6. Tachycardias
Notes
Introduction
Tachycardia refers to an abnormally fast heart rate.
Tachycardia is usually defined as an abnormally fast heart rate greater than 100 bpm. We refer to all the abnormally fast heart rhythms as tachyarrhythmias. When a tachyarrhythmia occurs intermittently, we call it paroxysmal.
Tachyarrhythmias may develop due to an ectopic foci of electrical activity within the atria, atrioventricular node (AVN) or ventricles. The aetiology of these ectopic foci can get quite complex, but is broadly due to problems with impulse conduction (i.e. transmission of electrical activity) or impulse formation (i.e. generation of electrical activity).
- Impulse conduction problems: caused by conduction blocks (discussed in our Bradycardia notes) and formation of reentrant circuits.
- Impulse formation problems: enhanced autorhythmicity (pacemaker site away from SAN increases rate of depolarisation) or triggered activity (abnormal electrical activity during repolarisation when cells should be ‘quiet’).
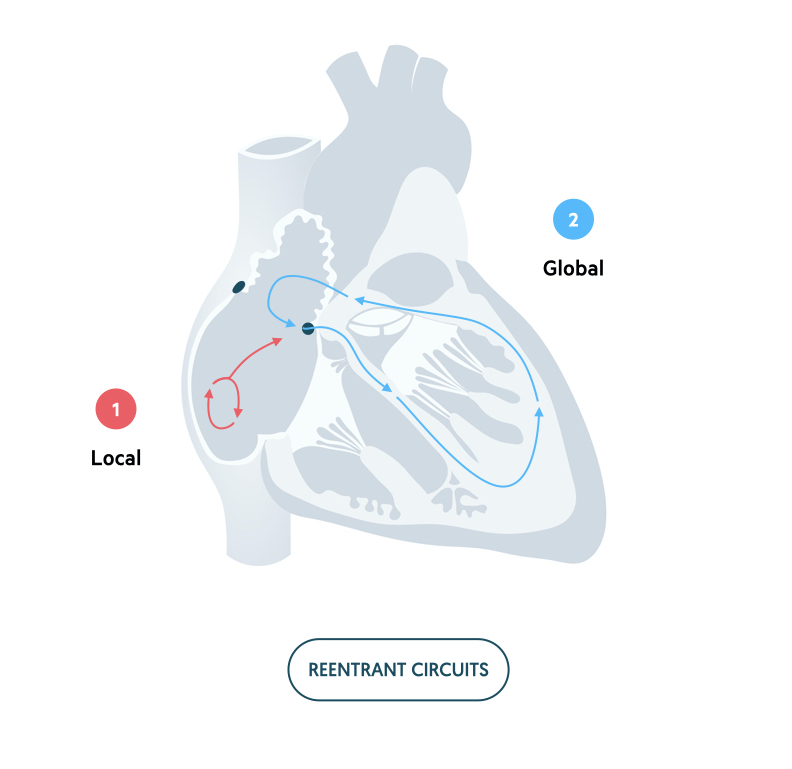
Reentrant circuits
Reentrant circuits are one of the main mechanisms underlying tachyarrhythmias.
A reentrant circuit refers to a continuous wave of depolarisation in a circular path. As the depolarising wave returns its site of origin, it reactivates that site leading to a continuous cycle. There are said to be three criteria for development of a reentrant circuit, but this is beyond the scope of these notes. Importantly, reentrant circuits can lead to generation of three types of arrhythmia:
- Ectopic beat
- Non-sustained tachyarrhythmia (i.e. paroxymal)
- Sustained tachyarrhythmia
Reentrant pathways may be considered as micro-reentrant occurring in a localised area of cardiac tissue or macro-reentrant occurring around a larger area of cardiac tissue. Atrial flutter and atrioventricular reentrant tachycardia (AVRT) are classical examples of macro-reentrant tachyarrhythmias.
