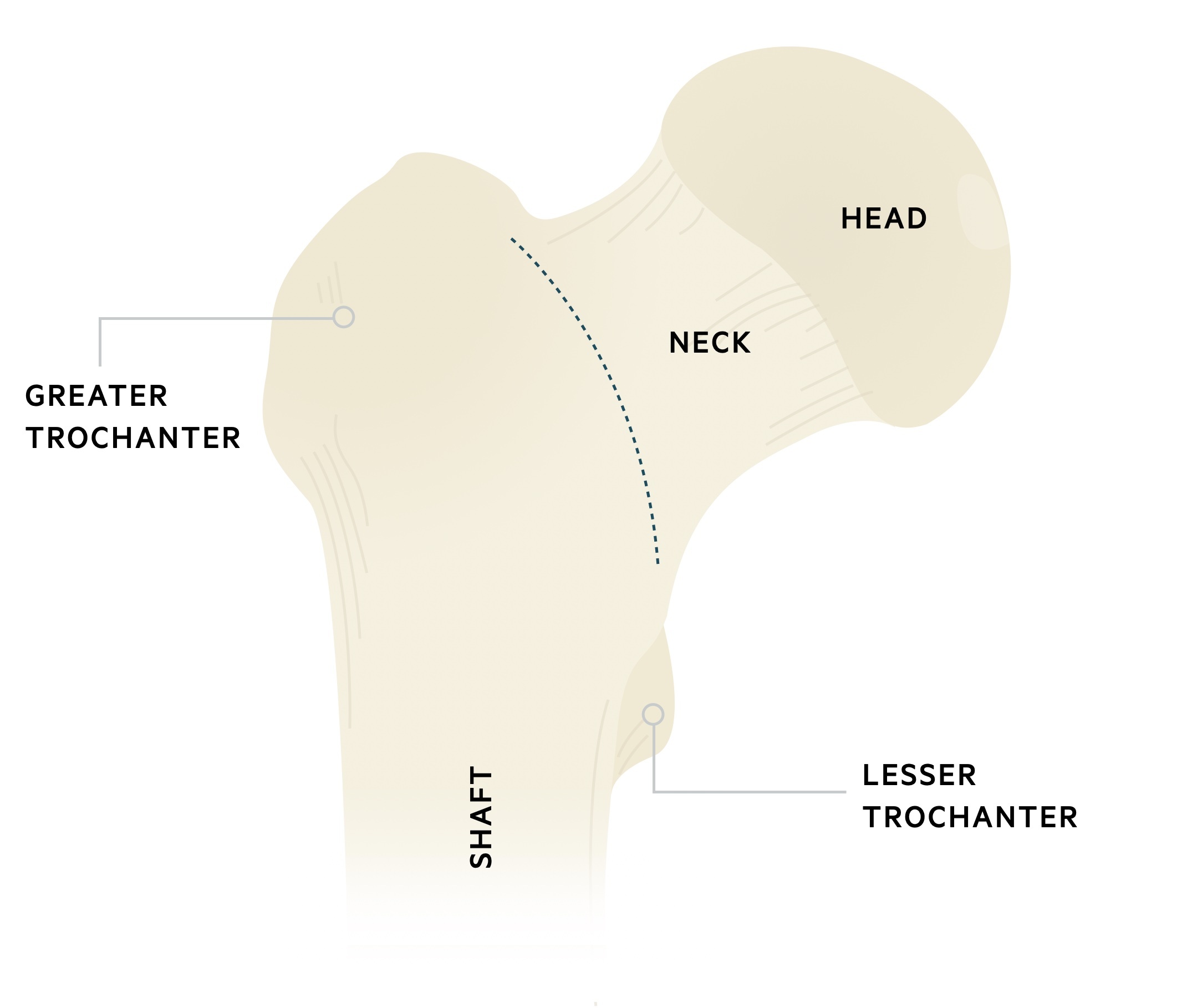
The proximal femur consists of a head, neck, trochanters (greater and lesser) & shaft. It is the largest bone in the human body.
The inter-trochanteric line lies on the anterior surface of the femoral neck, running between the trochanters. It demarcates the inferior attachments of the hip capsule.
