Anaphylaxis
Notes
Overview
Anaphylaxis is a serious systemic hypersensitivity (allergic) reaction that is rapid in onset and may cause death.
Anaphylaxis can be a life-threatening condition that is broadly defined as a severe, generalised or systemic hypersensitivity reaction that is characterised by airway and/or breathing and/or circulation problems that is usually associated with skin and mucosal changes (i.e. urticaria and angio-oedema). Features of anaphylaxis are usually sudden with rapid progression so urgent assessment and management is vital.
Anaphylaxis is the most severe form of an allergic reaction that forms part of a spectrum. Allergic reactions are characterised by skin changes (e.g. urticaria) and subcutaneous/mucosal changes (e.g. angio-oedema). The crucial differentiating factor between these changes and anaphylaxis is the presence or airway, breathing, and/or circulatory dysfunction.
Two key principles:
- Skin and/or mucosal changes alone are not a sign of anaphylaxis
- Skin and/or mucosal changes may be subtle or absent in 10-20% of anaphylaxis
Epidemiology
The mortality associated with anaphylaxis is less than 1% in patients presenting to hospital.
The true incidence of anaphylaxis is difficult to quantify. It is estimated that 1 in 300 people will experience an episode of anaphylaxis during their lifetime with an incidence in Europe of 1.5-7.9 per 100,000 person-years.
The overall risk of recurrent anaphylaxis is estimated at 1 in 12 per year within the UK.
Aetiology
Anaphylaxis may be triggered by a very broad range of allergens.
A specific trigger is commonly identified in anaphylaxis but up to 30% of cases may be idiopathic (i.e. no known cause). The most commonly recognised allergens include food, drugs and venom (e.g. insect bites or stings).
- Food (most common in young people): common examples include peanuts, walnuts, shellfish, Cow’s milk, eggs
- Drugs: common examples include antibiotics, neuromuscular blocking agents, NSAIDs, Chlorhexidine
- Venom: stinging insects (e.g. honeybees, fire ants, yellow jackets) and biting insects (less common)
- Occupational: latex
- Food additives
The above causes typically result in an immunological reaction that is mediated by immunoglobulin E (IgE) leading to mast cell degranulation and release of chemical mediators (see pathophysiology). Some alternative immunological mechanisms have been identified (e.g. complement-mediated) as well as non-immunological mechanisms.
In non-immunological mechanisms there is direct activation of mast cells and basophils leading to release of chemical mediators such as histamine. Examples include:
- Physical factors: exercise, cold, heat. Exercise is often associated with a cofactor (e.g. food or drug)
- Radiological contrast agents
- Medications: NSAIDs, codeine, vancomycin. NSAIDs may cause both non-immunological and IgE-mediated reactions.
Pathophysiology
The predominant mechanism of anaphylaxis is exposure to an allergen leading to IgE-mediated activation of mast cells and basophils.
Traditionally, the term ‘anaphylaxis’ was reserved for IgE-mediated reactions and ‘anaphylactoid reaction’ for non-IgE-mediated reactions. However, the two reactions are indistinguishable and the World Allergy Organization (WAO) now advises immunological anaphylaxis (e.g. IgE-mediated) and non-immunological anaphylaxis (e.g. direct mast cell activation).
We briefly review the formation of an IgE-mediated allergic reaction.
IgE-mediated allergic reaction
IgE is one of five types of antibody in the body. IgE, like all antibodies, are produced by B cells. IgE is normally involved in defence against parasitic disease, but is also central to the pathophysiology of ‘allergic’ disease. Allergy refers to an exaggerated immune response to an otherwise innocuous substance (e.g. pollen/nuts).
Sensitisation
In development of an allergic response there is an initial process called sensitisation. After entry of an allergen into the body, it is taken up by antigen-presenting cells that interact with T-helper type 2 (Th2) cells that signal for stimulation of B-cells within lymphoid tissue. This leads to allergen-specific IgE production by B cells. The released IgE then binds to mast cells and some basophils located around the body, particularly in the skin, gut and lungs.