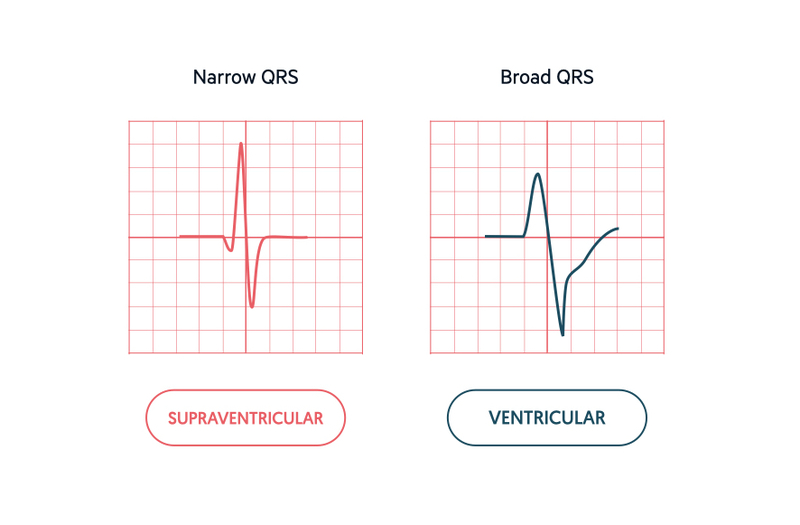
Origin of tachyarrhythmia
Tachyarrhythmias are broadly divided into supraventricular (above ventricles) and ventricular (within ventricles).
The key to differentiating a supraventricular from ventricular tachyarrhythmia is the width of the QRS complex (i.e. narrow vs broad).
During normal electrical activity, the coordinated excitation of the ventricles via the bundle of His, bundle branches and Purkinje fibres leads to fast depolarisation and a narrow QRS (< 120 ms). If electrical activity is initiated within the ventricles and travels by an abnormal path across the ventricular muscle, depolarisation occurs at a slower rate. This results in an abnormal, wide appearing QRS complex (> 120 ms).
Supraventricular rhythms:
- Sinus tachycardia
- Atrial tachycardia
- Atrial flutter
- Atrial fibrillation
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrioventricular reentrant tachycardia (AVRT)
Ventricular rhythms:
- Ventricular tachycardia
- Polymorphic ventricular tachycardia
Accessory pathways
The width of the QRS complex can provide evidence of the origin of arrhythmias in most cases. However, accessory pathways can be an exception to this rule.
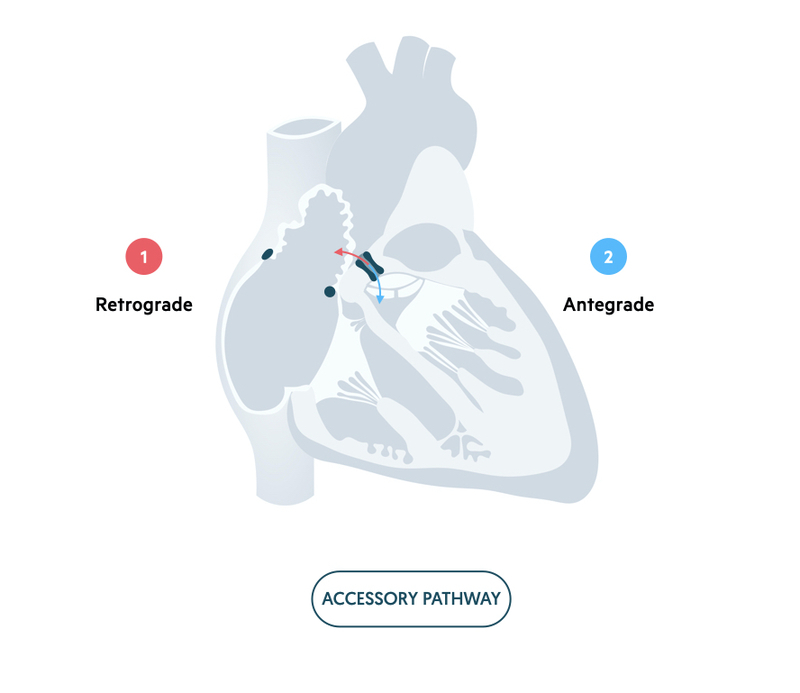
The AVN allows conduction of electrical activity between the atria and ventricles. The fibrous skeleton of the heart prevents electrical activity reaching the ventricles by another route. Occasionally, patients may have an accessory pathway within the heart. This refers to an abnormal connection between the atria and ventricles away from the AVN that allows electrical activity to pass through.
