Ramsay Hunt syndrome
Notes
Overview
Ramsay hunt syndrome refers to the reactivation of herpes zoster in the geniculate ganglion.
The terminology can be confusing. Technically it is Ramsay Hunt syndrome type II (type I is a form of cerebellar degeneration). It can also be referred to as herpes zoster oticus.
It is characterised by a facial nerve palsy associated with a vesicular rash affecting the ipsilateral ear, hard palate and anterior two-thirds of the tongue. Treatment is with antivirals, steroids (+/- gastro-protection) and appropriate eye care.
For our notes on Bell's Palsy (idiopathic facial nerve palsy) click here.
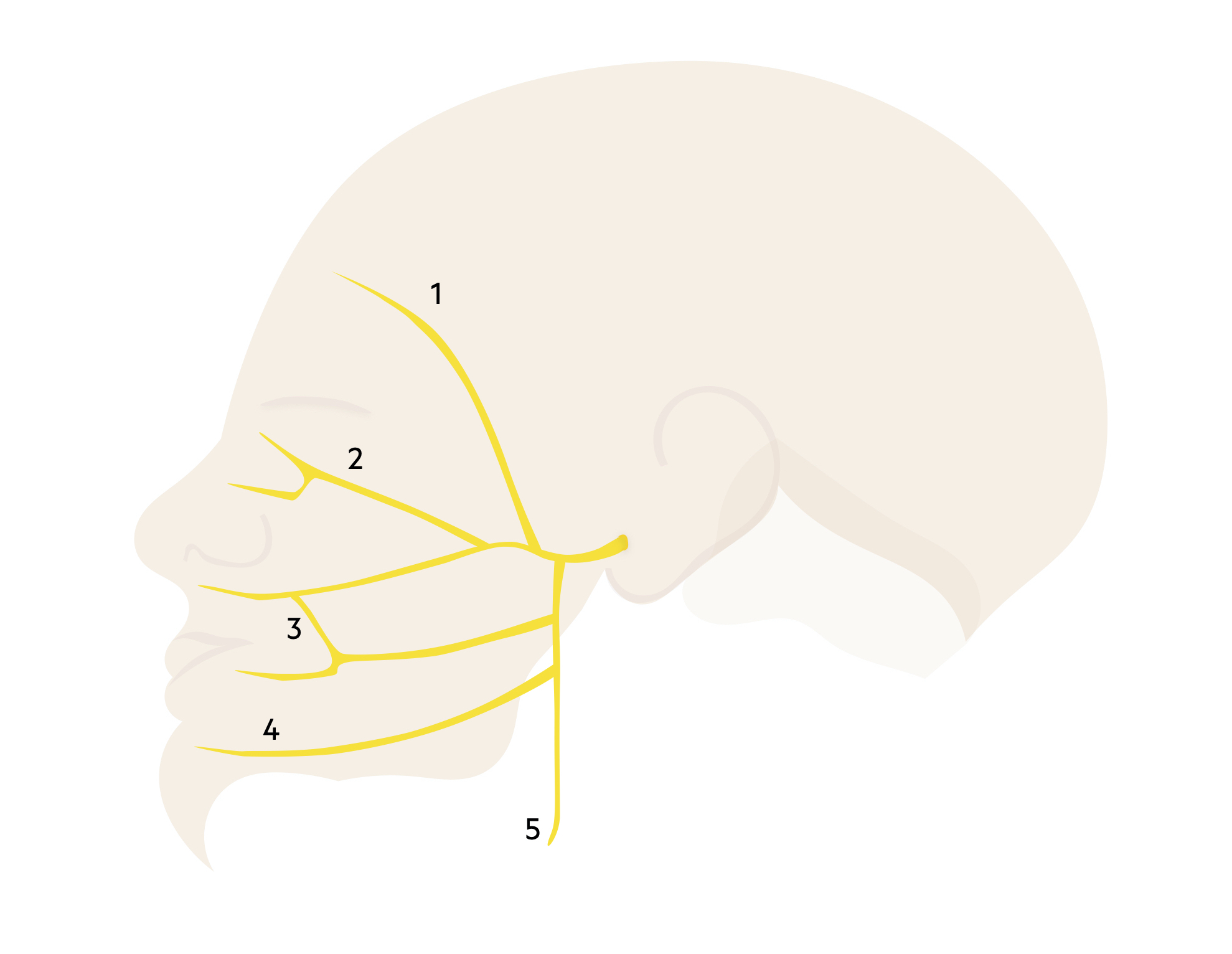
Facial nerve
The facial nerve is divided into five branches, which collectively control the muscles of facial expression.
The facial nerve is the VII cranial nerve. The nucleus is located in the pons, which is part of the brainstem. The nerve root passes through the internal acoustic canal within the temporal bone in close proximity to the inner ear. It then enters the facial canal giving off several branches before exiting the skull via the stylomastoid foramen. It terminates into five terminal motor branches within the parotid gland.