Re-exposure
Following sensitisation, patients may develop an allergic-reaction on re-exposure. If the patient is re-exposed to the same allergen and it diffuses in the proximity of these mast cells it can lead to binding on the IgE antibodies. Binding leads to cross-linking and aggregation that initiates intra-cellular signalling. If this signal is strong enough, it leads to activation and degranulation causing release of massive amounts of chemical mediators including histamine, tryptase, cytokines, prostaglandin and leukotrienes.
These chemical mediators act directly on tissue as well as recruit additional inflammatory cells (e.g. eosinophils). They cause local inflammation, vessel dilatation, loss of vascular integrity and fluid extravasation leading to oedema. The combination of oedema and massive vasodilatation can lead to airway obstruction, bronchoconstriction and reduced cardiac output. This culminates in marked hypoxia and hypotension that leads to anaphylactic shock.
Clinical features
Anaphylaxis is characterised by sudden onset airway and/or breathing and/or circulatory dysfunction often with typical skin/mucosal changes.
The sudden and rapid development of symptoms affecting the airway, breathing and/or circulation following exposure to an allergen is classic for anaphylaxis. A range of clinical features may be seen to affect different organ systems of which none are specific for anaphylaxis. It is the combination of features with rapidity of symptoms that suggests the diagnosis.
Patients with anaphylaxis should be assessed with an ‘ABCDE approach’ and here we present the clinical features in this manner.
Airway
- Throat/tongue swelling
- Horse voice
- Stridor
Breathing
- Dyspnoea
- Wheeze
- Hypoxia
- Persistent cough
- Respiratory arrest
Circulation
- Pale, clammy
- Dizziness
- Tachycardia
- Hypotension
- Cardiac arrest
Disability
Assessment of conscious level is vital. Decreased brain perfusion may reduce conscious level and compound airway obstruction. Features may include:
- Reduced Glasgow coma score (GCS)
- Agitation
- Confusion
- ‘Feeling of impending doom’
Exposure
Cutaneous findings are often the first feature of anaphylaxis, but may be absent in 10-20% of cases. Signs may be subtle (e.g. patchy erythema only). The two classic signs are urticaria and angio-oedema:
- Urticaria: red, itchy, raised papules or plaques
- Angio-oedema: swelling affecting deeper tissue. Commonly seen in lips, mouth and/or face
Gastrointestinal clinical features may also be present due to degranulation of mast cells in the GI tract. In the absence of airway, breathing, and/or circulation problems they are unlikely to represent anaphylaxis.
- Nausea
- Vomiting
- Diarrhoea
- Abdominal pain
Diagnosis & investigations
Anaphylaxis is a clinical diagnosis based on rapid development of characteristic signs and symptoms.
All patients with suspected anaphylaxis require urgent assessment using an ‘ABCDE’ approach. Anaphylaxis should be suspected in any patient with sudden onset and rapidly developing airway and/or breathing and/or circulatory dysfunction that is usually accompanied by urticaria and/or angio-oedema.
Basic investigations
A series of basic investigations should be requested including urgent bloods (e.g. full blood count, urea & electrolytes), arterial or venous blood gas, 12-lead ECG and chest x-ray. These investigations are not specific to anaphylaxis, instead they represent a routine set of investigations for any critically unwell patient.
Other investigations may be warranted depending on the suspected trigger or co-morbidities of the patient.
Mast cell tryptase
Mast cell tryptase is one of the major proteins released during activation and degranulation. This means its concentration will increase during an episode of anaphylaxis. Therefore, mast cell tryptase can be used as a surrogate marker of anaphylaxis and analysis of this protein is used in the follow-up of anaphylaxis. Importantly, it is NOT useful in the initial recognition and management of anaphylaxis.