Hip capsule
The capsule of the hip is attached proximally to margins of acetabulum and transverse acetabular ligament. Distally, to the inter-trochanteric line, bases of greater & lesser trochanters and to the femoral neck posteriorly (approx. 1/2 inch from the trochanteric crest). It contains the retinacular vessels - a major component of the blood supply to the femoral head.
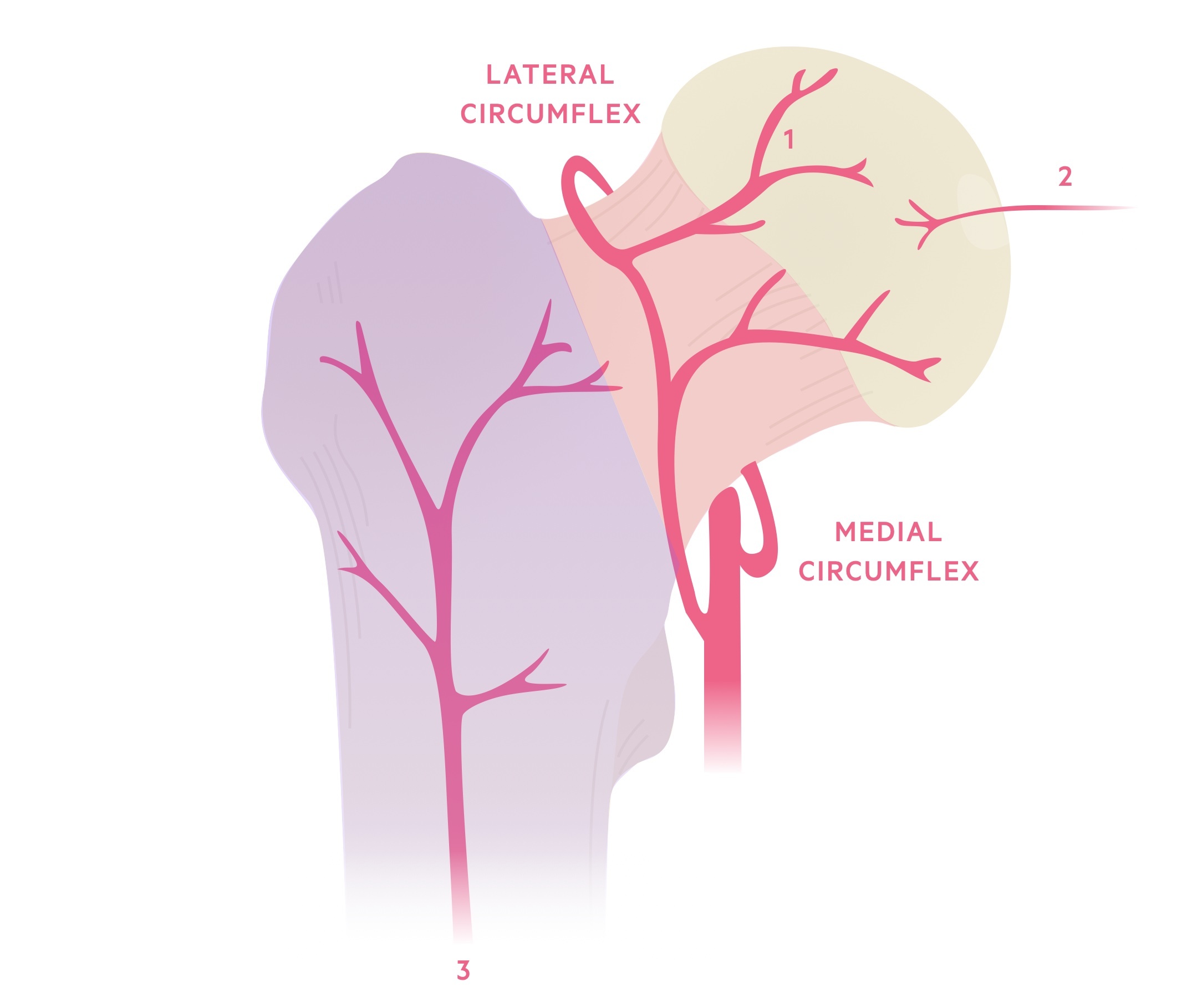
Blood supply to the femoral head
The femoral head receives blood from three sources:
- Retinacular vessels - main blood supply. Originates from an extra-capsular arterial ring, supplied by medial and lateral circumflex vessels (profunda femoris A.). Reinforced by the superior and inferior gluteal arteries (internal iliac A.).
