Tonsillitis
Notes
Overview
Tonsillitis refers to the acute inflammation of the palatine tonsils secondary to infection.
Acute tonsilitis is very common, especially in children. It is most frequently viral and associated with an upper respiratory tract infection (URTI). It may also be caused by bacteria (e.g. Group A Streptococci).
Management typically involves reassurance, fluids and analgaesia. Where a bacterial cause is suspected, antibiotics +/- steroids are given. The most common complication of acute tonsillitis is a peritonsillar abscess (see Quinsy). Recurrent severe tonsillitis results in considerable morbidity and time lost from school or work.
Clinical features
Clinical examination typically demonstrates enlarged and erythematous tonsils.
Exudate is more uncommon and typically suggests a bacterial pathogen, with Group A beta-haemolytic streptococcus (GABHS) being the most common bacterial cause. The Centor criteria (see chapter below) can be used to estimate the risk of the infection being bacterial in origin.
However, care should be taken to exclude infectious mononucleosis (Epstein-Barr virus), which can also result in exudative tonsilitis. These may be distinguished by lymphadenopathy which should be limited to the anterior chain in a simple bacterial tonsilitis, whilst is more generalised with infectious mononucleosis.

Inflamed tonsils covered in white exudate indicative of streptococcal tonsillitis
Image courtesy of James Heilman, MD and CC BY-SA 3.0
Symptoms
- Fevers
- Sore throat
- Dysphagia
- Trismus (difficulty opening the mouth)
- Malaise
Signs
- Enlarged and inflammed tonsils
- White exudate on tonsils
- Lymphadenopathy

Centor & FeverPAIN
The Centor or FeverPAIN criteria can be used to guide antibiotic use in those presenting with sore throat and tonsillitis.
NICE has produced guidance (NG84) on the use of antibiotics for sore throats and tonsillitis. They advise the use of two scores, Centor and FeverPAIN, to estimate the risk of a streptococcal infection.
Centor criteria
The Centor criteria evaluate the patient for the following:
- Tonsillar exudate
- Tender anterior cervical lymphadenopathy or lymphadenitis
- History of fever (over 38°C)
- Absence of cough
The presence of each is worth one point, with a maximum score of 4. The higher the score the greater the chance the illness is caused by GABHS. A patient with a Centor score of 0-2 is estimated to have a 3 to 17% likelihood of isolating streptococcus. A patient with a score of 3-4 is estimated to have a 32 to 56% likelihood of isolating streptococcus.
FeverPAIN criteria
The FeverPAIN criteria are used as an alternative to the Centor criteria.
- Fever (during previous 24 hours)
- Purulence (pus on tonsils)
- Attend rapidly (within 3 days after onset of symptoms)
- Severely Inflamed tonsils
- No cough or coryza (inflammation of mucus membranes in the nose)
The presence of each is worth one point, with a maximum score of 5. The higher the score the greater the chance the illness is caused by GABHS. A patient with a FeverPAIN score of 0-1 is estimated to have a 13 to 18% likelihood of isolating streptococcus. A patient with a score of 2-3 is estimated to have a 34 to 40% likelihood of isolating streptococcus. A patient with a score of 4-5 is estimated to have a 62 to 65% likelihood of isolating streptococcus.
Management
Management depends on the severity of the tonsillitis and any underlying conditions that may impact the conditions clinical course.
Simple tonsillitis
A common cause of presentation in primary care. Most patients can be managed with antipyretic analgesia (e.g. paracetamol, ibuprofen).
- Unlikely to benefit from antibiotics: those with a Centor score of 0-2 or a FeverPAIN score of 0-1. They should not routinely be offered antibiotics.
- May benefit from antibiotics: those with a FeverPAIN score of 2-3. Many offer a ‘back-up’ prescription that can be used if symptoms persist for longer than 3-5 days.
- Most likely to benefit from antibiotics: those with a Centor score of 3-4 or a FeverPAIN score of 4-5. They will generally be offered antibiotics though the evidence shows minimal overall benefit.
Phenoxymethylpenicillin is the first-choice antibiotic, clarithromycin or erythromycin may be used in those with penicillin allergy. Consider a lower threshold for antibiotics in patients at increased risk of rheumatic fever.
Appropriate safety netting must be given to all patients with advice to return if symptoms persist, worsen or there are other concerns.
Severe tonsillitis
Symptoms may be severe with dysphagia and high fevers. Some patients benefit from IV fluid, antibiotics and a dose of IV steroids. If severe they may be admitted overnight for observation and reassessed after 12-24 hours of IV therapy.
Note: In patients presenting with any of a severe sore throat, drooling, stridor or trismus – epiglottitis – a rare but potentially life-threatening condition should be considered.
Special cases
Additional care is required in certain patient groups at increased risk of severe infections.
- At risk of agranulocytosis (e.g. taking carbimazole): hold medication, send FBC and seek specialist advice.
- Immunosuppressed patients: may be due to an illness (e.g. haematological malignancy, HIV/AIDS) or due to medications (e.g. chemotherapy, immunosuppressants post-transplant). Complete a clinical review and seek specialist advice.