Mast cell tryptase should be collected 1-2 hours after onset but no later than 4 hours as levels begin to fall and can be normal within 6-8 hours. A minimum of one sample should be taken, but ideally, three samples should be collected as follows:
- Immediate sample: taken as soon as possible after onset. Should NOT delay treatment
- Second sample: taken at 1-2 hours after onset. Should be no later than 4 hours. Minimum required sample
- Third sample: taken at least 24 hours after onset. Often taken at follow-up allergy clinic. Acts as the baseline level
Mast cell tryptase helps to confirm the diagnosis of anaphylaxis after the initial episode. However, a normal value does not exclude anaphylaxis. It can be useful because many conditions may resemble anaphylaxis (e.g. hereditary angio-oedema)
Emergency management
The principal pharmacological treatment of anaphylaxis is intramuscular adrenaline.
The emergency management of anaphylaxis should be in line with the Resuscitation council 2021 guidelines. In a patient with suspected anaphylaxis the following algorithm should be followed:
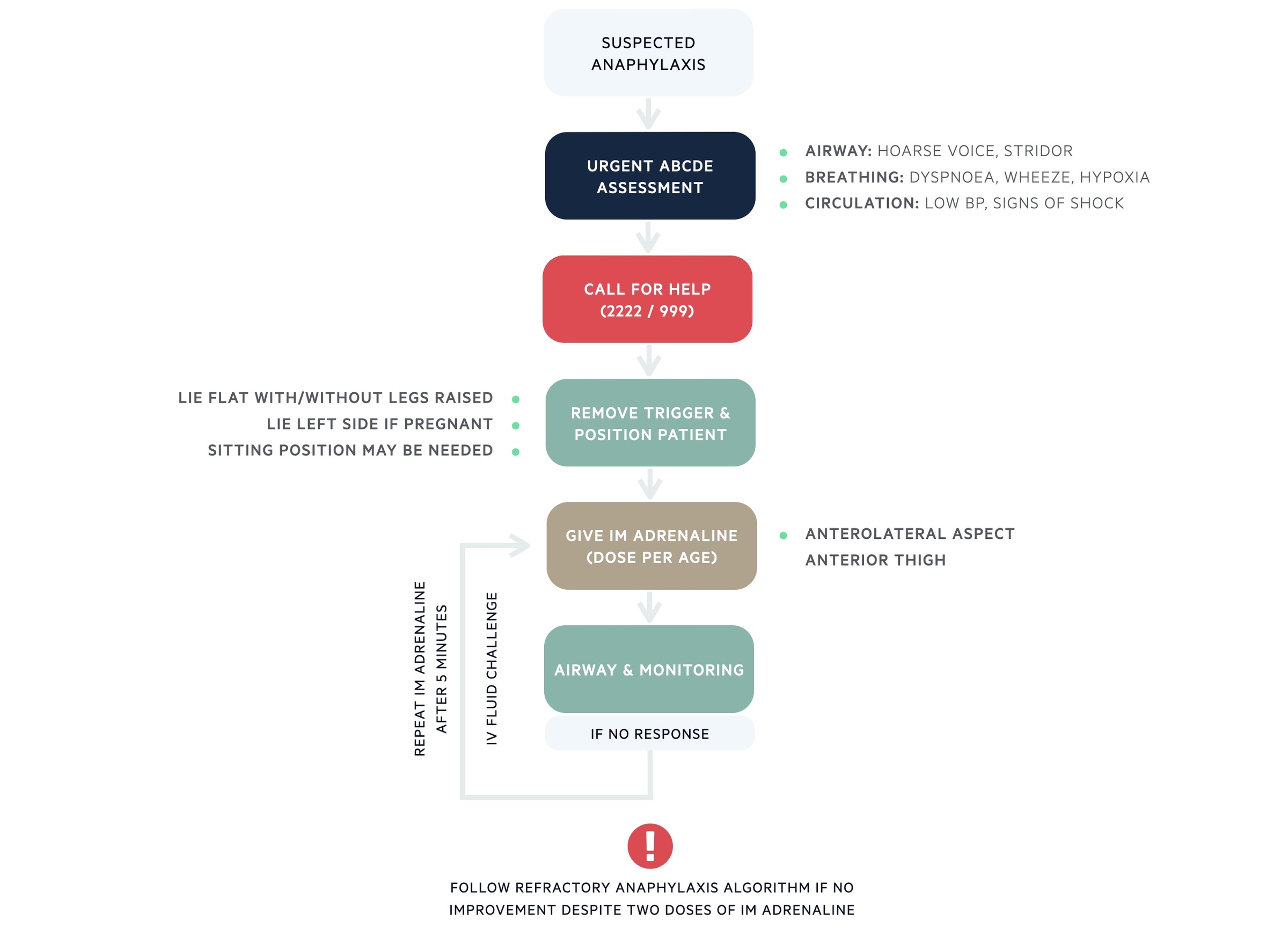
Adrenaline
Adrenaline is the principal medication used to treat anaphylaxis. It is given as an intramuscular (IM) injection (even if the intravenous route is available) into the anterolateral aspect of the anterior thigh. The concentration of adrenaline should be 1:1000 that is equivalent to 1mg/ml. The dose depends on the age of the patient:
- Adult and child >12 years old: 500 micrograms IM (0.5 mL of 1mg/mL adrenaline)
- 6-12 years old: 300 micrograms IM (0.3 mL of 1mg/mL adrenaline)
- 6 months - 6 years: 150 micrograms IM (0.15 mL of 1mg/mL adrenaline)
- < 6 months: 100-150 micrograms IM (0.1-0.15 mL of 1mg/mL adrenaline)
NOTE: Give 300 micrograms IM (0.3 mL) in a child who is small or prepubertal.
Adrenaline treats anaphylaxis by its action on two receptors:
- Alpha-adrenergic receptors: causes vasoconstriction that reverses peripheral vasodilation and reduces tissue oedema
- Beta-adrenergic receptors: causes bronchodilation, increases myocardial contractility and suppresses histamine/leukotriene release. Also inhibits mast cell activation