- Foveal artery - not a major source. During skeletal development, supplies the epiphysis with a small amount of blood. Said to become obliterated in adult life (ligamentum teres).
- Metaphyseal vessels - not a major source. After skeletal maturity, metaphysical arteries also contribute blood to the femoral head.
Classification
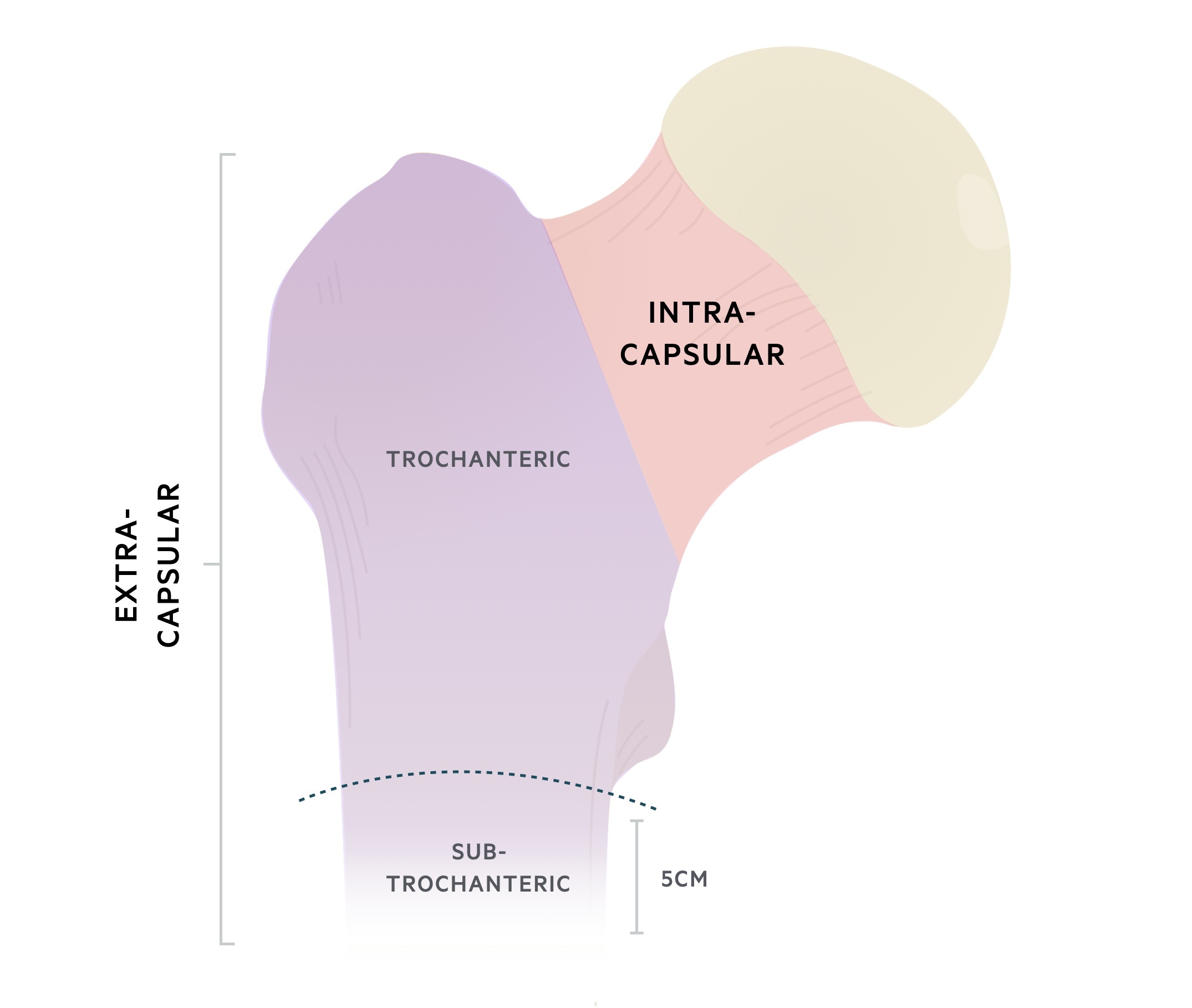
Hip fractures may be categorised as either intra- or extra-capsular, depending on their location in relation to the inter-trochanteric line.