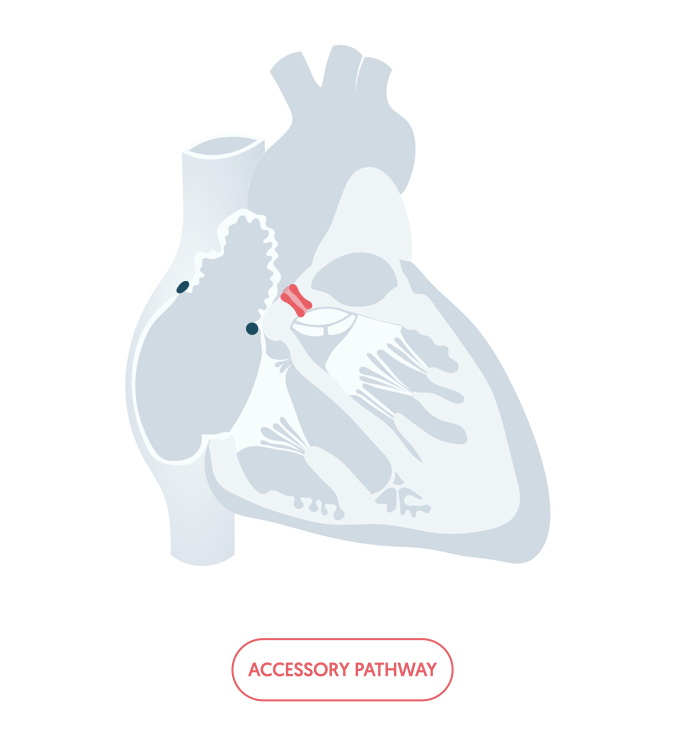
If electrical activity is conducted to the ventricles via the accessory pathway, it will take an abnormal slow route across the ventricles. This can lead to a broad QRS. Therefore, in the context of an accessory pathway a board QRS may be supraventricular in origin. As a general rule, a tachyarrhythmia with a broad QRS should be treated as ventricular in origin unless there is a known accessory pathway or specialist cardiology advice has be sought.
Sinus tachycardia
Sinus tachycardia refers to sinus rhythm with a heart rate > 100 bpm.
Under normal circumstances at rest, our heart should be in sinus rhythm with an accompanying rate of 60-100 bpm. If the defining features of normal sinus rhythm are met but the heart rate is fast (> 100 bpm), we call it sinus tachycardia.

Sinus tachycardia is a normal physiological response when the body is put under stress. This can occur due to exercise, intercurrent illness, or underlying pathology.
Atrial tachycardia
Atrial tachycardia occurs due to an abnormal focus of activity undergoing rapid depolarisation in the atria.
There are different types of atrial tachycardia depending on the origin of the abnormal electrical activity. It may be due to a single foci undergoing regular, organised depolarisation, multiple sites of competing atrial activity or a small reentrant circuit in the atria.
On an ECG, the characteristic feature of atrial tachycardia is a fast tachyarrhythmia (>100 bpm) with a narrow QRS (normal conduction via AVN to ventricles) and abnormal P waves. Atrial tachycardia is usually a regular tachyarrhythmia, but multi-focal atrial tachycardia may present with an irregular rhythm.