Complications
Complications are relatively rare but may be seen in bacterial tonsillitis.
GABHS can be associated with complications, these may be suppurative (pus producing) or non-suppurative.
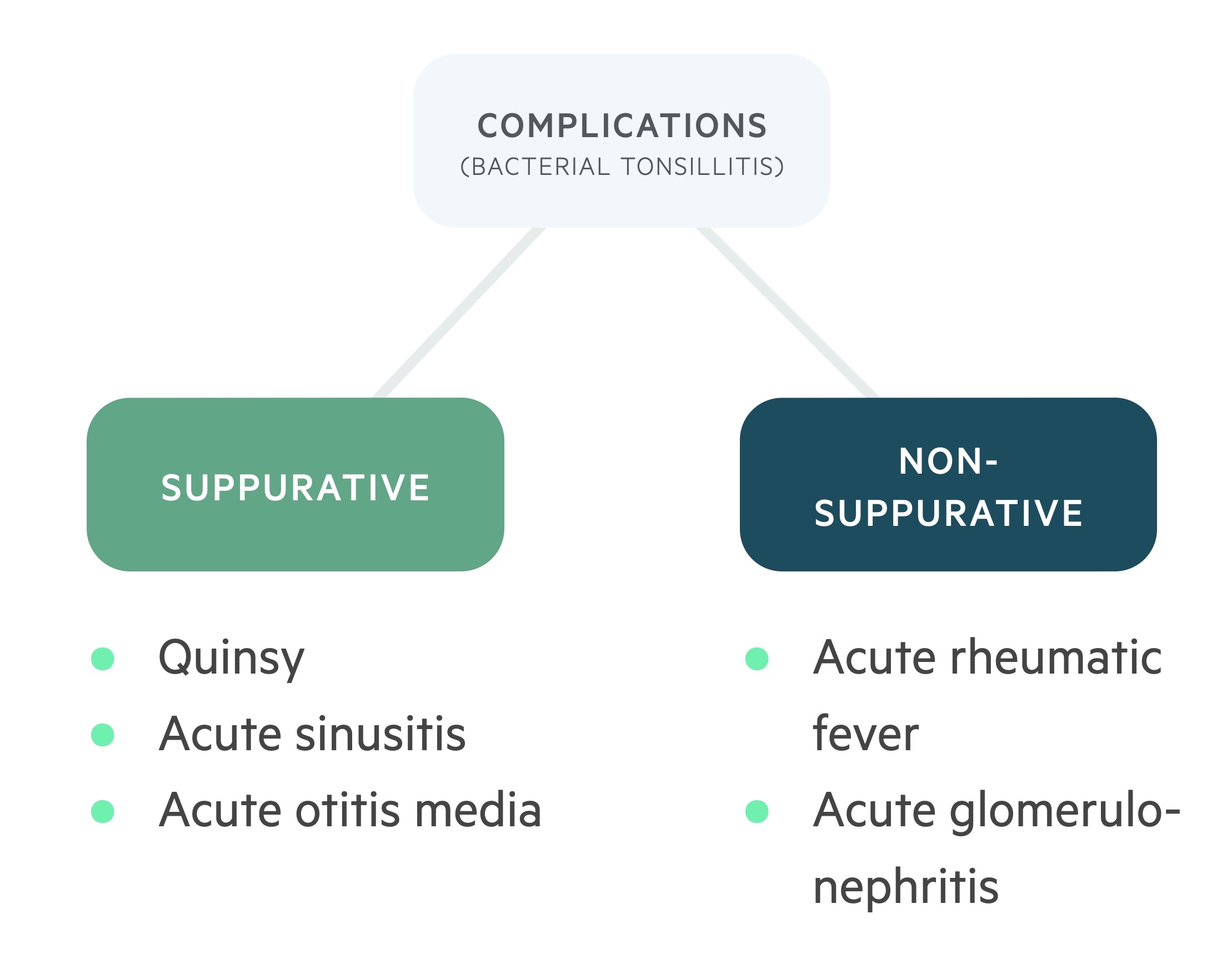
Suppurative
- Quinsy (peri-tonsillar abscess)
- Acute otitis media
- Acute sinusitis
Non-suppurative
- Post-streptococcal glomerulonephritis
- Acute rheumatic fever
Tonsillectomy
The NHS sets specific criteria that should be met for tonsillectomy to be considered.
The NHS will normally fund tonsillectomy where:
- Malignancy is suspected
- More than one episode of quinsy or airway obstruction
- Recurrent sore throat with disabling episodes preventing normal function, due to tonsillitis (seven or more eligible episodes in the last year or five or more in each of the last two years or three or more in each of the preceding three years)
- Obstructive sleep apnea
As always these criteria do not overrule clinical judgement and a holistic view of each patient and their presentation must be considered.
Note: Eligible episodes must score 3 or 4 in the Centor criteria.
Additionally, in children tonsillectomy (+/- adenoidectomy) may be considered where there is:
- Failure to thrive
- Sleep apnoea
- Significant impact on quality of life
Last updated: March 2021
Have comments about these notes? Leave us feedback