- Above = intra-capsular
- Below = extra-capsular
The type of fracture determines the likelihood of disruption to the blood supply of the femoral head. Broadly speaking, intra-capsular fractures are associated with a higher-risk of disruption, owing to the close proximity of the retinacular vessels.
Garden's classification (intra-capsular fractures)
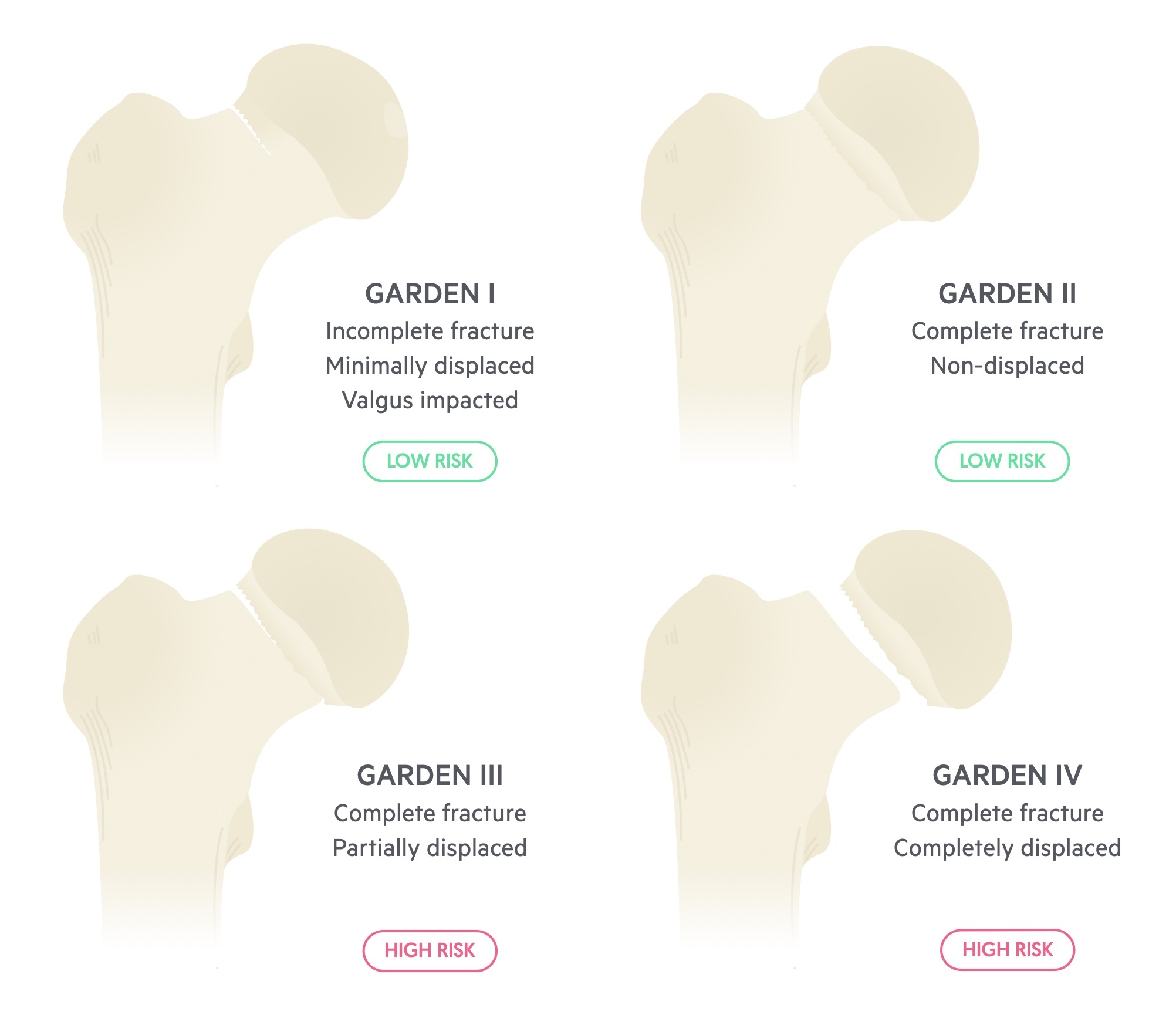
Intra-capsular fractures are further sub-classified according to Garden’s classification.