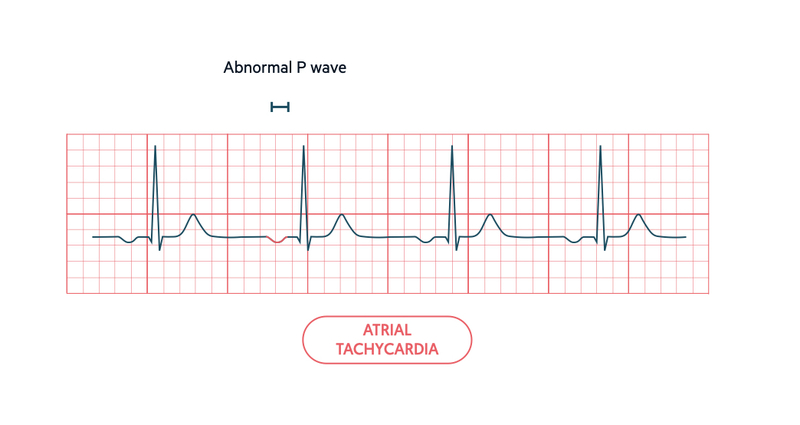
Normal P wave morphology is reliant on normal depolarisation of the atria from SAN to AVN. When electrical activity occurs at another site, the P wave will appear different. The actual morphology depends on the area in relation to the AVN. Typically, there is an abnormal P wave axis with inverted (negatively deflected) P waves in the inferior leads (II, III, aVF).
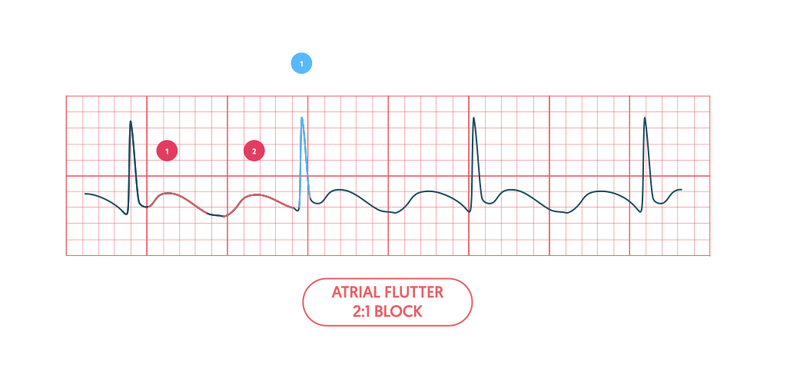
Atrial flutter
Atrial flutter is a classical example of a macro-reentrant circuit, which occurs within the atria.
Atrial flutter is a specific type of atrial tachycardia that occurs due to a rapid macro-reentrant circuit within the atria. It has a characteristic rate of depolarisation > 250 beats per minute (bpm).
Due to the rapid depolarisation, the isoelectric line on the ECG is not flat. Instead, it appears as a typical sawtooth pattern, which is best visualised in the inferior leads (II, III, aVF).
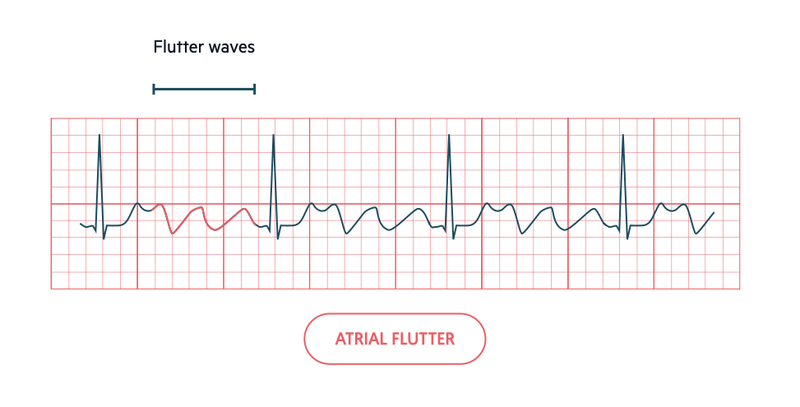
Due to the fast atrial rate the AVN causes a ‘block’. This means some of the atrial activity is not conducted to the ventricles. This is a physiological response of the AVN to allow time for ventricular filling. In atrial flutter this is classically seen as a 2:1 block (two flutter waves to one QRS complex) but higher degrees of block can occur.
Atrial fibrillation
Atrial fibrillation (AF) refers to irregular atrial contraction, caused by chaotic impulses.
AF is an extremely common tachyarrhythmia that occurs due to multiple waves of spontaneous depolarisation leading to fragmentation of the normal electrical activity. This causes muscle fibres to contract independently leading to ‘fibrillation’ of the atrial muscle.