A second dose of adrenaline may be given after 5 minutes if there is no improvement. If there is no improvement after two doses of adrenaline treatment should follow the refractory anaphylaxis algorithm in line with the resuscitation council guidance.
Anti-histamines
The use of anti-histamines was traditionally part of the initial management of anaphylaxis. However, they are currently NOT recommended as part of the initial management. They can be used to treat skin symptoms (e.g. urticaria/angio-oedema) that occur alongside anaphylaxis but use should not delay administration of adrenaline and IV fluids.
A second-generation non-sedating agent (e.g. cetirizine) should be given via the oral route. If the oral route is not available, chlorphenamine may be given intravenously or intramuscularly. This is a first-generation sedating anti-histamine.
Corticosteroids
The use of corticosteroids (e.g. intravenous hydrocortisone) was traditionally part of the initial management of anaphylaxis. The primary use was to prevent the late phase inflammatory response (i.e. biphasic reaction). However, there is little evidence they shorten protracted symptoms. Therefore, the routine use of steroids is no longer advised.
Corticosteroids may be considered for refractory reactions or ongoing asthma/shock after the initial resuscitation. Importantly, they should not be given in preference to adrenaline.
Intravenous fluids
Patients with evidence of hypotension/shock or those that have a poor initial response to adrenaline should be given an intravenous fluid bolus. The initial bolus should be:
- Adults: 500-1000 mL of non-glucose-containing crystalloid (e.g. 0.9% sodium chloride, Hartmann’s)
- Children: 10 mL/kg of non-glucose-containing crystalloid (e.g. 0.9% sodium chloride, Hartmann’s)
Further fluids should be given as necessary and recognise that large volumes of fluid may are required for patients with anaphylaxis (e.g. up to 5 litres in adults). With larger volumes of fluid, a balanced crystalloid (e.g. Hartmann’s) is preferred to 0.9% sodium chloride.
Refractory anaphylaxis
Defined as anaphylaxis requiring ongoing treatment despite two appropriate doses of adrenaline.
The exact mechanism of refractory anaphylaxis is poorly understood. However, it is likely due to a combination of delayed administration of adrenaline, ongoing release of inflammatory mediators or diminished response to adrenaline.