There are four types.
- Type I - Incomplete, impacted in valgus
- Type II - Complete, undisplaced
- Type III - Complete, partially displaced
- Type IV - Complete, completely displaced
With type 1 & 2 there is minimal displacement, and therefore a lessened risk of disruption to the femoral head blood supply. Conversely, with type 3 & 4, where there is much greater displacement, there is substantially higher risk.
Classification is based on the integrity of the trabecular lines in an AP projection. It is used to guide management.
Risk factors
A number of risk factors pre-dispose patients to hip fractures.
- Increasing age
- Osteoporosis
- Low muscle mass
- Steroids
- Smoking
- Excess alcohol intake
- Metastatic spread of cancer to bone
Aetiology
In the elderly, hip fractures are normally caused by falls.
The mechanism varies from direct falls onto the affected hip, to twisting, in which the patient’s foot is planted and the body rotates. Bones are typically osteopaenic (reduced bone density) and also deficient in elastic reserve (i.e. they are very brittle).
In younger patients, hip fractures are more commonly the result of major trauma (e.g. motor vehicle accidents), or in patients with gait disturbance (e.g. in multiple sclerosis) in which they are at increased risk of falls. Certain medications, such a prolonged corticosteroid use, can also predispose to osteopaenia.
Clinical features
Hip fractures are diagnosed radiologically, but may be suspected clinically.
Patients usually describe a fall or recent trauma; it is unusual for fractures to occur with no precipitating trauma. High-energy trauma (e.g. motor vehicle accident) is more common in younger patients, although accounts for only a small percentage (2-3%) of all hip fractures.
It is important to elucidate why an individual may have fallen; whether the fall was mechanical in nature (e.g. slipped on a wet floor) or if the event was precipitated (e.g. MI, stroke, chest infection, UTI etc.)
Patients typically report an inability to bear weight and pain in the affected side, with a reduced range of movement.
Symptoms
- Hip / knee pain
- Inability to bear weight
- Limited range of motion
Signs
- Bony tenderness over affected hip
- Shortened / externally rotated leg (only present if significant displacement)
Investigations
A hip fracture is a radiological diagnosis, although additional investigations can be used to aid the diagnosis and look for complicating pathology.
Bedside
- Observations
- Urine dip
- ECG
Bloods
- FBC
- U&E
- CRP
- Clotting
- Group & Save x 2
- Bone profile
- Vitamin D
Imaging
- CXR: required pre-operatively.
- Plain films: XR pelvis, AP and lateral of affected hip. Full length views of the femur may be obtained, particularly if metastatic disease in the bone is suspected.
- MRI/CT: if plain films are inconclusive, to rule out occult fracture. MRI is gold-standard, CTs are generally more readily availible.
- Cardiac echo: if new murmur is auscultated, abnormal ECG, or significant cardiac history. Often requested by the anaesthetist pre-operatively.
X-ray interpretation
X-rays are the first-line imaging investigation - fractures may be obvious, subtle or occult.
X-rays should be carefully reviewed using the clinical presentation to provide context. The typical series will include an AP pelvis, AP view of the affected hip and lateral view of the affected hip. The cortical lining of the bone should be examined for any breaks.