As multiple waves of electrical activity (varying in strength) reach the AVN, it intermittently conducts these to the ventricles. This results in an irregular rhythm, which is characterised by three main ECG features:
- Irregularly irregular rhythm
- Absence of P waves (no coordinated atrial activity)
- Irregular, fibrillating baseline.
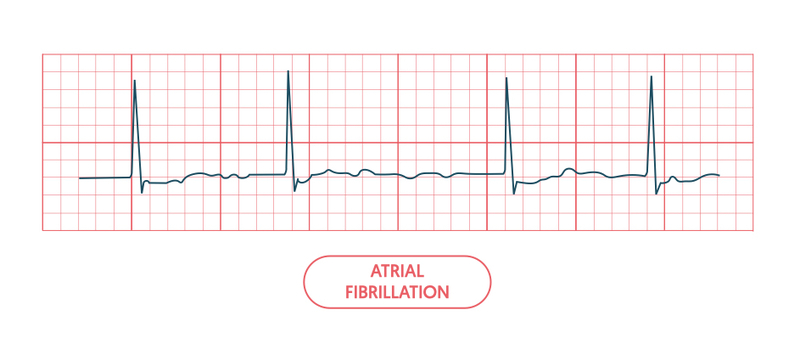
For more information see our notes on atrial fibrillation.
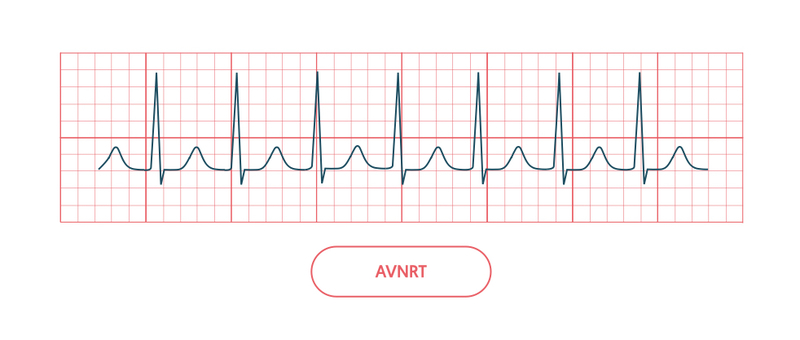
Supraventricular tachycardia
Abnormal tachyarrhythmias derived from reentrant circuits involving the AVN are known as ‘SVT’.
Confusingly, a supraventricular tachycardia (SVT) can refer to the origin of a tachyarrhythmia or a subset of abnormally fast heart rhythms that are due to reentrant circuits involving the AVN.
In clinical practice, the term SVT is reserved for these reentrant arrhythmias, which are broadly divided into two types: atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT).
AVNRT
This is the most common SVT (50-60%), which typically occurs in patients with a structurally normal heart. It is due to additional conduction pathways within the AVN, which allows initiation of a reentrant circuit.
There is usually a rapid, narrow-complex tachycardia with absent P waves.
AVRT
This is the second most common SVT (30%), which usually presents at a younger age than AVNRT and can occur in children. It is due to an accessory pathway away from the AVN. These pathways may enable electrical impulses to pass antegrade (atria to ventricles) or retrograde (ventricles to atria), which establishes the reentrant circuit.
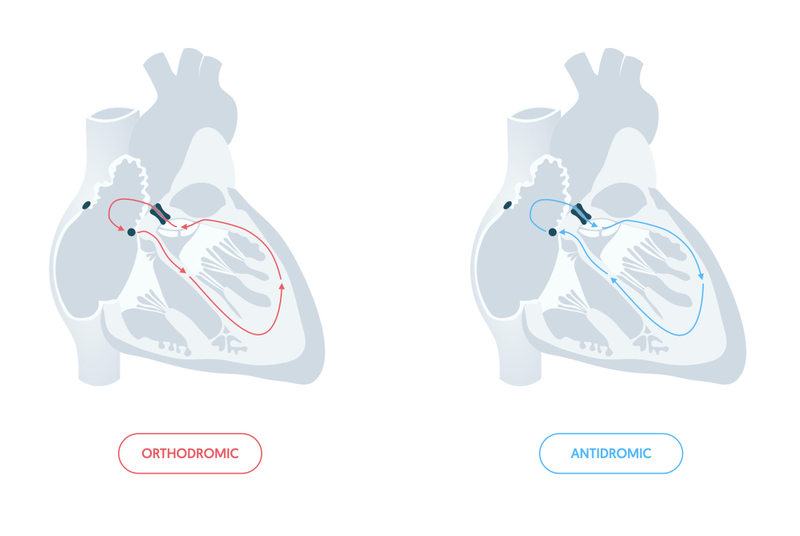
It can be difficult to distinguish AVRT from AVNRT on an ECG during the tachyarrhythmia. The characteristics of the ECG depends on the direction of electrical impulses via the accessory pathway during the tachyarrhythmia. We refer to these directions as orthodromic and antidromic.