Motor functions
Within the facial canal, the nerve to the stapedius is given off, to supply the stapedius muscle within the inner ear.
The extracranial portion of the facial nerve contains the main motor root. Prior to reaching the parotid gland, three motor branches are given off:
- Posterior auricular nerve
- Nerve to the posterior belly of the digastric muscle
- Nerve to the stylohyoid muscle
The facial nerve terminates within the parotid gland giving off five terminal motor branches:
- Temporal
- Zygomatic
- Buccal
- Mandibular
- Cervical
Parasympathetic functions
- Greater petrosal nerve: arises in the facial canal. Provides parasympathetic supply to the lacrimal gland via the pterygopalatine ganglion.
- Chorda tympani: arises in the facial canal. Provides parasympathetic supply to the submandibular gland and sublingual glands via the submandibular ganglion.
Special sensory functions
- Chorda tympani: provides taste to the anterior two-thirds of the tongue.
Pathophysiology
Ramsay Hunt syndrome results from herpetic inflammation of the geniculate ganglion.
It is caused by reactivation of latent varicella-zoster virus (VZV) within the geniculate ganglion. VZV is one of the human herpesviruses (HHV-3) that cause a spectrum of disease in humans.
The geniculate ganglion is found at the first genu (‘knee’) of the facial nerve and receives input from the facial nerve and nervus intermedius (branch of the facial nerve).
Differential diagnosis
There are many other causes of facial nerve palsy.
Other causes of facial weakness (upper and lower motor neuron - see below) include:
- Bell's palsy (click here)
- Inner ear disease (Otitis media, cholesteatoma)
- Parotid disease (Parotid tumour, parotitis)
- Sarcoidosis (click here)
- Guillain-Barré syndrome (click here)
- Lyme disease
- Trauma
- Stroke (click here)
- Tumours
- Encephalitis
- Meningitis (click here)
- Multiple sclerosis (click here)
- Diabetes mellitus related neuropathy (click here)
Clinical features
The facial nerve palsy in Ramsay Hunt syndrome tends to be more severe than in Bell's palsy.
Symptoms
- Vesicular rash on the ipsilateral ear
- Vesicular rash on the ipsilateral hard palate and anterior two-thirds of the tongue
- Hearing loss
- Ipsilateral facial weakness
- Post-auricular/ear pain
- Difficulty chewing
- Incomplete eye closure
- Drooling
- Tingling (cheek/mouth)
- Hyperacusis (heightened sensitivity to sound)
Signs
- Vesicular rash on the ear
- Loss of nasolabial fold
- Drooping of the eyebrow
- Drooping of the corner of the mouth
- Asymmetrical smile

Vesicles on the ear consistent with Ramsay Hunt syndrome
Image courtesy of Dr. Stephen Reich (CC BY-SA 4.0)
Differentiating upper and lower motor neuron lesions
Peripheral facial nerve palsy is a 'stroke mimic', but it is differentiated from stroke by the absence of ‘forehead sparing’. Facial weakness can be caused by an upper motor neuron (UMN) or lower motor neuron (LMN) lesion. Examples of UMN lesions include stroke and cerebral tumours.
The frontalis muscle, which is supplied by the temporal branch of the facial nerve, has bicortical innervation. This means it receives information from both hemispheres of the cerebral cortex. Therefore, in a UMN lesions leading to unilateral facial weakness, there is ‘forehead sparing’ (i.e. the frontalis can still function). In LMN lesions, the frontalis is affected leading to complete unilateral paralysis.