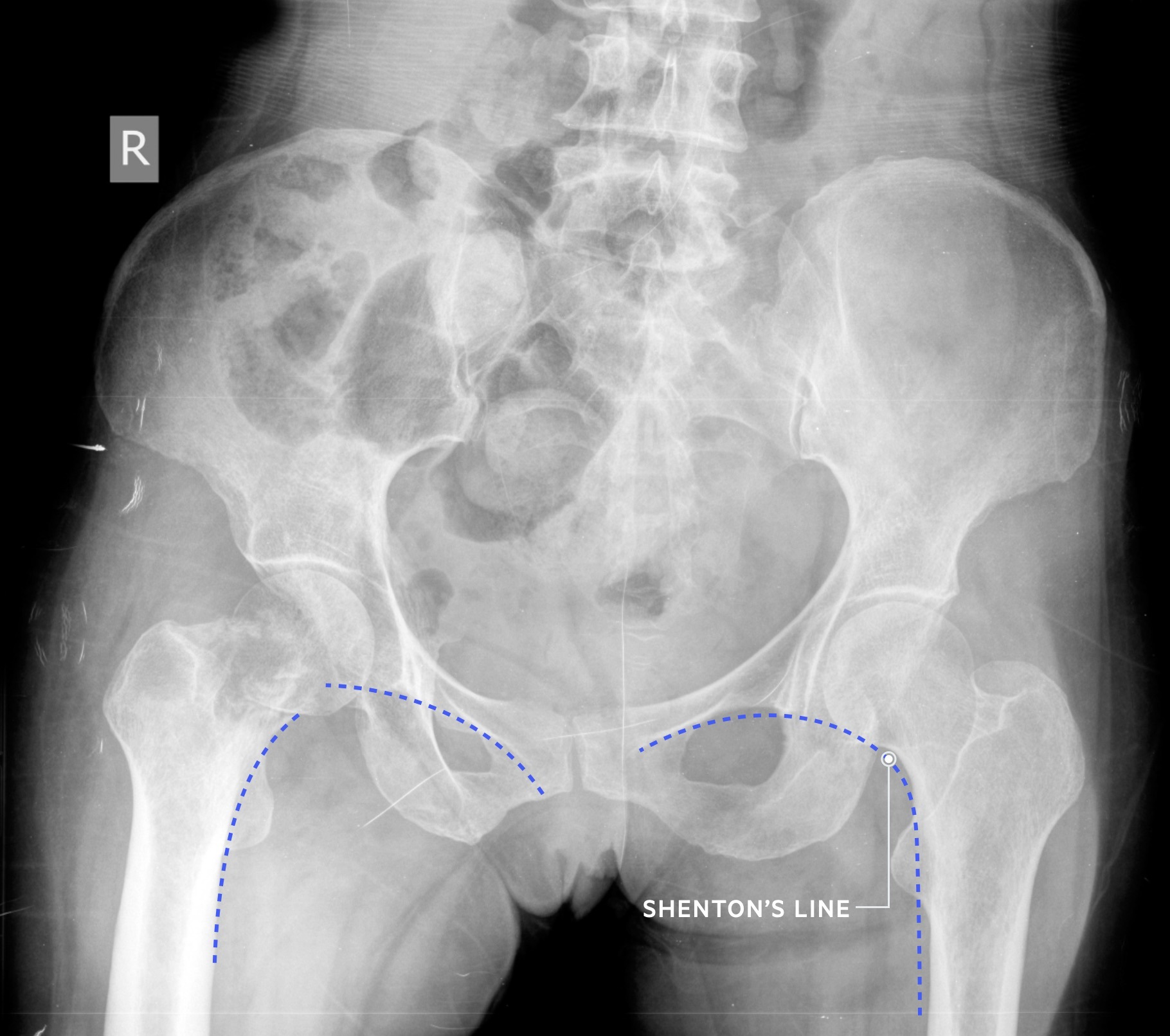
Shenton’s line - an imaginary curved line drawn along the inferior border of the superior ramus, along the inferomedial border of the neck of femur. It should be continuous and smooth.
Initial management
Initial management involves analgesia, routine investigations and pre-operative work-up.