- Orthodromic (common): antegrade conduction via AVN, retrograde conduction via accessory pathway. Appearance similar to AVNRT. Rapid, narrow complex (QRS <120 ms) with absent P waves (or abnormal if retrograde conduction seen).
- Antidromic (uncommon): antegrade conduction via accessory pathway, retrograde conduction via AVN. Appearance similar to VT. Rapid, broad-complex (QRS >120 ms) with absent P waves.
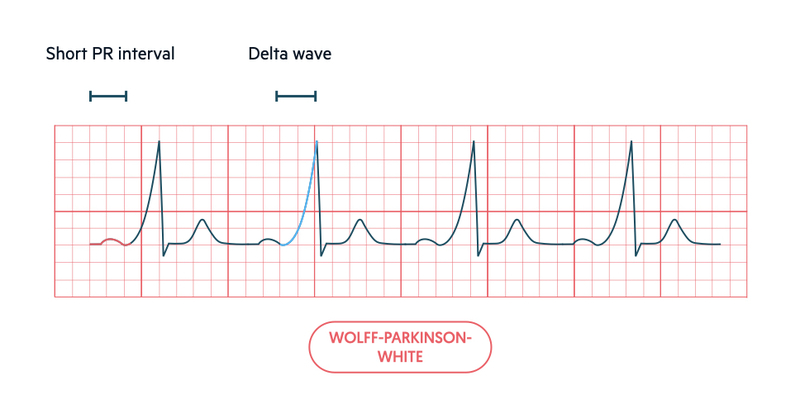
On a resting ECG, we may see evidence of an accessory pathway due to pre-excitation (early depolarisation of the ventricles). The classic pre-excitation syndrome that leads to episodes of AVRT is Wolff-Parkinson-White (WPW) syndrome.
Wolff-Parkinson-White syndrome
WPW is a preexcitation syndrome that is characterised by a congenital accessory pathway and episodic tachyarrhythmias.
The accessory pathway in WPW is usually referred to as the ‘Bundle of Kent’ and it can allow conduction antegrade or retrograde. If there is antegrade conduction during normal electrical activity it can be seen on the resting ECG. Retrograde only conduction ‘conceals’ the accessory pathway.
The ECG pattern in WPW is due to the early (i.e. pre-excitation) of the ventricles via the accessory pathway. This leads to a short PR interval as there is no AV conduction delay, which is followed by an early slurred upstroke in the QRS complex, called a delta wave. The remaining QRS complex is normal because the usual conduction via the AVN, His bundle and branches ‘catches up’ with the pre-excitated impulse.
The main concern in WPW is development of AF, which may be conducted to the ventricles leading to a rapid ventricular response. This could deteriorate into ventricular fibrillation.
Ventricular tachycardia
Ventricular tachycardia occurs due to a focus of electrical activity in the ventricles undergoing rapid depolarisation.
Ventricular tachycardia (VT) occurs due to rapid, recurrent ventricular depolarisation from a focus within the ventricles. This is commonly due to scarring of the ventricles following myocardial infarction.
On an ECG, it is seen as a rapid, broad-complex tachycardia (QRS >120 ms).