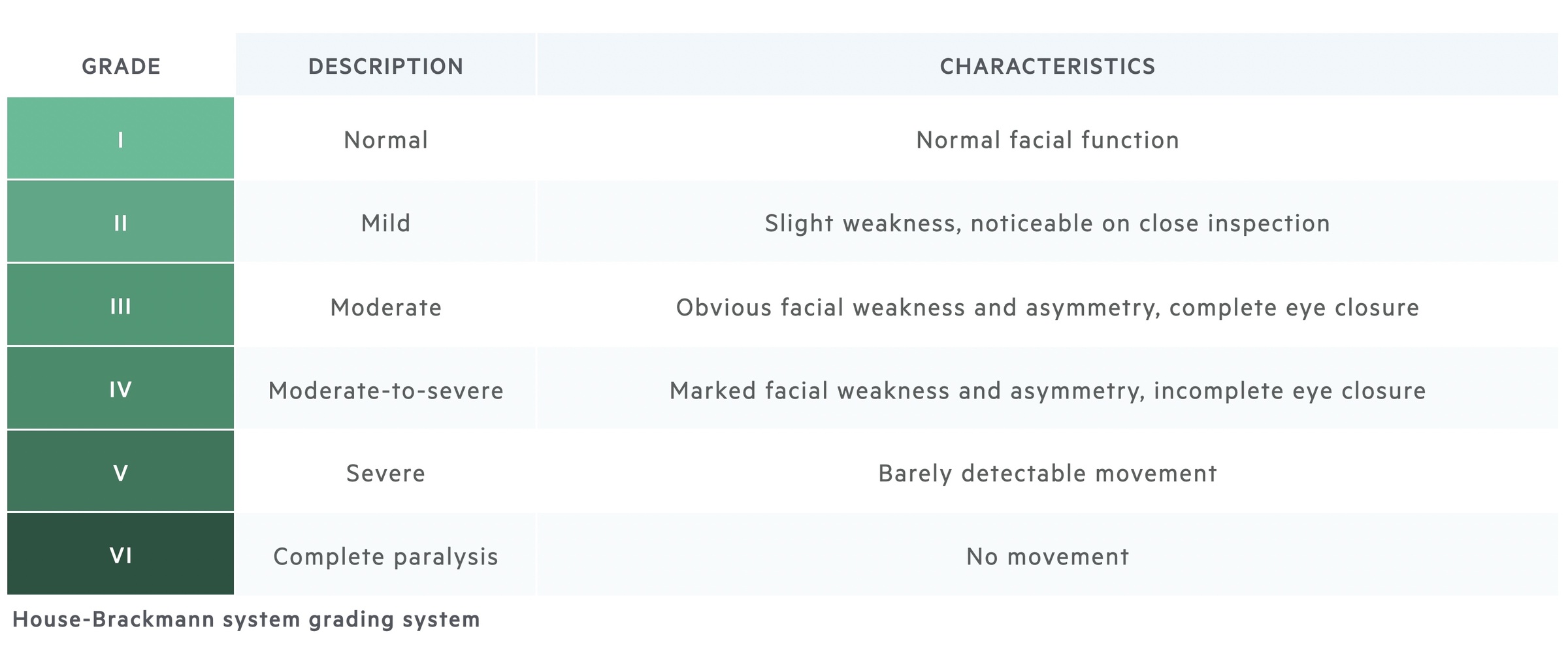
House-Brackmann
Acute facial paralysis can be graded using the House-Brackmann system.
The House-Brackmann system was originally created to assess the degree of facial nerve damage following surgery. It can however be used more generally to grade facial nerve paralysis.
Investigations
Ramsay Hunt syndrome is largely a clinical diagnosis based on facial nerve palsy and characteristically located vesicular rash.
Investigations may include routine blood tests, neuroimaging or specialists tests (e.g. lumbar puncture, Lyme serology) which are considered if alternative diagnoses are felt likely. Strong consideration should be given to sending a blood-borne virus (HIV, Hep B, Hep C) and diabetic (blood sugar, Hba1C) screen. Occasionally a PCR for VZV may be arranged.
When assessing a patient with new-onset facial nerve palsy, it is important to consider alternative causes of facial palsy that may prompt further investigations. Features that point to an alternative diagnosis include:
- Insidious onset +/- progressive
- Systemic illness +/- fever
- Vestibular abnormalities
- Hearing abnormalities (other than hyperacusis)
- Forehead sparing (i.e. suspected UMN lesion)
- Mass
- Recurrent palsy
- Bilateral involvement
Management
Anti-virals, corticosteroids and good eye care are keys to good management.
Treatment early (< 72hrs) with anti-virals and corticosteroids may reduce the incidence of persistent facial nerve palsies and reduce the length of symptoms.
- Analgesia: simple pain relief with paracetamol and NSAIDs (in the absence of contraindications)
- Corticosteroids: typically oral prednisolone, example regime would be 40mg OD for 7 days.
- Anti-virals: typically oral acyclovir, example regime would be 800mg five times a day for 7 days.
Gastroprotection in the form of a PPI is normally given to cover the period of time a patient is taking steroids.
The evidence for anti-viral therapy for Ramsay Hunt syndrome is mixed and limited. A Cochrane review from 2008 found no evidence of benefit but this was based on a single, very small RCT. A Cochrane review at the same time found no RCTs investigating the use of corticosteroids. There is a significantly greater evidence base however in the general use of these treatments for shingles.
There have been numerous papers published since but most compare different anti-virals or combination therapy without any placebo group.
Eyecare
It is critical to provide good eye care - this is somewhat dependent on the severity of the facial nerve palsy.
Treatment includes drops (i.e. lubricating drops and ointments), advice on taping the eye when sleeping and sunglasses outdoors. Any patient with incomplete eye closure (House-Brackmann ≥ IV) should be referred to ophthalmology.
Follow up
Where appropriate, ENT follow-up should be arranged if investigations like an audiogram or tympanogram are indicated.
Last updated: May 2021
Have comments about these notes? Leave us feedback