Most A&E department will have hip fracture proformas that outline important parts of the initial management. The patient and family should be informed of the injury and its implications.
Routine investigations and catheter
Routine blood tests and two group and saves should be sent. All patient should have a CXR. Urine dipsticks and MSUs should be sent when relevant.
In the majority of cases a urinary catheter should be placed as urinary retention is common. Cognitive status should be assessed and recorded.
Analgesia
Appropriate analgesia should be administered - the use of NSAIDs is discouraged. Paracetamol and opiod analgesia should be prescribed with reference to the patients weight, renal function and age. In the absence of contraindications a fascia iliaca block should be offered.
Medication review
Patients may have an acute kidney injury requiring adjustments to regular medication. In general anticoagulants and antiplatelets are held - however context is key! If a patient has had a recent CABG or PCI for example discussion with cardiology / cardiothoracic surgery is warranted. Where reversal of anticoagulation or coagulopathy is needed discuss with haematology.
Pre-operative assessment
The orthopaedic team should review, mark, book and consent the patient. In most trusts medical teams or orthogeriatrics will also review the patient.
Where the patient lacks capacity, any lasting powers of attornery for health should be identified or a consent form 4 completed in the patients best interest.
Anaesthetic assessment should be obtained. The options of spinal anaesthesia or general anaesthetic should be discussed. The patient should be made NBM depending on when surgery is planned.
Surgical management
Most hip fractures are treated surgically, unless there are significant co-morbidities restricting surgical intervention. Surgical management differs between intra- and extra- capsular fractures.
The evidence shows without surgery, patients remain bedbound with high risk of blood clots, chest infections and other complications. Surgical fixation on the other hand allows early mobilisation (same-day or next day) and rehabilitation.
As such it is only in rare cases that conservative treatment is used. This can involve traction, bed rest or restricted mobilisation. Outcomes are often very poor in these patients.
NICE guidelines recommend surgery to be performed on the day of, or the day after, admission. The aim is to allow patients to fully weight bear (without restriction) in the immediate postoperative period.
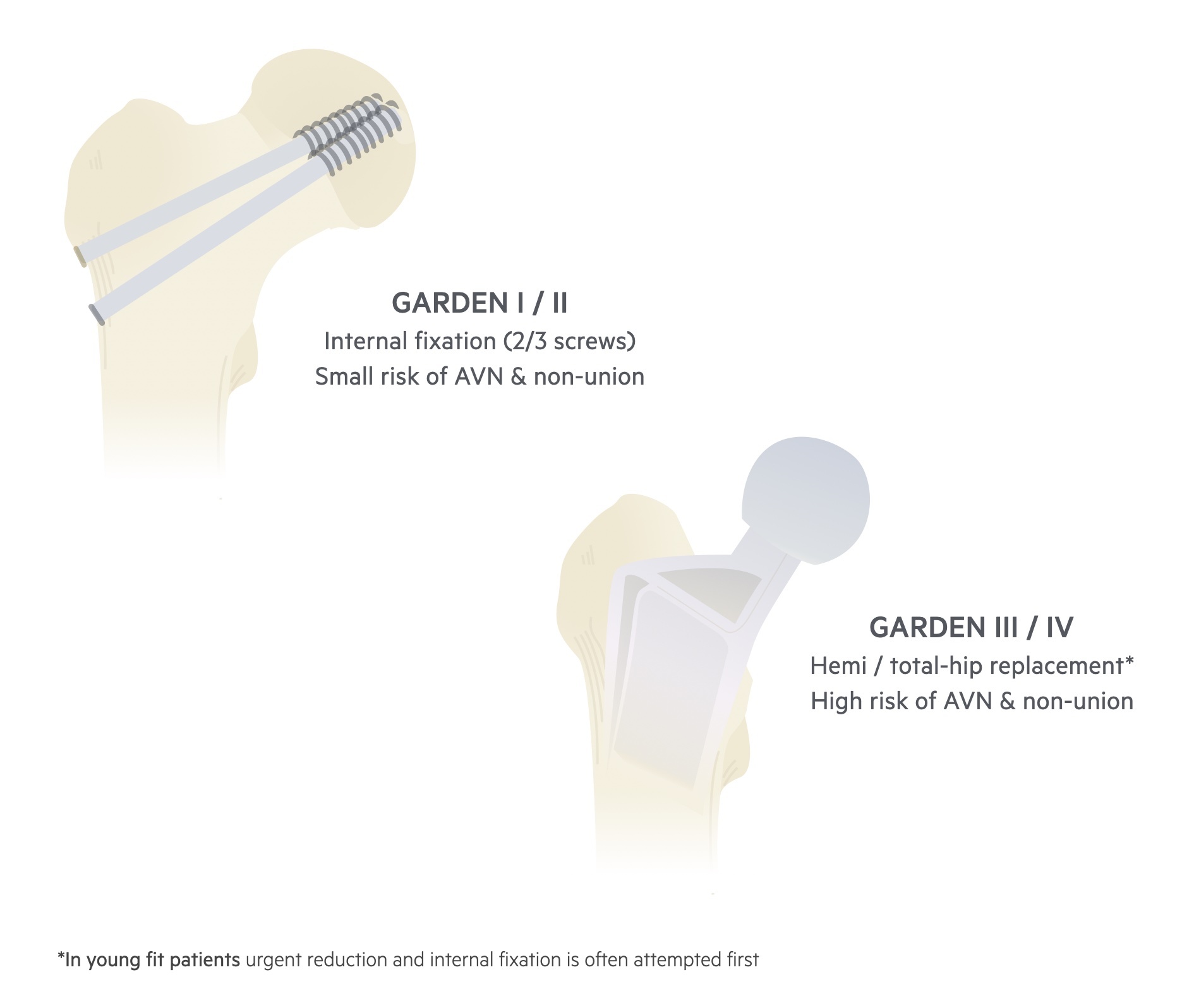
Intracapsular fractures