Patient with refractory anaphylaxis should be referred to the critical care team for ongoing support. The principal treatment is initiation of an adrenaline infusion. Repeated doses of intramuscular adrenaline should be given at 5 minute intervals whilst the intravenous infusion is being prepared and ongoing fluid resuscitation should be administered.
For more information, see the refractory anaphylaxis algorithm published by the resuscitation council.
Biphasic reaction
This refers to the recurrence of symptoms several hours later in the absence of exposure to the allergen.
The biphasic reaction is estimated to occur in around 5% of patients with anaphylaxis. The median time to developing a biphasic reaction is 12 hours. It can be difficult to distinguish this reaction from sustained anaphylaxis that had a transient response to adrenaline or further absorption of the allergen in the gastrointestinal tract (food allergies).
Risk factors for developing a biphasic reaction include:
- Severe initial presentation
- More than one dose of adrenaline required
- Delay in giving adrenaline (>30-60 minutes from initial symptoms)
Due to the risk of a biphasic reaction patients are traditionally observed for a period of 6-12 hours, however, fatal outcomes are very rare. More recently, depending on a patients risk of developing a biphasic reaction, observation may be for a shorter period of time.
- Deemed at low risk: minimum 2 hours observation from resolution
- Deemed at moderate risk: minimum of 6 hours observation from resolution
- Deemed high risk: minimum of 12 hours observation from resolution
Specific criteria are outlined in the resuscitation council guidelines on anaphylaxis that help to determine a patients risk of anaphylaxis. For considering early discharge (i.e. within 2 hours), several criteria must be met that includes already having unused adrenaline auto-injectors and knowing how to use them.
Follow-up management
Information on discharge and follow-up in an allergy clinic are important following anaphylaxis.
Discharge information
Several broad principles are required prior to discharging a patient following an anaphylactic reaction.
- Review by a senior clinician: helps to determine whether further observation is warranted and patient is safe to go home
- Patient information on anaphylaxis: should discuss clinical features of anaphylaxis, the biphasic reaction and what to do if they occur. Also need to give advice on avoiding triggers (if possible) and provide information about support groups
- Prescriptions: patients should be prescribed a new or replacement adrenaline auto-injector (except in drug induced reactions unless it would be difficult to avoid the drug). There are various brands (e.g. Epipen®) and patients should be trained how to use them. Usually come as dose of 300 mcg (adults) or 150 mcg (children). Patients should have two devices at all times
- Referral: patients should be referred to an allergy/immunology clinic on discharge
Allergy clinic
All patients should be referred to an allergic clinic on discharge. Each patient will be reviewed by a clinical immunologist or allergist to determine whether the reaction was true anaphylaxis and the likely underlying cause. This should be conducted in an outpatient clinic once the patient is stable and discharged from hospital
Numerous test can be requested including mast cell tryptase to compare with the level at the time of the reaction, allergen-specific IgE antibodies and skin-prick testing.
- Allergen specific IgE antibodies: this describes performing assays for IgE specific to an allergen to help diagnose allergic disease. This is an in vitro blood test that has no risk to the patient and is generally not affected by medications. A positive test means the patient is sensitised to the allergen and may have a clinical reaction to it. However, sensitisation alone is not enough to diagnose an allergy because not all patients will develop symptoms on re-exposure
- Skin testing: this describes a rapid, sensitive and cost-effective in vivo test. Allergens are introduced into the skin by a ‘skin prick’. The allergens comes into contact with cutaneous mast cells that leads to a transient urticarial reaction if the patient is ‘allergic’. It cannot be performed in patients at high risk of anaphylaxis on re-exposure
Complications
Anaphylaxis is a life-threatening condition that can lead to death without urgent treatment.
Without treatment, anaphylaxis can be fatal but thankfully the mortality is estimated as <1% in patients presenting to hospital. Approximately 50% of deaths are due to circulatory collapse (shock) and 50% due to respiratory arrest.
Allergic reaction secondary to food are more likely to lead to respiratory arrest. Insect stings/bites and medications are more likely to lead to circulatory collapse.
Last updated: November 2021
Have comments about these notes? Leave us feedback