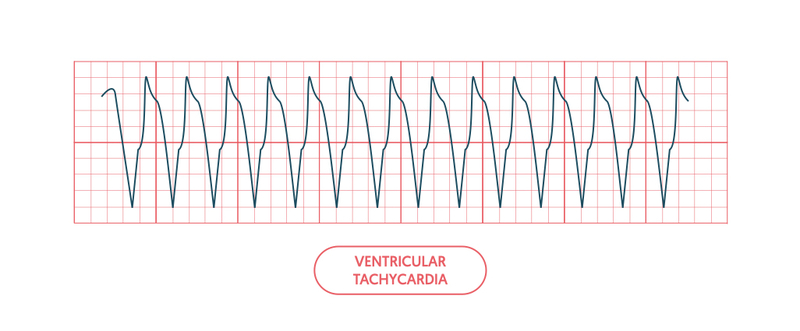
VT is a life-threatening arrhythmia that may lead to loss of consciousness, loss of cardiac output and ultimately cardiac arrest. VT without a pulse is one of the ‘shockable’ cardiac arrest rhythms.
It may be difficult to distinguish VT from a supraventricular tachyarrhythmias that presents with a broad QRS complex (e.g. SVT with bundle branch block, AVRT with antegrade conduction via accessory pathway). We refer to these supraventricular rhythms with abnormal conduction as SVT with aberrancy.
Certain ECG features help differentiate these two conditions. However, this is beyond the scope of these notes.
Polymorphic VT (Torsades de pointes)
Polymorphic VT is a particular type of VT that is due to depolarisation of multiple foci within the ventricles leading to variable QRS complexes. It is usually secondary to myocardial ischaemia.
Torsades de pointes is a subtype of polymorphic VT that is characterised by ventricular tachycardia that ‘twists’ around the isoelectric line. This subtype occurs secondary to a prolonged QT interval.
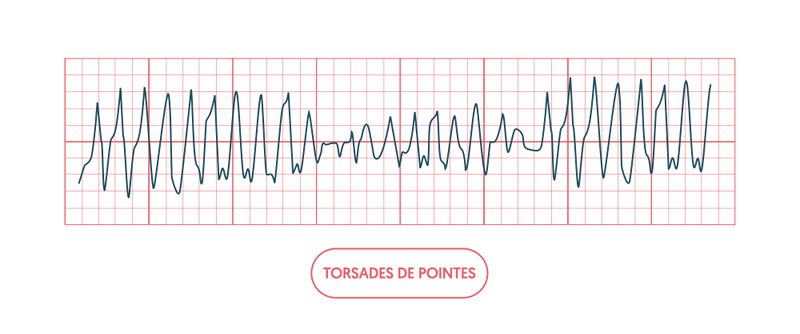
Torsades de pointes is important to recognise because the management is aimed at shortening the QT interval with intravenous magnesium sulphate. If a patient is unstable with Torsades de pointes, they should undergo immediate DC cardioversion as with any unstable tachyarrhythmia.
Ventricular fibrillation
This arrhythmia is incompatible with life and will result in loss of consciousness and cardiac arrest.
Ventricular fibrillation (VF) occurs when the ventricular muscle fibres contract independently. On the ECG, this is seen as no coordinated electrical activity with a chaotic, fibrillating baseline.
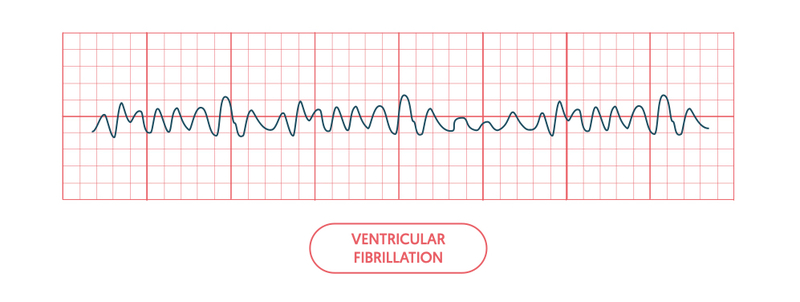
VF is incompatible with life and patients who development this rhythm will go into cardiac arrest. It is one of the ‘shockable’ cardiac arrest rhythms that requires immediate DC cardioversion.
Last updated: March 2022
Have comments about these notes? Leave us feedback