Minimally or non-displaced intracapsular fractures (e.g. Gardens I/II)
These are frequently treated with cannulated hip screws (often 2 or 3).
Displaced intra-capsular fractures (e.g. Gardens III/IV)
These tend to be managed either with a total hip replacement (THR) or a hemi-arthoplasty.
NICE advise that THR is offered to patients who:
- Are able to walk independently out of doors with no more than the use of a stick and
- Are not cognitively impaired and
- Are medically fit for anaesthesia and the procedure
Intertrochanteric fractures
These may be managed with a dynamic hip screw (DHS) or intra-medullary (IM) nail. DHS are unique in the fact that they allow the fracture ends to ‘slide’; this is thought to promote bone healing.
Subtrochanteric fractures
These tend to be managed with an intra-medullary (IM) nail.
Post-operative management
Post-operatively PT/OT are key helping patients mobilise and get home safely
Daily review
Delirium is common post-operatively (and pre-op) and should be screened for. Chest infection and urinary infection are also relatively common. Less often op site haematomas or op site infections may be seen.
Significant complications like peri-operative cardiac events and DVT/PE may occur. Patients should be reviewed by both the orthopaedic surgeons and the orthogeriatricians. Prophylaxis for fragility fractures should be considered.
VTE prophylaxis
Patients are at increased risk of DVT and PE following a hip fracture and surgical fixation. Normally prophylactic dose LMWH is started 6-12 hours post-op. This will normally be continued for a minimum of one month, though it may be longer depending on circumstance (e.g. prolonged hospital stay). TED stockings and intermittent pneumatic compression may also be used.
Of course many patients in this cohort will already be formally anticoagulated for other conditions such as AF. In these patients anticoagulation should be resumed under the instruction of the operating team +/- haematology/cardiology advice.
Physiotherapy and Occupational therapy
Patients should be encouraged to mobilise the day after surgery. Early mobilisation helps reduce the risk of blood clots, chest infections and deconditioning. Patients should have daily physiotherapy as an inpatient and a plan for community support at discharge.
Patients home situation should be reviewed and a re-ablement package instituted as needed to (ideally) return the patient to their home or care home.
Last updated: October 2021
Further reading
- NICE guideline NG124: Hip fracture: management
- NICE guideline NG89: Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism
Have comments about these notes? Leave us feedback
